Article Topic: Chiari Type I Malformation
Author: Marah Bassam Akhdar
Keywords: Chiari Type I Malformation, Tonsillar Ectopia, Hydrocephalus, Neural Tube Defect, Posterior Fossa Anomalies
Scientific editor: Dr.Omar Jbara
Linguistic editor: Philip Sweidan
Congenital Malformations & Perinatal Brain Injury
Central Nervous System Malformations giving rise to mental retardation, cerebral palsy, neural tube defects and posterior fossa anomalies have an incidence rate of 1%-2%. Perinatal insults, brain injuries, genetic, and environmental factors interfering with normal central nervous system development could result in various birth defects [1].
Posterior Fossa Anomalies
The most common manifestations of posterior fossa anomalies include the displacement or partial/complete agenesis of portions of the cerebellum [1]. One of these anomalies is Chiari Type I Malformation.
Introduction
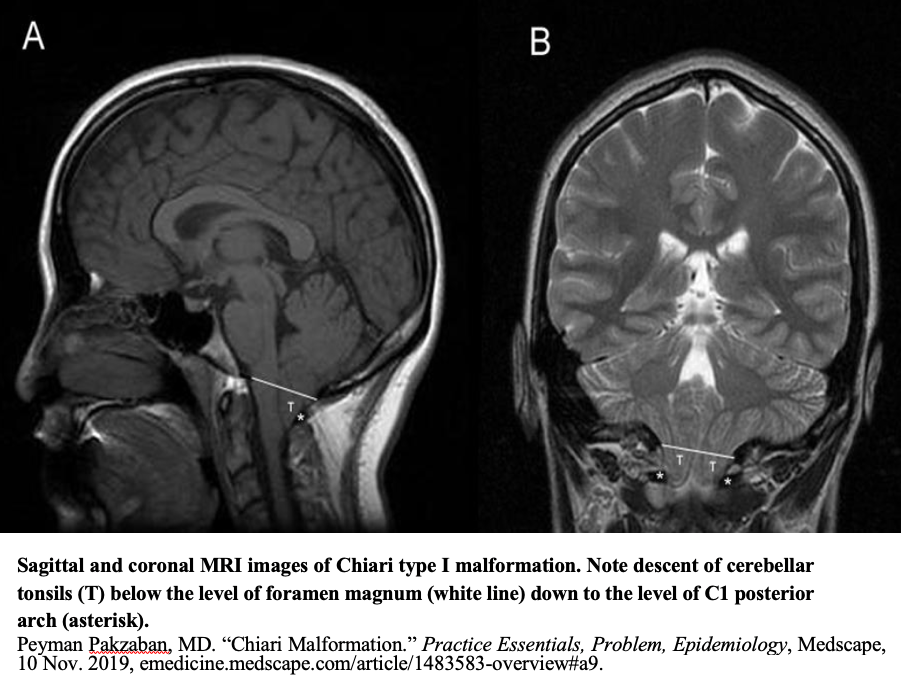
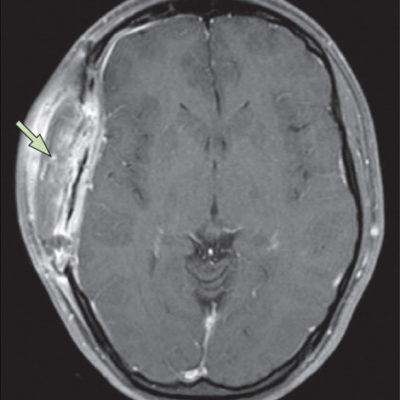
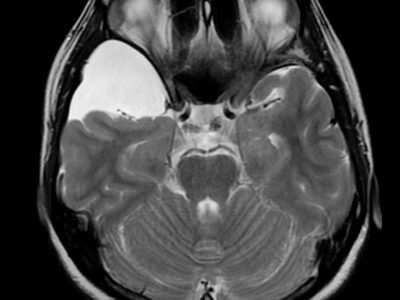
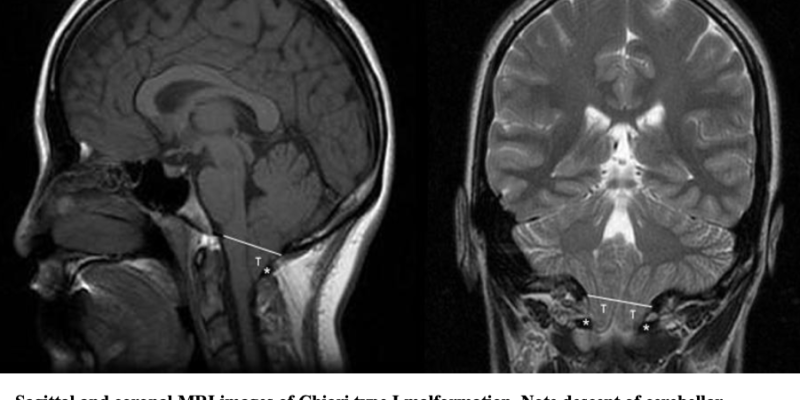
Among Chiari Malformations, Chiari Type I Malformation is the least severe and most common variant on the spectrum. It manifests itself during late childhood and adulthood [2]. Chiari Type I Malformation is characterized by tonsillar ectopia which is the caudal descent of cerebellar tonsils below the level of the foramen magnum. The clinical syndrome is produced due to the impaction of the foramen magnum, cervicomedullary junction compression by tonsillar ectopia and cerebrospinal fluid flow interruption [3].
The definition of Chiari Type I Malformation is highly controversial as there is no universally accepted definition among scientists. The Chiari Type I Malformation shows incongruity in radiological findings [4]. As a result, some authors have proposed to term Chiari Type I Malformation as ‘Chiari Syndrome’ and denote ‘Chiari Malformation’ for types II-IV. The alternative term would clearly point out the distinct etiology, pathophysiology, radiology, and clinical features of Chiari Type I [5].
History
The Austrian pathologist Hans Chiari described Chiari Type I Malformation as the herniation of cerebellar tonsils passing through the foramen magnum [6].
This description often involved further anatomical variations of the skull and central nervous system [6,7]. Various theories were proposed to justify the underlying mechanism for hindbrain herniation [8]. The nomenclature of Hans Chiari described asymmetrical tonsillar ectopia; however, it lacked a quantifiable amount of tissue herniation [9]. In 1985, Aboulezz et al. proposed that cerebellar herniation could be up to 3 mm below the foramen magnum [10]. Later, Barkovich et al. posited that a 3mm herniation is the minimal cut off for Chiari Type I [11], although an inferior cutoff of 5mm herniation is widely accepted [12].
Etiology
Although the genetics of Chiari Type I Malformation still needs further confirmation [13], a familial aggregation analysis suggests genetic basis for the disease [14, 15]. Recent studies have proposed links to chromosomes 2, 9, 14 and 15 [14, 16, 17]. There is a hypothesis that Chiari Type I originated as a paraxial mesoderm disorder resulting in the formation of a small posterior fossa. The formation of a hypoplastic posterior fossa causes cerebellar compression, cerebellar tonsillar herniation, and foramen magnum impaction. This hypothesis is consistent with suggested associations of Chiari Type I Malformation and other congenital mesodermal connective tissue disorders: for example, Ehlers- Danlos Syndrome [18].
Moreover, secondary conditions including craniocerebral disproportion, craniosynostosis, secondary neurulation abnormalities, platybasia, and bone metabolic disorders could be a leading cause of Chiari Type I Malformation. A pressure build-up due to hydrocephalus or tumor growth could also result in Chiari Type I Malformation. This type of malformation could be iatrogenic due to lumboperitoneal shunt used for idiopathic intracranial hypertension treatment [19]. Chiari Type I may be rarely but possibly caused by an injury. Another possibility for the etiology of Chiari Type I could be a tethered cord at the sacrum. A caudal traction could pull on the bone marrow and brainstem structures causing the descent of cerebellar tonsils and in turn Chiari Type I Malformation [20].
Epidemiology
Chiari Type I Malformation is the most common type of Chiari Malformations. The prevalence of Chiari Type I Malformation is approximately 1in 1000 births. Among adults a female predominance of 3:1 has been established in comparison to children where the disease does not appear to be related to sex [21].
It has also been observed that differences in the prevalence of Chiari Type I Malformation in various ethnicities may be due to ethnic variations in posterior fossa size and cerebrospinal fluid flow [22, 23, 24].
It is also remarkable to mention that the epidemiological data is underestimated due to late manifestation of the disease and high rates of asymptomatic patients [2].
Pathogenesis/Pathophysiology
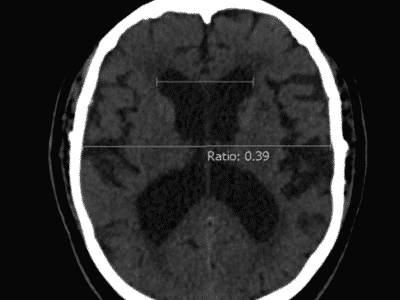
The classification of Chiari Malformations is based upon the morphology. Chiari Type I Malformation presents with >5 mm caudal descent of the cerebellar tonsils below the foramen magnum [25].
Generally, the pathogenesis leading to Chiari Type I Malformation can be categorized into four groups: (1) Structural anomalies of the skull base, (2) abnormal segmentation of cervical vertebral bodies, (3) overcrowding due to small posterior fossa and/or cranial vault, and (4) presence of excessive tissue in the posterior fossa or cranial vault [26].
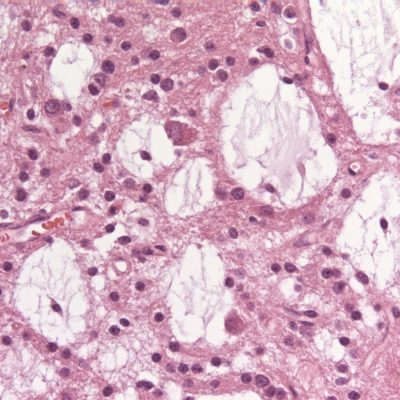
Chiari Type I Malformation causes cerebrospinal fluid outflow obstruction and neurological dysfunction by direct compression of neural tissue at the craniovertebral junction. Obstruction of cerebrospinal fluid outflow could lead to progressive formation of secondary hydrocephalus or syringomyelia which is found in around 65-75% of Chiari Type I Malformation cases [27].
Tonsillar ectopia is regarded as an incidental neuroradiological finding, meaning that not all cases of Chiari Malformation Type I detected on imaging are symptomatic. Additionally, the severity of the disease does not correlate with the degree of herniation as cases with prominent herniation could also be asymptomatic [28, 29]. As previously mentioned, the manifestation usually presents in adulthood in the third-fifth decades of age [30, 31].
Chiari Malformation Type I presents in all ethnicities, with slight female predominance in adults which is believed to be due to hormonal status or genetic variants affecting disease susceptibility and progression. There is no sex predominance of the disease in pediatric cases suggesting a different etiology between adults and pediatrics [30, 32, 33].
The genetics of Chiari Type I Malformation are thought to be multigenic that involve genes that influence the morphology of cranial base and craniocervical junction, cerebellar size, cerebrospinal fluid production, and absorption. Recent studies suggest the whole exome sequencing on large cohorts of Chiari Type I Malformation patients has great potential to improve the understanding of Chiari Type I Malformation pathogenesis [34].
Chiari Type I Malformation patients are mostly asymptomatic; nonetheless, the main symptom to manifest in both adults and children is pain or tussive headache in the occipital/cervical region [35]. Headaches in Chiari Type I Malformation could be exacerbated with Valsalva maneuver as a result of small foramen magnum. Clinical features may include syncopal episodes and sinus bradycardia due to autonomic dysfunction, swallowing alterations and vomiting due to glossopharyngeal and vagus nerves involvement resulting in an absent gag reflex, balance difficulties resulting in unsteady gait, hand coordination difficulties, tingling and numbness in extremities due to sensorial manifestations, dizziness, tinnitus, progressive muscular weakness in the arms and legs, and stiffness in the back, shoulders, arms, or legs, acute paraparesis, etc. [35,36,37,38,39,40,41].
Prognosis
For the majority of patients, the prognosis is good. However, thorough and appropriate investigations should be performed to determine the appropriate treatment approach (medical/ surgical). 73% of patients show favorable surgical outcomes in less than one year post surgery. In addition, 79% improve at the one to three years follow-up postoperatively [2,42].
Management
Management options for Chiari Type I Malformation are rather empirical due to the lack of clear agreement upon a precise algorithm. Medical and surgical approaches have provided a degree of relief for symptomatic patients of Chiari Type I Malformation [2].
Symptomatic patients that present with headaches or neck pain could be prescribed with physical support collars, muscle relaxants, and non-steroidal anti-inflammatory drugs (NSAIDS) to relief the pain. Nonetheless, less common symptoms including gait disturbance are minimally affected by the above mentioned options. Recent proposals have suggested meditation or yoga therapy as forms to address the pain[2].
Chiari Type I Malformation patients who present with severe symptoms as well as confirmed cerebellar ectopia on imaging and cerebrospinal fluid (CSF) obstruction on cine MRI are typically offered surgical interventions. Posterior Fossa Decompression (PFD) is the most adopted neurosurgical approach that focuses on decompressing the cervicomedullary junction thus restoring cerebrospinal fluid (CSF) flow. The surgery involves a suboccipital craniectomy and laminectomy at the level of C1 posterior arch [43]. In some cases, duraplasty during Posterior Fossa Decompression (PFDD) is performed. The latter is determined intraoperatively using cine MRI [46]. Posterior Fossa Decompression (PFD) is performed in 99% of the literature [44].
To address Chiari Type I Malformation with syringomyelia, surgeons perform a sub meningeal cerebellar tonsillar herniation resection and cisterna magna reconstruction without craniectomy [45]. Several studies have proposed the syringomyelia decompression by distal drainage using a syringosubarachnoid shunt [47]. The latter are considered minimally invasive approaches to manage Chiari Type I with syringomyelia.
Latest Advancements in Management
Numerous research studies are being conducted to find the most efficacious Chiari Type I Malformation management strategies.
Recent studies revealed that performing Posterior Fossa Decompression (PFD) without duraplasty does not achieve the needed outcomes. Today, the most favorable approach is Posterior Fossa Decompression with Duraplasty (PFDD). Additionally, some studies do not recommend tonsillar resection due to elevated risk of side effects. Other studies show that using a shunt increases the size of cavities [48].
Further investigations should be performed to establish a unified algorithm for the management of Chiari Type I Malformation.