Article Topic: Skull fractures
Author name: Zaid Sayegh
Edited by: Philip Sweidan, Ethar Hazaimeh
Keywords: Skull fractures; Cranial fractures; head trauma; CSF leaks.
Overview
Over the past two decades, there has been a considerable increase in the number of head injuries which led to a spike in the number of skull fractures.[1] So in this article, we will discuss skull fractures which fall into four main categories: linear, depressed, diastatic, and basilar.[2] Cranial fractures are generally more common in children than in adults because children are more prone and vulnerable to head trauma due to their thinner and more pliable skulls which provide less protection to the brain.[3] Skull fractures can affect the brain either directly by inducing neurological or vascular damage or indirectly by the commonly associated intracranial hemorrhages that can compress the underlying brain tissue. [1,4]
Epidemiology
Skull fractures occur mostly between the ages of 1 and 20 years.[5] Basilar skull fractures are relatively rare and occur in about 4% of all patients with severe head injuries. They also constitute approximately 20% of all skull fractures.[6] Meanwhile, depressed skull fractures are present in around 10% of patients with severe head injury and are more frequent in males than females (7:1 ratio). [1,7]
On the contrary, Linear and diastatic fractures have a higher rate of occurrence in females which could be explained by the difference in the skull architecture between both sexes where males have thicker and stronger skulls that can absorb impact force.[1,5] When it comes to linear fractures, they happen more often in children because of their thinner skulls and happen to account for three-fourths of all pediatric skull fractures.[3,8]
Etiology
Skull fractures are caused by trauma to the head which can be categorized by etiology into accidental and non-accidental injuries. Some of the most common accidental causes of head injuries include a fall, motor vehicle accidents, sports-related injuries, pedestrian injuries, penetrating injuries like gunshot wounds, and direct blows to the head. [3,6] An example of a non-accidental head injury would be abuse which is more commonly seen in children and assault. [3,6] Depressed “ping-pong” fractures can sometimes occur in neonates due to injury at birth. [3]
Pathophysiology
The skull can be divided into two parts: the calvarium and the skull base. The former is composed of the frontal, parietal, occipital, and temporal bones while the latter is made up of the sphenoid, palatine, and maxillary bones as well as some parts of the temporal and occipital bones. [3] Now we will discuss each type of skull fracture:
Linear skull fractures usually occur in the temporal or parietal areas and involve no bone displacement. [3] While diastatic skull fractures occur when the fracture happens along one of the suture lines in the skull. [3]
Depressed skull fractures occur when part of the bony skull is displaced into the brain which increases the risk of underlying cerebral contusion or laceration. The most common sites of depression are the frontal area (53%) followed by the parietal region (28%). [9] These usually require surgical intervention. The damage caused by depressed skull fractures depends on the region of the brain affected by the displaced bone. [8,10]
Basilar fractures typically involve the temporal bones, the external auditory canal, and the tympanic membrane but may involve the occipital, sphenoid, ethmoid, and orbital plate of the frontal bone as well. Therefore, the location of the fracture can be utilized to predict the associated injuries. For instance, the most common kind of fractures, temporal fractures, are linked to carotid injury, injury to cranial nerves VII (Facial nerve) or VIII (vestibulocochlear nerve), and mastoid cerebrospinal fluid leak. Furthermore, Anterior skull base fractures are correlated with, nasal cerebrospinal fluid leak, orbital injury, and injury to cranial nerve I (olfactory nerve). Moreover, Central skull base fractures are linked to an injury to cranial nerves III, IV, V, or VI (oculomotor, trochlear, trigeminal, and abducens respectively) and carotid injury. Finally, Posterior skull-based fractures are related to a vertebral artery injury, cervical spine injury, and injury to the lower cranial nerves. The said kind of injuries tends to be critical and dreadful thus leaving the patients with hemiplegia or paraplegia.
Basilar skull fractures are usually seen with other central nervous systems (CNS) pathologies such as epidural hematoma due to the fragility of the temporal bone (which is the bone most commonly involved in basilar skull fractures) and its close proximity to the middle meningeal artery.[6]
Clinical presentation
The clinical presentation of basilar skull fractures is determined by the degree of cranial nerve and brain injury. Patients may experience nausea, and vomiting, or show signs of mental status alterations. These clinical features can be used to predict a basilar skull fracture. For instance, one of the earliest features of a basilar skull fracture is the tympanic membrane appearing purple which happens due to the accumulation of blood behind it from a fracture that involves the petrous ridge of the temporal bone. This is clinically known as Hemotympanum. [6]
A clinical manifestation typically occurs immediately after injury where the cerebrospinal fluid (CSF) seeps out of the ears or nose (CSF rhinorrhea or otorrhea) and mixes with blood to form a “Halo” sign which looks like a double ring pattern consisting of the two mentioned fluids. However, the “Halo” sign is not specific to CSF leaks as it can appear when blood mixes with water, saline, or mucous. CSF leaks can also occur within days to weeks after the initial trauma. [3,6] Distinguishing between CSF and mucous discharge presents difficulty due to the presence of glucose in both of these fluids which makes it hard to discern between them but the high level of chloride relative to serum can indicate that the fluid is the CSF.[11].
Furthermore, about 1 to 3 days after the initial trauma in fractures of the anterior cranial fossa, blood pools around the eyes causing periorbital ecchymosis (raccoon eyes). [6] Another clinical feature that appears 1 to 3 days after the incident is retroauricular or mastoid ecchymosis (Battle sign), where blood pools around the ears. This finding is associated with fractures to the middle cranial fossa. [6] Other clinical manifestations include tinnitus, nystagmus, hearing loss, vertigo, or cranial nerve palsies. [6,11]
Complications
The most common complications of cranial fractures include:
- CSF leak. [6]
- Pneumocephalus. [7]
- Cranial nerve palsies. [6]
- Hearing loss. [6]
- Cavernous sinus thrombosis. [6]
- Vertigo. [6]
- Carotid dissection, pseudoaneurysm or thrombosis. [6]
- Carotid-cavernous fistula. [6]
- Injury to cranial nerves III, IV, VI, VII and VIII. [6]
- Intracranial hemorrhage. [6]
- Seizures. [9]
- Meningitis. [3]
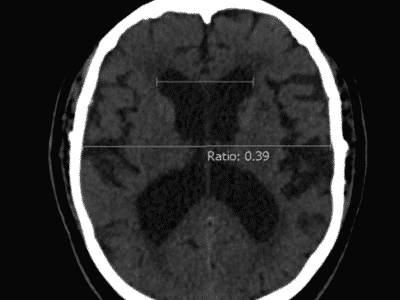
- Hydrocephalus. [12]
- Death. [6]
Diagnosis
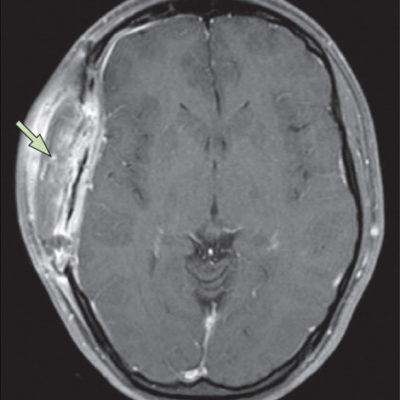
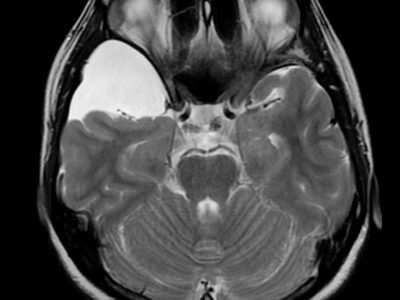
The diagnosis of skull fractures starts with a physical exam, Fractures like open compound depressed skull fractures can be palpitated through the laceration as depressions.[7] Usually, plain x-rays are not sensitive enough for a diagnosis especially for basilar skull fractures therefore computed tomography (CT) scans are used. Initially, evaluation is done using a non-contrast CT scan which cannot easily detect linear or non-displaced skull fractures.
If there is any suspicion that a basilar skull fracture is present, then a multidetector CT (MDCT) thin-slice scanning through the face and skull base is used to detect subtle fractures. Unfortunately, small neural and vascular channels seen on MDCT can be misinterpreted as fractures so further imaging with CT angiography and venography (CTA, CTV) is done to look for any vascular injuries. [6] MRI can also be utilized to assess nerve injury and look for CSF leak. [6] It is difficult to diagnose a CSF leak therefore the fluid should be sent for analysis of beta transferrin. [6] CT scanning should be done in all patients with suspected skull fractures to rule out any underlying intracranial pathologies. [8]
![Figure 1: Long linear branching left parietal fracture, case courtesy of Dr Dalia Ibrahim[13].](https://neuropedia.net/wp-content/uploads/2022/07/skull-fracture-linear-11-300x268.png)
Figure 1: Long linear branching left parietal fracture, case courtesy of Dr Dalia Ibrahim[13].


Figure 2 shows a biparietal diastatic skull fracture, case courtesy of Dr Ian Bickle[14].

Figure 3 shows a depressed skull fracture, case courtesy of Dr Ian Bickle[15].
 Figure 4 shows Heavily comminuted facial bone and base of skull fractures with bilateral Le Fort fractures. The right side demonstrates a Le Fort II while the left is a Le Fort III fracture. The base of the skull fracture extends through the body of the sphenoid consistent with a lateral frontal diagonal fracture pattern (see transsphenoidal basilar skull fractures). Case courtesy of Dr Amit Chacko[16].
Figure 4 shows Heavily comminuted facial bone and base of skull fractures with bilateral Le Fort fractures. The right side demonstrates a Le Fort II while the left is a Le Fort III fracture. The base of the skull fracture extends through the body of the sphenoid consistent with a lateral frontal diagonal fracture pattern (see transsphenoidal basilar skull fractures). Case courtesy of Dr Amit Chacko[16].
Management
The approach to dealing with cranial fractures depends on the location and type of the fracture along with the presence of any other intracranial pathologies. For instance, most simple linear fractures heal without intervention. [3]
Compound depressed skull fractures typically require neurosurgical intervention specifically in patients with radiological evidence of dural penetration, intracranial hemorrhage, frontal sinus involvement, or even pneumocephalus. In any of these cases, the advocated course of action is early operation and antibiotics. Delaying the treatment results in an elevated risk of meningitis, cerebritis, epilepsy, and death. However, open depressed skull fractures with no dural laceration are treated with local wound washout, closure, and antibiotics alone. [7]
Because basilar skull fractures are caused by significant trauma, the first step when treating them is a thorough trauma evaluation with interventions to stabilize the airway, ventilation, and circulatory issues. Nasogastric tubes, and nasotracheal intubation should be avoided due to the risk of inadvertent intracranial tube placement while nasal intermittent positive pressure ventilation (NIPPV) should be avoided since it can cause pneumocephalus. Patients with basilar skull fractures should be admitted for observation especially those who are taking anticoagulants. Some cases might be complicated by vascular injury, significant cranial nerve injury, persistent cerebrospinal fluid leak or intracranial bleeding which requires decompression, and these cases are considered in dire need of surgical management. In basilar skull fractures, there is an elevated risk of meningitis due to the increased possibility of bacteria from paranasal sinuses, nasopharynx, and the ear canal directly contacting the central nervous system. Therefore, patients with this kind of fracture are often treated with prophylactic antibiotics to prevent meningitis. However, there is no evidence to support the use of prophylactic antibiotics in preventing meningitis even in the presence of a CSF leak. Conversely, the use of antibiotics for prophylaxis is still considered appropriate in procedures like intracranial pressure (ICP) monitor placement.[6]
Surgery
Compound depressed skull fractures tend to be considered surgical emergencies and if they are not treated immediately certain serious complications could arise like meningitis, cerebral abscess, osteomyelitis, or post-traumatic seizure. [18] Therefore, patients with cranial fractures that are depressed to a degree that is greater than the thickness of the skull should be surgically treated by elevation, debridement, and antibiotics. [19] If the dura is injured, lacerated brain matter could be present in the wound which should be drained out and after proper hemostasis, the dural tear should be repaired in a watertight fashion where the pericranial graft or fascia lata could be used. [18] However, if there is no clinical or radiographic proof of dural penetration, significant intracranial hematoma, depression greater than 1 cm, frontal sinus involvement, gross cosmetic deformity, wound infection, pneumocephalus, or gross wound contamination, in all these situations a non-surgical approach can be taken. [19]
Prognosis
The prognosis of cranial fractures depends on:
- The associated dural tear and CSF leak. [6]
- The time the patient takes to get to the hospital. [17]
- Instability. [6]
- Associated injuries. [6]
- Initial severity of neurologic and vascular injuries. [6]
Usually, CSF leaks spontaneously resolve within 5-10 days while hearing loss typically resolves within 7-21 days. [6]
Acknowledgment: Thanks to IFMSA-JO.