Article Topic: Multiple Sclerosis
Author: Kafa Al-Zoubi
Keywords: Multiple Sclerosis (MS), B cells, Pathogenesis, Classification
Scientific Editor: Marah Bassam Akhdar
Linguistic Editor: Noor AlOsta.
Definition
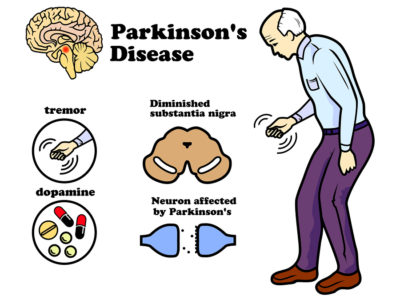
Multiple sclerosis is a chronic inflammatory demyelinating disease affecting the central nervous system in which oligodendrocytes are damaged and neuronal function is progressively lost (1). It is characterized by transient and frequent episodes of inflammation that result in demyelination and subsequent damage of the underlying axons in the brain, optic nerve, and spinal cord (2). The word sclerosis is derived from the Greek word “skleros”, meaning hard, and “Multiple” refers to the many different parts of the nervous system that may have damaged myelin. Multiple sclerosis is the most common autoimmune disease of the CNS (3).
The onset of multiple sclerosis typically develops in early adulthood between 20 and 40 years. Moreover, it affects women two to three times more than men (4). This has led to extensive studies of variation between women and men in the immune system or nervous system, which may be caused by the influence of gonadal hormones, genetic differences, as well as numerous environmental and current lifestyle exposures in men and women (5). Although MS appears in all regions of the world, its prevalence varies significantly, being highest in North America and Europe (140 and 108 per 100,000, respectively) and lowest in Sub-Saharan Africa and East Asia( 2.1 and 2.2 per 100,000, respectively) (6).
Etiology
The cause of MS is not clear but there are genetic and environmental factors that affect the disease:
Genetic factors
In first degree relatives of MS patients, the risk of MS is higher than the risk of the general population (absolute risk, 2-5% ) (7). In the general population, the probability of developing MS is nearly 0.1 %. The chance for a child to develop the disease if one of his parents have MS is about 2%, and the risk for relatives with second and third degree is about 1% (2). The human leukocyte antigen (HLA) complex contains the strongest genetic associations with MS. The main risk allele is the class II allele HLA-DRB1*1501 which increases the risk of MS three times in most populations (8). More recently, alleles of interleukin-2 receptor alpha gene (IL2RA) and interleukin-7 receptor alpha gene (IL7RA) have also been identified as inheritable risk factors (7).
Environmental factors
There are some environmental factors strongly associated with MS risk such as:
1-EPSTEIN BARR VIRUS (EBV)
The risk of developing MS is about 15-fold higher among people with a history of early childhood EBV infection and about 30-fold higher among those infected later in life with EBV (6). Primary EBV infection occurs mostly in young children and is asymptomatic in general. When it occurs in early adulthood it is more often associated with symptoms manifesting as infectious mononucleosis (IM), and there is an association between infectious mononucleosis occurrence and the development of MS (9).
2-VITAMIN D DEFICIENCY
Many studies have demonstrated that in some vulnerable patients, higher vitamin D levels have a potential protective effect (10). So the low level of vitamin D increases the risk of MS. It seems that vitamin D is not only an environmental risk factor that contributes to the risk of developing MS but may also modulate the activity and progression of the disease. In many studies, low serum levels of vitamin D have been associated with an increased relapse rate, increased impairment, and increased lesion load seen in magnetic resonance imaging (11).
3-SMOKING
There is a correlation between smoking and MS. Smoking also raises the risk of producing antibodies that neutralizes biologics, such as natalizumab and interferon β, used in the treatment of MS (10). Also, the intensity of smoking effect on MS susceptibility is low (relative risk 1.5) but still significant (12).
PATHOGENESIS
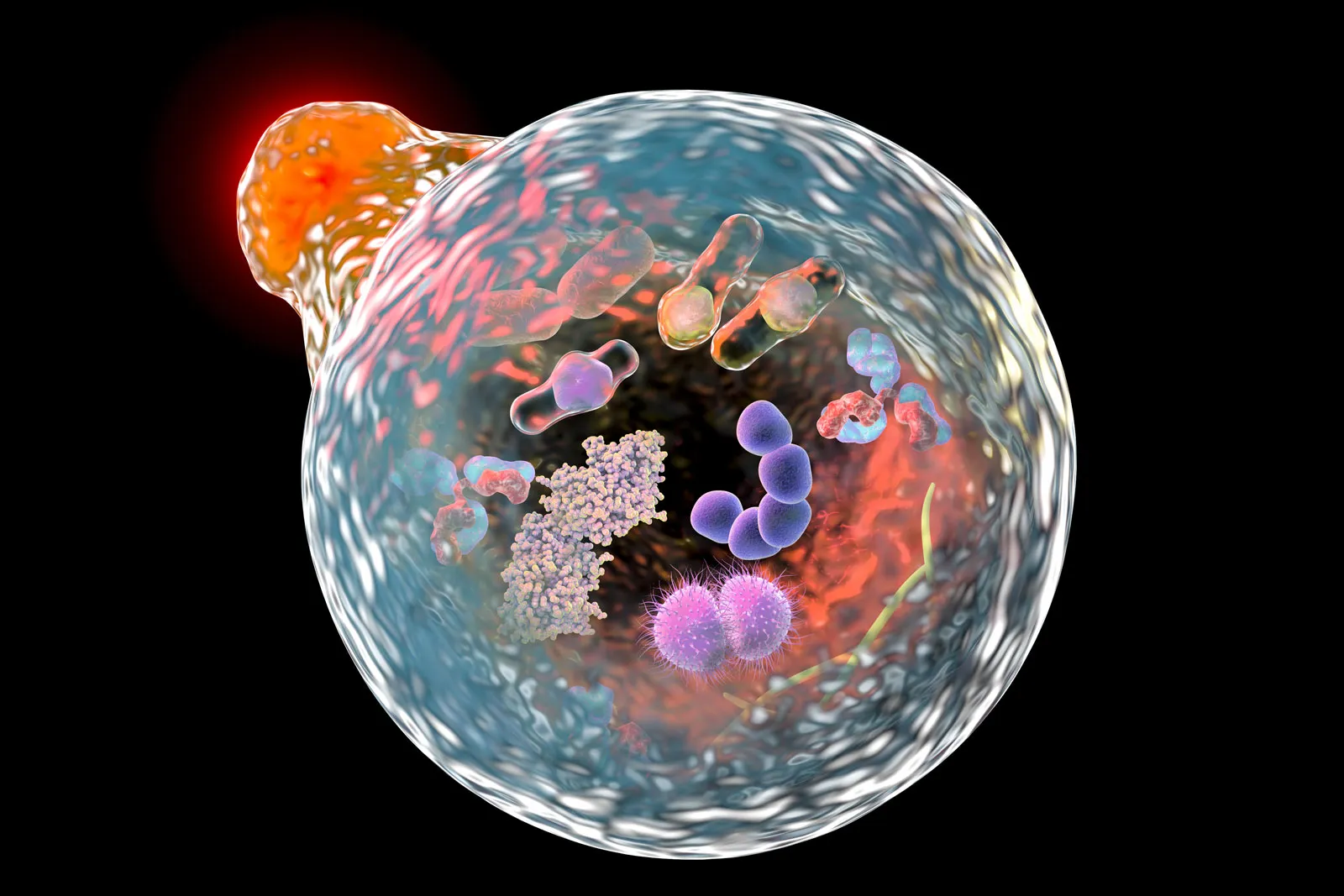
There are two major interconnected mechanisms describing the pathophysiology of MS, which are neuroinflammation and neurodegeneration (13). The inflammatory portion of the pathophysiology of MS includes abnormally excessive activation of the immune system against CNS antigen(s), resulting in interactions between autoreactive leukocytes and the inflamed cerebral endothelium, disintegration of the blood-brain barrier (BBB), and penetration of these activated leukocytes into the CNS parenchyma (14). Infections with a variety of viruses, such as EBV, has been proposed to be the activating factor for the T lymphocytes that are sensitized against viral proteins that share identical structures with CNS proteins; such as, Myelin basic protein (MBP), the so-called “molecular mimicry hypothesis (13).
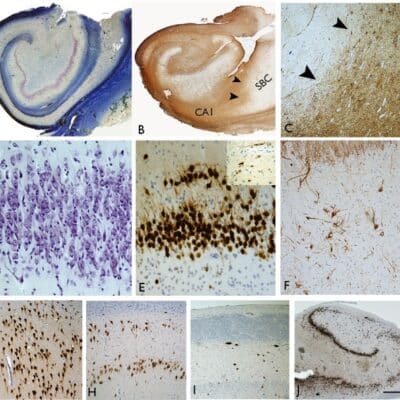
Various scientific studies, as experimental autoimmune encephalomyelitis (EAE) the closest animal model of MS, have demonstrated that autoreactive CNS-antigen(s)- directed T lymphocytes (CD4⁺, CD8⁺) play major roles in the development of CNS demyelinating lesions. IL-17, a potent inflammatory cytokine, stimulates CNS inflammation by disrupting the BBB, allowing greater permeation of autoreactive peripheral CD4⁺ T cells into the CNS (15).
Inflammation of white and gray matter tissue in the central nervous system is the main cause of damage in MS (16). Several studies suggested that the involvement of T helper (Th) cells (also known as CD4⁺ T cells) and adaptive immune responses initiated by interaction between antigen-presenting cells (APCs) with T lymphocytes play an important role in the initiation and progression of MS (17). Simultaneously, pathogen-associated molecules bind to toll-like APCs receptors, stimulating the production of specific cytokines including interleukin (IL)-12, IL-23, and IL-4 . These cytokines induce CD4⁺ T cell differentiation into Th1, Th2, or Th17 phenotypes that can release specific cytokines (18).
Th1 cells produce Interferon-gamma (IFNγ) and tumor necrosis factor-alpha (TNF-α). These cytokines can stimulate inflammation by suppressing Th2 differentiation, which releases the anti-inflammatory cytokines IL-4, and IL-13. IL-4 reduces pathological inflammation through the increase in M2 macrophage (repair macrophages), and alternative activation of M1 macrophages that promote inflammation (18). Th17 is another CD4⁺ T cell that releases a large number of cytokines (IL-17, IL-21, IL-22, and IL-26) which are capable of inducing inflammation(19).
Another CD4⁺ T cell type involved in the pathogenesis of MS is regulatory T cells (T reg). The function of T reg cells is to regulate effector Th1, Th2, and Th17 cells. Studies have demonstrated that for both MS and control patients, the number of T reg cells is the same, but MS patients have decreased T reg function (20). IFN-β improves CD4⁺ regulatory T-cell function, however, the specific mechanism of action of IFNβ-1a on the T reg function is still unclear and requires more investigation.
In MS lesions, CD8⁺ T cells are present and may have a regulatory role in the
progression of the disease. CD8⁺ cells mediate the inhibition of the proliferation of CD4⁺ T cells by secreting perforin, which is cytotoxic to CD4⁺ T cells, resulting in their inactivation (17). CD8⁺ cells also destroy glial cells, leaving exposed axons. In addition, CD8⁺ T cells transect axons, facilitate vascular permeability, and activate the death of oligodendrocytes (21).
Under normal conditions, B lymphocytes do not cross the BBB. During MS along the massive immune cascade, B lymphocytes become initiated, produce antibodies, and cross the BBB (13). There are multiple roles of B cells in MS. While antigen-activated B cells differentiate into plasma cells that secrete antibodies, they act as strong APCs. Also, it can exert anti inflammatory properties that modulate the effector role of other immune cells (22).
The precursors of antibody-secreting plasma cells, B cells
The development of these polyclonal antibodies is known as oligoclonal
bands(OCB)in the cerebrospinal fluid of patients with MS (16). About 90% of MS patients have IgG OCBs, but just 30 %-40 % have IgM OCBs and the hallmark diagnostic finding in the cerebrospinal fluid (CSF) are elevated numbers of clonally expanded B cells and oligoclonal immunoglobulin bands (23).
Plasma cells and antibodies produced from B cells are present in the majority of inflammatory CNS plaques. The involvement of antibodies in MS pathogenesis is provided by the identification of antibodies that bind to myelin fragments within phagocytes and also complement depositions in perivascular MS lesions(24). In addition, studies have demonstrated that antibodies produced by plasma cells clonally expanded in the CSF of Patients with MS can bind to CNS tissue, causing demyelination mediated by complement (25).
Some CNS auto-antigens, including myelin oligodendrocyte glycoprotein (MOG), myelin basic protein myelin-derived lipids, neurofascin, contactin-2, KIR4-1, as well as some intracellular auto-antigens such as DNA and RNA have been identified as targets for serum or CSF antibodies (26).
B cells as antigen-presenting cells(APCs) for activation of T cells
B cells can contribute as APCs for T cell activation to the development and
progression of CNS autoimmune diseases. Recognition of T-cell antigen must occur twice, once in the periphery that helps activated-T cells to enter the CNS, and another time inside the CNS that activates and directs encephalitogenic T-cell effector function. In CNS autoimmune diseases, many forms of APCs may lead to T-cell activation. Generally, they can be classified into APCs that are resident (CNS) and nonresident (bone-marrow-derived). In comparison, non-resident, peripheral APCs play a more significant role in inducing CNS demyelinating disease (28).
Activation of myelin-specific T cells requires recognition of myelin antigen in
association with MHC class II molecules expressed on antigen-presenting cells. In MS pathogenesis, many forms of APC can participate in T cell activation (29). B cells are more successful in presenting protein antigens and tend to be the strongest APCs at low concentrations of antigen since their unique receptor can detect neoantigens (30). Besides, CNS resident microglia and astrocytes have the ability under inflammatory conditions to express the molecules necessary for antigen presentation (29).
B-cell activation by a combination of the T-cell products CD40L and interleukin (IL)-4, but not by unspecific factors such as toll-like receptor ligand and IL-2-rendered B-cells capable of stimulating T-cells in a myelin-antigen-specific way. These data demonstrate that T-cell-mediated activation of B cells is extremely important for their capability to process and present antigen to T cells and that both populations thereby reciprocally stimulate each other (31).
The role of cytokines secreted by B cells in MS
B cells may regulate inflammatory processes through the release of pro and anti-inflammatory cytokines. B cells of MS patients produce abnormally high levels of IL-6, tumor necrosis factor α (TNFα), lymphotoxin α (LT-α), and granulocyte-macrophage colony-stimulating factor (GM-CSF) (32). Enhanced production of these pro-inflammatory cytokines by B cells can stimulate other immune cells leading to disease progression IL-6 secreted by B cells can promote Th17 cell differentiation and conversely can inhibit differentiation of regulatory T cells (33).
Also, B cells can regulate immune responses by producing anti-inflammatory
cytokines such as IL-10, IL-35 and transforming growth factor-b (34). Studies have demonstrated that B-cell-produced IL-10 plays a key role in recovery from an acute attack of CNS autoimmunity (35). These IL-35-producing B cells can regulate immune responses through induction of IL-10-producing B cells, indicating that IL-35 can be used to stimulate regulatory B cells to treat
autoimmune diseases(36). B-cell-derived transforming growth factor-b1 limits the early induction phase of EAE by inhibition of Th1/Th17 responses and activity of dendritic cell APC (37).
Types of MS
There are four types of MS (38) :
1- Relapsing-remitting MS: The most common type, affecting around 85% of
MS patients. It is characterized by flare-ups (relapses or exacerbations) of
symptoms followed by periods of remission when symptoms improve or vanish.
2- Secondary progressive MS: It may evolve in some patients with the relapsing-remitting disease. Disease-modifying agents help delay the progression of this type of MS in many patients. The disease course continues to worsen with or without intervals of remission or leveling off of symptom severity (plateaus).
3- Primary progressive MS: It affects about 10% of patients with MS. Symptoms continue to steadily escalate from the onset. There are no relapses or remissions, but periodic plateaus can be present. This form of MS is more resistant to drugs that are usually used to treat the disease.
4- Progressive-relapsing MS: this is an unusual form, affecting less than 5% of
patients. It is gradual from the onset, with occasional flare-ups of deteriorating symptoms along the way. There are no remission intervals.