Title: Epidural Abscesses
Author: Dana Alshawabkeh
Editor: Rahmeh Adel
Reviewer: Ethar Hazaimeh
Keywords: epidural abscess, intracranial abscess, spinal abscess, brain abscess
Abbreviations:
ICEA=Intracranial Epidural Abscess, SEA= Spinal Epidural Abscess, ESR= Erythrocyte Sedimentation Rate, CSF= CerebroSpinal Fluid, MRI= Magnetic Resonance Imaging, CT= Computerized Tomography.
Abstract
Epidural abscess is an infection within epidural space anywhere in the brain or spinal cord.5 It is a serious, potentially life-threatening central nervous system infection involving the intracranial or spinal compartments.1
Intracranial epidural abscesses (ICEAs) are uncommon lesions, being more frequent in older children and adults, they commonly result from direct extension of a pre-existing infection and rarely present with the focal deficit.2
Spinal epidural abscess (SEA) is a rare condition that occurs most commonly in adults in their fifth and sixth decades of age.21 Despite advances in diagnostic medicine, early recognition of SEAs remains difficult.3 Delay in early diagnosis may be related to increased morbidity and mortality,6 wherefores once SEA was diagnosed in the patients, immediate treatment has to be initiated for all SEA patients.7
Overview
The sites of spinal epidural abscesses are variable. Only 20% occur anterior to the spinal cord. Abscesses in the cervical or upper thoracic region are not uncommon, the preponderance of lower thoracic and lumbar abscesses. Patients with a lumbar abscess may be misdiagnosed as having a herniated lumbar disc.27
So, in this article, we will discuss diagnosis epidemiology, risk factors, pathogenesis, clinical presentation, diagnosis, complications, and treatment of an epidural abscess.
Epidemiology
SEA is nine-time more common than ICEA and more likely to be acute. Although ICEA is not common, still the third most common focal pyogenic intracranial infection, after brain abscess and subdural empyema.9
The incidence of SEA is 0.2 to 1.2 cases per 10,000 hospital admissions 9 and the ratio of male to female is about [1: 0·56], which is associated with the higher prevalence of risk factors in men and boys and mortality rate from about 6% to 32%.5
SEAs are more prevalent in 30-year-old patients and older. However, they can affect younger people, even young children.5
The ICEA complications are more in children, adolescents, and young adults (7–20 years of age).5
Risk factors
Intracranial Epidural Abscess (ICEA)
The most common risk factors for ICEAs include frontal sinus infection, post-traumatic infection, recent intracranial, transnasal, or transmastoid surgical procedures, and congenital defects in the bone of the anterior cranial fossa which facilitate communication between the intracranial epidural space and the paranasal sinuses.5
Spinal Epidural Abscess (SEA)
Non-spinal infections were the most common cause of SEAs. Among them, the paravertebral abscess was the most cause, then skin and soft tissue abscesses. Additional risk factors include spinal procedures such as epidural injection for pain control, acupuncture treatment, and previous spine surgery after spinal trauma. Risk Factors such as diabetes mellitus, liver disease, and cancer were also found (Table 1).7
There are other risk factors including penetrating injury to the spine, class III obesity, primary or iatrogenic immunosuppression, skin infections or abscesses, and transient bacteremia.5 The organism was identified in 84% of cases, most commonly Staphylococcus aureus.8

Table 1: Associated predisposing factors of SEAs.7
Etiology and pathogenesis
ICEA
Streptococci (usually anaerobe forms like Peptostreptococcus) and other anaerobes such as Cutibacterium (part of the skin flora) are usually the causing organisms. Gram-negative bacilli or fungi can be a cause as well. They generally originate in the sinuses.
ICEA generally starts with an exogenous port of entry, either the paranasal sinuses or ears and can be a complication of neurosurgery. Also, the infection can spread inward from osteomyelitis of the skull or fetal monitoring probes applied to the cranium during birth.9
SEA
The infection enters the spinal epidural space by some 4 mechanisms:20
- Hematogenous spread from an existing infection is the most common mechanism.
- Through direct extension.
- Inoculation via spinal procedures.
- Trauma.
Hematogenous SEAs are primarily located in the posterior aspect of the spinal canal.27 The second most common mechanism of infection is direct spread from an infected element of the vertebral column or paraspinal soft tissues. Most commonly, this takes the form of anterior SEAs in association with vertebral body osteomyelitis.20
Septic arthritis of a facet joint can cause a secondary infection of the posterior epidural space. Direct spread from other posterior structures such as retropharyngeal, psoas, or paraspinal muscle abscess may cause SEAs as well.20
Less frequent mechanisms include direct inoculation and trauma. Infection of the epidural space can occur in conjunction with spinal surgery, placement of an epidural catheter, or spinal injections. Hematoma secondary to an osseous or ligamentous injury can become seeded by bacteria, causing abscess formation.20
Clinical presentation
ICEA
The clinical presentation of brain abscess relies on the lesion’s size and anatomic location, the causative pathogen’s virulence, the host’s immune status, and the presence of underlying systemic conditions.1 Symptoms of ICEAs may include nausea, vomiting, fever, and headache. Neurologic deficits are common, but not always present.24
SEA
SEA should be suspected in the patient presenting with complaints of back pain or a neurologic deficit in association with fever or an elevated erythrocyte sedimentation rate.22
The typical features of spinal epidural abscess are recognizable clinically.27 The classic triad of clinical manifestations of SEA includes localized back pain, progressive neurologic deficit, and fever.18
It occurred in only a minority of patients (37%). However, the coexistence of axial back pain and progressive neurologic symptoms remained the most reliable clinical indicator for the presence of SEA.12
Diagnosis
Imaging findings
Any patient presenting with purulent otorhinogenic, sinus, or dental infections with encephalopathy or focal neurologic deficits must undergo brain imaging with contrast.1
Plain radiographs are ineffective and lack specificity and sensitivity in diagnosing SEAs.5 If there is a concern for SEAs, patients should undergo an immediate MRI of the whole spine. If MRI is not available, CT with IV contrast is a less sensitive alternative. Lumbar puncture is not necessary as it lends little diagnostic utility and has potential morbidity in the setting of spinal epidural abscess.13
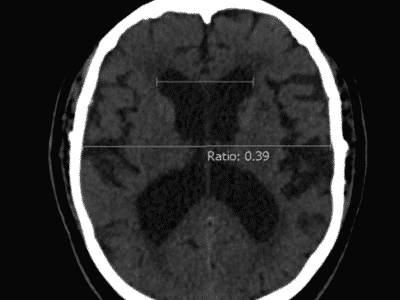
CT scan
CT is less sensitive for detecting an epidural abscess than MRI is. Features of epidural abscess on CT include extra-axial location, isodense or hypodense to surrounding brain, biconvex shape, usually does not cross suture lines, may cross the midline, and strong peripheral enhancement with contrast.25
MRI
ICEAs
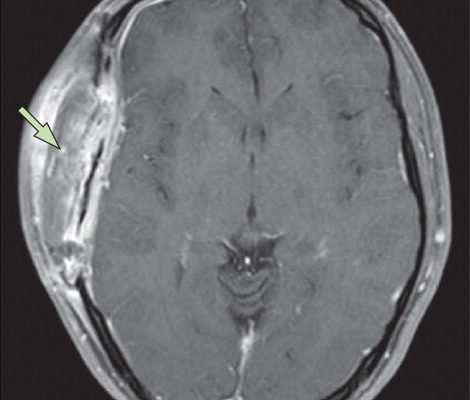
Characteristics of ICEAs on MRI include:25 (as shown in figure 1)
- T1: hyperintense
- T1 C+ (Gd): strong peripheral contrast enhancement
- T2/FLAIR: isointense or hyperintense
- PD: isointense or hyperintense
- DWI: area of restricted diffusion
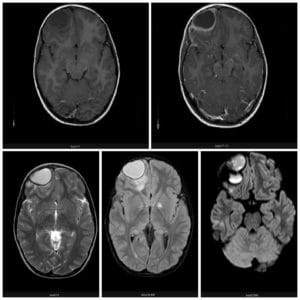
Figure 1. MRI shows the multiloculate morphology of the intracranial epidural collection located in the right supraorbital region. The collection is hypointense on T1-weighted and hyperintense on T2-weighted images, with a surrounding membrane that enhances with contrast administration.25
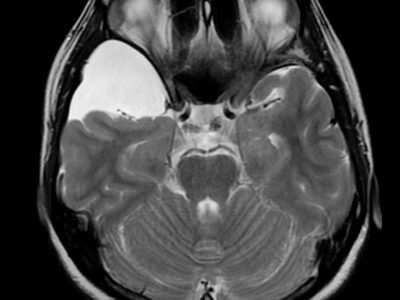
SEAs
Gadolinium-enhanced MRI is the imaging option for the diagnosis of spinal epidural infection. Diffusion-weighted sequences are helpful to confirm the condition.
There are two main manners, with distinct imaging appearances:
- Phlegmonous stage of infection results in a homogeneous enhancement of the abnormal area which correlates to granulomatous-thickened tissue with embedded micro-abscess without a significant pus collection.
- Liquid abscess surrounded by inflammatory tissue shows a varying degree of peripheral enhancement with gadolinium.
The key to relating liquid abscesses, which is usually a sufficient cause for surgical drainage, is the presence of a region of high T2 signal, with low T1 signal and without enhancement, usually surrounded by an edge of enhancement (as shown in figure 2). DWI/ADC commonly demonstrates limited diffusion of the abscesses content.26
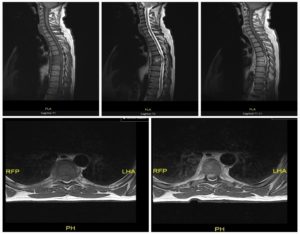
Figure 2.
Changing signal and avid enhancement of the T6 and T7 vertebral bodies and intervening discs. Epidural abscess, canal stenosis, and thoracic cord compression at T6/T7 level. L4/L5/S1 degenerative change.26
Laboratory Findings
Sensitive tests such as (ESR) and (CRP) can help guide more investigation of epidural abscesses in such patients.19
In ICEA serum inflammatory markers, including (ESR) and (CRP) may be elevated. In one study, 73 of 90 patients (81%) had an elevated ESR and 23 of 25 patients (92%) had a raised CRP.1,14 Elevated markers of inflammation, although nonspecific, raise the degree of suspicion for infection, while normal measures do not rule out the presence of a brain abscess.17 The presence of peripheral leucocytosis is highly variable but can be seen in 50% or more of cases.15
Lab evaluation for SEAs should include blood cultures, complete blood count, inflammatory markers, and coagulation studies. Although the ESR is often elevated in these patients, it does not rule out the diagnosis of a spinal epidural abscess (85% to 94% sensitivity). Positive cultures are found in 90% of abscess aspirates, 62% of blood specimens, and 19% of CSF specimens.13
The presence of leucocytosis is not sensitive nor specific for the diagnosis. While an elevated ESR and CRP are sensitive, they are not disease-specific. Blood cultures are positive in almost 60% of SEAs.18
Histopathology
Blood cultures define the organisms and histopathology of SEAs. Staph aureus accounts for over 60% of the SEA. Polymicrobial SEAs are a rarity and blood cultures are positive in most patients.
This situation differs from that of IEAs in which blood cultures are positive in only 10% of patients; and even if positive, they do not represent the actual causative organism. Brain abscess pus often grows mixed organisms.28
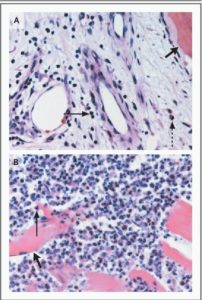
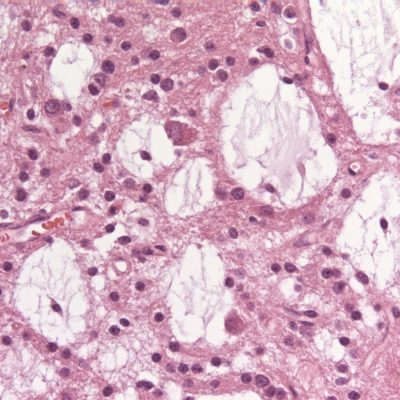
Figure 3.
Histopathological Findings in patients with SEAs.
Panel A, H&E stained vertebral-bone biopsy in chronic vertebral osteomyelitis that led to a SEA, shows chronic inflammatory cells, including lymphocytes (arrow) and plasma cells (dashed thin arrow) in the vicinity of trabecular bone (thick arrow).
Panel B, the spread of infection from the epidural space resulted in the formation of an acute psoas muscle abscess, and the infiltration of PMN cells (thin arrow) adjacent to striated muscle fibers (thick arrow) 16
Complications
Complications of SEAs include meningitis or subdural infection if the needle traverses the epidural abscess, sepsis, neurologic deterioration if the lumbar puncture is performed below a complete spinal subarachnoid block, and irreversible paralysis which is the most fearsome complication of spinal epidural abscess and continues to affect 4 to 22% of patients.16
ICEA has a 10% mortality rate and may result in long-term neurologic deficits.24
Treatment and Management
The treatment of choice is usually urgent surgical debridement in combination with intravenous antibiotics.8 SEA may be treated without surgery in cautiously selected patients.20 Few studies have reported similar outcomes in patients who were treated with antibiotics alone and in patients who received both medical and surgical treatment.16 The findings of blood cultures or CT-guided needle aspiration of the abscess must guide antibiotic treatment.16
ICEAs
ICEAs treatment usually requires a combination of a drainage procedure and antibiotic therapy, like most abscesses.
Physicians should choose antibiotics for Streptococcus, Hemophilus, and anaerobes to cover infections that have spread from the ear, sinuses or other areas of the head and neck. Third-generation Cephalosporins plus Vancomycin and Metronidazole is one regimen. They can then change treatment depending on cultures and sensitivities.4
Vancomycin does not cross the BBB; therefore, some authors advocate using Rifampin in its place while others may consider a short course of steroids. Linezolid and Daptomycin have also been used, but data on their efficacy are very limited.4
Antibiotic therapy is usually 6 to 8 weeks of intravenous agents since oral agents will possibly not achieve a therapeutic level in CSF that is needed for a cure.10
SEAs
The treatment usually comprises decompressive surgery, drainage of the abscess, and Eradication of the primary underlying infectious focus (if detectable).
Drainage of the abscess is considered the gold standard under most circumstances. The surgeon usually places a drainage system and continues to irrigate the abscesses for several days post-surgery until the infection is entirely resolved.
Parenteral antibiotic therapy; targets potential etiologic agents such as coagulase-negative staphylococci (CoNS), and streptococci.
A combination of a third-generation Cephalosporin (Ceftriaxone) with another antimicrobial that exhibits anti-staphylococcal activity (Rifampicin, Nafcillin, or Fosfomycin) is recommended.
Physicians must treat patients with antibiotic therapy for 4 to 6 weeks unless there is associated osteomyelitis, in which case they should continue the treatment for 6 to 8 weeks.1
Prevention
The most critical factor in preventing permanent disability is early recognition and treatment.11
Recent updates
In recent years, the number of reported cases of SEAs has elevated.23
The incidence rate of SEAs during the period (2004-2014) of 5.1 cases per 10,000 admissions. Mortality rates among SEAs cases have improved over time from a mortality rate of 81% in the 1920s to 34% in 1954-1960, and 15% in 1991-1997. There was a 7% mortality rate reported in recent studies.8