Article topic: Rehabilitation for Patients with Multiple Sclerosis
Author: Yara Abu Al Halaweh
Editor: Ethar Hazaimeh
Keyword: Multiple sclerosis, Demyelinating, physiotherapy
Overview
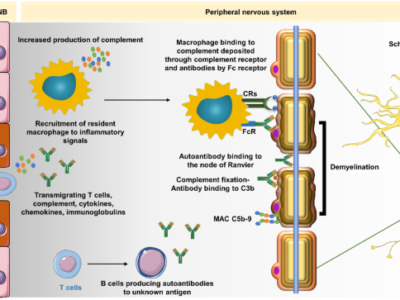
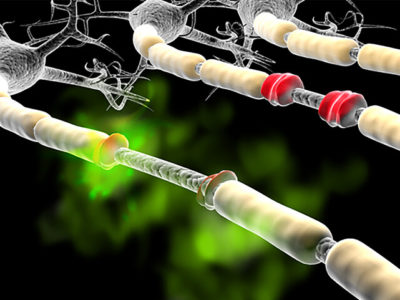
Multiple sclerosis ( MS ) is a long-lasting inflammatory demyelinating illness of the central nervous system (CNS) the reasons of which are not fully clear yet and whose course is tough to predict. 1 It is well recognized that the progress of demyelinating lesions might be caused by autoimmune processes as well as geographical and genetic factors. The pathophysiology of MS suspects that demyelination changes are harmful to the gray matter and cerebral cortex. As well as basal ganglia and cerebellar cortex. The inflammatory process is parallel to the existence of two main sub-types of immune cells and pro-inflammatory cytokines influences on the brain-blood barrier. Which is linked to swelling and neuronal dysfunction, which can lead to a relapse of the disease.2
Involvement of the myelin sheath and neurodegenerative processes result in a decrease in the number of synapses and axons, which eventually to the loss of nerve cells.3 Viral infections, insufficiency of vitamin D, and the action of sex hormones are recorded as some of many causes of the disease. Sex hormones consider an important factor influencing the development of (MS), which is reflected in the increase of ( MS) cases in women. Literature has shown that women suffering from MS who have higher levels of estradiol and decreased levels of progesterone experience greater severity of the disease.4,5 The highest rate is between the twenties and forties years of age. MS is also found in children as a childhood form of MS. People over 50 may be diagnosed with the late form of MS.6
Four main types of MS have been described9, 10; relapsing-remitting MS (RRMS), which consider 85% of cases. This type shows periods of symptom attacks and periods of complete remission; secondary progressive MS (SPMS) is described by an initial relapsing-remitting course and is marked by disability progression. The possibility of having SPMS is close to 2% each year and 50% will develop SPMS within 10 years11; primary progressive MS (PPMS) contain a worsening progression of disability, patients do not experience symptom relapses in fact there is a constant decrease of functional level from the time of disease onset, almost 10-15% of cases are this form of MS11; progressive relapsing MS (PRMS) is characterized by periods when symptoms gradually worsen and periods of symptom attacks. This type is the least frequent, affecting around 5% of patients with MS11. (Fig.1)

Fig.1 Main types of multiple sclerosis70
Rehabilitation and Multiple Sclerosis
Physiotherapy in multiple sclerosis’s main goal is to improve mobility through compensation mechanisms that work on the activation of capabilities of effectors and behavior, which gain in the patient regaining functioning, not a movement. The introduction of physical activity, regardless of the progression of the disease, will decrease the negative effects of akinesia, and thus improve the functional capabilities of all body systems7.
The severity of the disease, degree of impairment, and neurological deficiencies must all be considered in the rehabilitation program. The therapy at the time of remissions is therefore based on the level of impairment and the goals of treatment. The patient’s mental state, neurological status, and cognitive function state should all be considered in the process.8.
The continuousness of the rehabilitation should include exercises that target the problems caused by disease. Therefore, daily rehabilitation would be a mix of balance and coordination exercises. Also, breathing, stretching, and relaxation exercises. Additionally, it would include aerobic training, hydrotherapy, exercises that strengthen specific groups of muscles and get better proprioception. The intensity level of load and exercise should not cause overheating and fatigue of the body, which may result in an elevation in muscle tension. Kinesitherapy, physical therapy, massage, and hydrotherapy are all examples of physiotherapy, which is an important aspect of any rehabilitation program.
Hydrotherapy
In 1890, Professor Wilhelm Uhthoff reported that an elevation in body temperature due to physical effort could cause transient vision blindness in patients with MS due to retrobulbar optic neuritis. This effect was later described as the Uhthoff’s sign ‘’ Uhthoff’s phenomenon (also known as Uhthoff sign or Uhthoff syndrome) is described as non-permanent, short-lived (less than 24 hours), and stereotyped worsening of neurological function among multiple sclerosis patients in response to an elevation in core body temperature.’’- S Panginikkod, A Rayi, LA Rukmangadachar – 2017 (20), and up until 1983, the hot bath test was used as a diagnostic tool for MS. Heat and physical efforts were limited for the fear of flaring up the disease and hydrotherapy were restricted to a water temperature of 30 °C.12, 2321,22. These contain mainly resistance training and suggest an overall improvement in disability and movement with aerobic training.
Magnificent results have also been achieved with rehabilitation programs containing treatment in swimming pools at temperatures around 30ºC or higher. Rehabilitation approaches have to be designed specifically for the needs of each patient23, 24 Rehabilitation and active lifestyle have been beneficial to keep the quality of life of patients with MS25, 26. Aquatic therapy has become an essential element of the rehabilitation process of MS patients.
Cold baths along with cooling devices elevate local and systemic hypothermia in MS patients. Also, mobility in water focusing on trunk movement, postural stability exercises, and body position changes have provided benefits for rehabilitating gait in these patients27, 28. The hydrostatic, hydrodynamic, and thermal impacts of aquatic activities in inpatients with multiple sclerosis are based on the physical characteristics of water (viscosity, surface tension, density, specific heat, and heat conductivity).29. In MS patients, hydrotherapy is generally well tolerated and helps in decreasing fatigue, pain, gait speed, motor actions, and endurance level30 (Fig. 2). Although hydrotherapy has been well used in the rehabilitation program of patients with MS13-19, the possible harmful effects of heat in these patients have been long known.

Fig. 2 71 hydrotherapy for people with MS
Balance intervention for MS patients
The maintenance of balance or upright stance needs collaboration between multiple sensorimotor systems (visual, vestibular, proprioception) to provide coordinated movements that keep the center of mass within the limits of stability31, 32. Balance is a comprehensive component of physical function, and a product of the task is taken and the environment in where it is performed33. the elements of balance rehabilitation include multisensory and motor strategy training, strengthening and endurance training and a lot of neurotherapeutic approaches in individual targeted or group sessions therapy32, 33. Impairments in balance and the underlying physical functions are common in people with MS34-40.
Patients with MS have balance impairments characterized by increased sway in quiet stance, delayed responses to postural perturbations, and decreased ability to move towards their limits of stability41. Much of people with MS fall over and over41–43, have fear of falling44, and the risk of fall-related injuries is high 45, 46. High risk of fall has also been found in connection with various gait assessments41 and with the use of a assisted walking aid47. Recognition of the biomechanical and information processing demands affected by the task and by the environmental context allows us to assess this model33.
Manner of movement for the lower extremities, upper extremities, neck, and head have been improved. One of using techniques that both methods employ is a manual technique of facilitation of movement (PNF). The aim of this technique is to help the patient to perform a movement correctly in a specific activity, so we prevent a pathological position of the body and assist in the beginning and end of the movement. The PNF technique also contains gait training and exercises of facial muscles. Decrease the impairment of chewing, swallowing, and breathing. The prober muscle tension and active movements can be gained by preventing the abnormal patterns of posture. These exercises improve stability during gait, decrease falls, and improve posture control.
Coordination exercises enhance the coherence of movement and decrease energy consumption which is caused by deficiency of coordination1. Balance and proprioceptive exercises in people with stability in standing positions are executed by the use of stabilometric and posturemetric platforms depending on the biofeedback.
Hippotherapy is another type of exercise that enhances balance and stability in people with MS. Promoted gait and balance were seen in patients who take hippotherapy when compared to the control group in which traditional physiotherapy was taken49. Other studies may provide a better sight of the effects of physiotherapy interventions on the balance if the interventions were designed in more detail (e.g. type of exercise, term of intervention, weekly frequency of exercise, number of exercises per session).
Spasticity in people with MS
Spasticity is a common sign in MS, spastic paresis affects both limbs with higher severity of pathological tension in the lower extremities seen while higher physical efforts can increase muscle tension50. The physical application which is used pre kinesiotherapy is cooling the targeted parts of the body, as the spinal cord is treated with decreased temperatures also, this is to get the effect of topical anesthesia in peripheral sensory receptors, using of cold decrease responses to active stretching. Passive stretching is a contraindication, as it decreases the excitability of the motor neurons and keeps the elasticity properties of muscles and joints in 40–60% of patients with multiple sclerosis1. Mild spasticity is beneficial as it enhances blood circulation in the limbs and decreases muscular wasting. The high degree of spasticity (3 or 4 on the Ashworth scale) leads to contractures, joint deformity, and bed ulcers which cause infections50. The plan of the rehabilitation program should take into consideration the fact that the use of physical applications before kinesiotherapy has positive effects.
Physical techniques used in dealing with spasticity are electrotherapy and magnetic therapy. Electrical stimulation of transcutaneous electrical nerve stimulation (TENS), neuromuscular system (NMES). Electrical stimulation seems to be the best technique because harm to the upper motor neuron does not reverse the excitability of the muscles to electrical stimulation so that the affected bioelectrical function of muscles can be replaced.
The treatment parameters are set on the basis of Electromyography (EMG) or chosen according to the commonly accepted standards. Using implant electrodes may cause complications such as displacement of electrodes and this will lead to an adverse reaction of the body to the implant51. Transcutaneous electrical nerve stimulation (TENS) is a technique that has been widely used in the treating of pain in people with MS. Pads are placed along the nerves or in sites of pain. The frequency varies from 1 to 100 Hz, and the intensity depends on the patients according to their individual feelings. Hufschmidt procedure is also used to decrease muscle tension through the stimulation of spastic muscles and their antagonists.
Double square-wave impulses are used to get a functional balance between agonists and antagonists. This procedure helps in proprioceptive facilitation and affects alpha motor neurons52 Functional electrical stimulation (FES) runs mini stimulators that are placed to paretic muscles behind the control of the central nervous system. Magnetic fields of low and high frequencies are also used in people with multiple sclerosis. The benefit of using magnetic fields is the fact that they are painless, thermal, and porous through the patient’s tissue. In magnetotherapy, the frequency varies from 2 Hz to 60Hz, the induction can be up to 20. The application of impulses can be triangular, rectangular, sinusoidal, and trapezoidal shapes53. This application in people with MS is used to limit pain and reduction of muscle tension. In the case of spasticity, the intermittent mission of magnetic fields is begin with a 3 s break and then in each subsequent application, the break is gradually decreased by 0.5 s till it reaches continuous emission. This results in the decrease of muscular tension, relaxation, which helps in the reduction of fatigue syndrome54. The research of magneto stimulation has proven the efficacy of this treatment for the exertion of hormones such as melatonin is correlated to an analgesic effect and serotonin the increase of which enhance well-being and mood55.
Transcranial stimulation is a technique that involves stimulating specific areas of the cerebral cortex. This operation is used to improve the conductivity of the optic tract in the treatment of retrobulbar optic neuritis. The use of repeated transcranial magnetic stimulation in persons with MS resulted in a decrease in lower-limb stiffness and an improvement in neurogenic bladder dysfunction56. Laser radiation’s regeneration impact is significant for persons with MS because it promotes demyelination regeneration in the central nervous system, which reduces nerve conduction. Biostimulation laser light affects neuron regeneration by stimulating the development of Schwann cells, which improves nerve conduction. Because cold is utilized in combination with laser radiation, cool lasers are also used to alleviate muscular tension and offer analgesia57.
Resistance exercise for MS patients
Strengthening is considered one of the essential elements of exercise programs and physical activity for people with MS61. It might for strengthening training to improve function such as gait, it possible to need to be applied using parameters that different from what is desired to what is commonly used to improve force production. A final and probably important explanation is that strengthening training studies to facilitate gait in patients with MS may not include exercises with the appropriate intervention approach in order of modes, positions, or muscle targets62. Strength training using modes or positions that are not functional, or are not focused on muscle groups that are important for gait, may not be beneficial for walking even if strength gets stronger63. In older adults, strengthening training has been found to be the only beneficial exercise intervention to improve gait speed, intensity varies between 70% and 80% 1RM (or up to 7- to 8-repetition maximum)64.
Neurogenic bladder dysfunction
The rehabilitation plan should also contain pelvic diaphragm muscle exercises because of the neurogenic bladder dysfunction, which has been seen in 78% of people with MS1. Sphincter disorders caused by the form of urinary incontinence or retention lead to discomfort for patients and restrict their involvement in activities of daily living and social participation. Kegel isometric exercises, which involve tightening and relaxation of specific groups of muscles, are executed to exercise the pelvic diaphragm, which results in an improvement in muscle mass and strengthening and the growth of the resting tension of these muscles. The exercises help in long-term contraction of the muscles, enhancing control of neuromuscular and connective tissue to stabilize the pelvis, which, in turn, enhances the mechanism of urination. Pelvic diaphragm muscle training should be mixed with the enhancement of deep muscles like transversus abdominis mostly because of the synergistic action of these structures. Co-activation of these muscles is decreased or seated aside in patients with urinary incontinence65. Also, the training must include gluteal muscles, the adductor muscle, and the ischio-crural muscle group. The parallel use of Kegel exercises, EMG biofeedback, and electrical stimulation (NMES) provide very well results66.
Gait and endurance training
An overall analysis should precede gait training, with the goal of evaluating the impairment in many stages of gait in comparison to the normal gait style. Walking on a treadmill with a non-weight-bearing foot is one of the most commonly utilized training procedures. This contributes to the improvement of gait characteristics. The World Health Organization (WHO) recommends 30 minutes of moderate-intensity physical exercise five days a week, or 20 minutes of high-intensity physical activity three days a week.
Regulated physical activity in the type of sport or refreshment results in well health benefits, they prove the effectiveness of aerobic training in people with MS. The rehabilitation must be for several weeks or even months, mostly using a treadmill or a cycloergometer in this type of exercise8. Physical activities enhance their physical capacity and their mood and attitude to the exercises. Best cardiorespiratory efficiency has been confirmed to improve cerebrovascular function, which proposes that movement can also significantly enhance brain function in people with multiple sclerosis67. Aerobic training improves muscle strength of the lower limbs, which results in decreasing spasticity without the risk of relapse or the symptoms of fatigue68.

Figure 372 gait training for people with MS
Updated recommendations for people with MS propose doing physical activities two to three times per week at an intensity of 50–70% of VO2max up to 60–80% of maximum heart rate. The span of the exercise should not exceed the initial period of 40 min. The intensity should elevate gradually depending on the degree of disability. Studies showed that patients who do not practice physical activities got a significantly reduced quality of life and a major degree of disability compared to the group that practices regularly69 (Fig 3).