Article Topic: Cerebral edema
Author: Areen Amaireh
Keywords: Brain Edema, Swelling, Cerebral Edema, ICP
Scientific Editor: Marah Bassam Akhdar
Definition
Cerebral edema is the accumulation of extreme quantities of fluid within the brain parenchyma [1]. It can be caused by brain damage because of several potential reasons, such as ischemic or hemorrhagic strokes, brain traumas, infections, or tumors. Brain edema causes weakened nerve function, increased intracranial pressure (ICP), leading eventually to unconsciousness and herniation [3]. Cerebral edema could cause an irreversible injury [2]. The herniation results in direct stress on the brain tissue and compresses the vessels which leads to further ischemia and, later on, death [3].
The edematous brain is softer than a normal brain. It often appears to overfill the cranial cavity. In brain edema, the surfaces of the gyri are flattened due to compression of the expanding brain by the dura mater and the inner surface of the skull. Such changes result in a dangerous increase in intracranial pressure [1]. There are two types of brain edema [1]:
1-Vasogenic edema.
2-Cytotoxic edema.
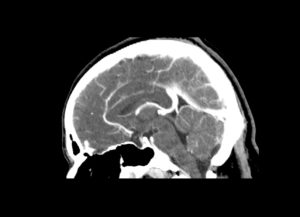
Figure (1): Cerebral edema Case courtesy of Dr Orsolya Lajos [4].
Vasogenic edema
Vasogenic edema occurs when the integrity of the normal blood-brain barrier (BBB) is disrupted [1]. This disruption involves the breakdown of the tight endothelial junctions comprising the blood-brain barrier following a physical disruption or a release of vasoactive compounds [5]. The blood-brain barrier is formed by astrocytes and pericytes joined together, along with adhesive proteins producing tight junctions [6]. As a result, intravascular proteins and fluid move from the vascular area into the extracellular compartment of the brain [5].
This type of edema can be localized in a specific area or generalized in a wider area [1]. Accumulation of extracellular fluid increases the brain volume and intracranial pressure (ICP) causing the symptoms of cerebral/brain edema [6].The white matter is greatly affected because of its reduced density with multiple unconnected parallel axonal tracts [5]. Vasogenic edema is seen extensively around brain tumors and cerebral abscesses. However, some vasogenic edema may be seen around maturing cerebral contusion and brain hemorrhage [7].

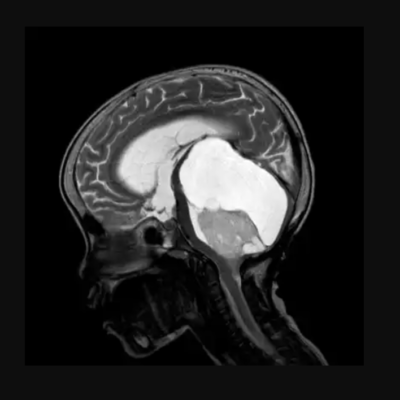
Figure (2): Intraparenchymal hematoma and vasogenic edema in the left parieto-occipital lobe [8].
Cytotoxic edema
Cytotoxic edema is an increase in intracellular fluid secondary to neuronal and glial cell damage. It might occur following generalized hypoxic or ischemic insult or exposure to specific toxins [1]. In other words, it is a type of brain edema that is most commonly seen in cerebral ischemia in which extracellular water passes into cells resulting in swelling [9].
Cytotoxic edema results from a disruption in adenosine triphosphate (ATP)-dependent transmembrane sodium-potassium and calcium pumps. It is usually caused by brain ischemia or excitotoxic brain injury [5]. Attrition of energy sources reduces the activity of the sodium-potassium pump in the cell membrane leading to cellular retention of sodium ions [6]. This leads to intracellular accumulation of fluid in neurons, axons, glial cells, and myelin sheaths. The gray matter will be affected first due to its high metabolic activity and greater astrocyte density. Eventually, both the gray and white matters will be involved. There is an overall limitation of diffusion of water molecules across the cell membrane and within the cytoplasm. Initially, the blood-brain barrier (BBB) remains unchanged or intact and extracellular water does not increase. Nonetheless, intense or repeated insults overwhelm the transmembrane ion pumps which leads to cell death with the breakdown of the blood-brain barrier causing vasogenic edema [5]. Subsequent complications include neuronal apoptosis, atrophy, and gliosis [5]. However, the definitive consequence of cytotoxic edema is the oncotic death of neurons [6].
Etiology and Symptoms
Brain swelling is a life-threatening condition that develops because of an inflammatory reaction. Most frequently, this is the result of cerebral trauma, severe cerebral infarction, hemorrhages, abscess, tumor, allergy, sepsis, hypoxia, and other toxic or metabolic factors [10]. Symptoms of brain edema are nonspecific [5]. Additionally, its severity depends on the exact cause but it is generally related to an acute increase in the pressure within the skull.
Increased pressure within the skull can lead to a compensatory elevation of blood pressure to preserve cerebral blood flow [6]. Symptoms of brain edema include: Headache, nausea, loss of coordination, seizures, lethargy, memory loss, and reduced level of consciousness [11]. Also, symptoms are frequently accompanied by visual problems and vertigo [6].
Pathophysiology
For cerebral edema and swelling to occur, brain tissue must be supplied by an external fluid source [12]. The pathophysiology of cerebral edema/swelling at the cellular level is complex. Injured cells swell, damaged blood vessels leak and absorption pathways stop thus forcing the fluid to shift into the brain tissues [13]. The hydrostatic force produced by the mass effect of ion transport and the osmotic force produced by the derangements in ion transport drives the bulk flow of edema [12].
Cellular and blood vessel damage leads to an activation of an injury cascade. The cascade begins with releasing glutamate into the extracellular compartment. Calcium (Ca) and sodium (Na) entry channels on cell membranes are opened by glutamate stimulation. Membrane ATPase pumps extrude one calcium ion in exchange for three sodium ions. Sodium builds up within the cell making an osmotic gradient and rising cell volume by water influx. An increase in fluid causes cell swelling and dysfunction but not necessarily permanent or irregular damage. Finally, hypoxia consumes the cells’ energy stores weakening the sodium–potassium ATPase and decreasing calcium exchange [13].
Pathogenesis
Brain edema is created by an increasing buildup of intracerebral water and represents a brain reaction against most injuries. The volume of the brain parenchyma enlarges to the detriment of the other two intracranial components: Blood and the cerebrospinal fluid (CSF) which causes changes in the ratios between intracranial volume and intracranial pressure [14].
Several mediators have been identified to play a role in edema formation after traumatic brain injury (TBI). Probably, the most exciting recent developments include the identification of aquaporin water channels as critical participants in the formation of brain edema, and the focus on agents that affect the blood-brain barrier (BBB); and therefore, the vascular contribution to brain swelling. These mediators are Aquaporins, vasoactive agents, and matrix metalloproteinases [15].
The development of cerebral edema occurs in two stages. It begins with the disturbance of the glioneuronal metabolic circuits by changing the transport mechanisms. Then, extension and expansion – when the specified features of cellular/extracellular injury is defined and developed by covering wide areas of the brain tissue [14].
Edema is hazardous because it causes cell swelling. This swelling alters cellular metabolite concentration and thus cellular physiology, and biochemistry which results in abnormal function. When the swelling involves not only the cells themselves but also the brain parenchyma, there is a fast increase in intracranial pressure (ICP), which causes a compression of blood vessels, minimized tissue blood flow, decreased oxygenation and later tissue shift down pressure gradients (herniation) that may suppress vital brain centers such as centers responsible for respiration and cardiac function [15].
Epidemiology
Since cerebral edema is not an easily determined simple disease but a different continuum created by several causes and presents in combination with some other common cerebral pathologies, the epidemiology of this disorder is not easily defined [3,6]. The incidence of brain edema should be considered in terms of its potential etiology. Cerebral edema presents in most cases of traumatic brain injury (TBI), central nervous system tumors, brain ischemia, and intracerebral hemorrhage/bleeding [6].