Article topic: Criteria of Brain Death
Author: Hebah Samer Altaweel
Editors: Bashar Abualsebaa , Sadeen Eid.
Reviewer: Ethar Hazaimeh
Keywords: Brain death, Coma, Brainstem Reflexes, apnea test, absence of cerebral blood flow, organ donation, criteria for death.
Introduction
Brain death (BD) is defined as the complete and permanent loss of brain function as defined by an unresponsive coma with loss of capacity for consciousness, brainstem reflexes, and the ability to breathe independently [1]. A determination of death must be made by the accepted medical standards and must additionally include one of the following [3]:
- Irreversible cessation of circulatory and pulmonary functions.
- Irreversible cessation of all functions of the entire brain, including the brainstem.
The determination of brain death holds supreme significance in medical practice. For instance, in the context of organ donation, it enables the maximization of viable organs suitable for transplantation. Furthermore, it plays a pivotal role in clinical management by guiding clinicians to refrain from administering futile treatments and instead concentrate on delivering palliative care to patients and offering support to their families. Additionally, brain death certification carries significant implications in legal contexts and ethical decision-making processes. Its determination is based on updated guidelines for both children [4] and adults [5] that delineate a regimented series of clinical criteria conducted largely at the bedside. When the criteria have been fulfilled, the patient is declared dead and organ support continues only if organ donation is planned.
Brain Death Criteria
Understanding the criteria used to diagnose brain death is crucial for healthcare professionals, policymakers, and the general public because it forms the basis for critical decisions regarding patient care, organ transplantation, and legal determinations of death.
Brain death criteria have historically been based on three cardinal features: coma, brainstem areflexia, and apnea, and have consequently experienced minimal changes. In 1995, the American Academy of Neurology (AAN) outlined these criteria in a step-by-step manner, including prerequisites, clinical examination, ancillary testing, and documentation [6].
Fifty years ago, the ad hoc committee of Harvard Medical School provided the influential first guidance on confirming death using neurological criteria (DNC). Currently, 70% of countries have established legal or professional frameworks enabling the use of DNC. Although there is widespread acceptance of a three-staged approach to the clinical diagnosis of brain death, there are variations in international practice. It is imperative to develop international consensus and standards in the future to maintain and enhance public and professional confidence in the diagnosis [7].
Etiology
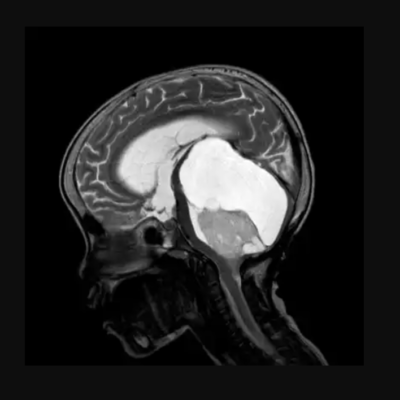
Brain death is diagnosed following catastrophic brain injuries such as trauma, intracranial hemorrhage, or hypoxic brain injury while the circulation is present, and ventilation is provided mechanically, hypoxic brain injury following increasingly successful cardiopulmonary resuscitation (CPR) after cardiac arrest is recognized as one of the most common etiologies of brain death [7], so brain death can be caused by various conditions or events that result in severe brain injury or damage such as brain tumors, stroke and anoxic brain injury.
In addition brain death can occur via two mechanisms
- Intracranial causes: In adults, the predominant intracranial injuries leading to brain death are traumatic brain injuries (TBI) and subarachnoid hemorrhage. These injuries elevate intracranial pressure (ICP), impair cerebral perfusion, and reduce brain tissue oxygenation, leading to neuronal damage. In pediatric cases, non-accidental trauma is a common cause, contributing to increased ICP and subsequent brain injury [9][10].
- Extracranial causes: In both adults and children, a significant extracranial cause of brain death is cardiopulmonary arrest with delayed or inadequate resuscitation [11].
Epidemiology
The most common processes leading to brain death in order of frequency, are cardiopulmonary arrest, traumatic brain injury (TBI), subarachnoid hemorrhage, and intracerebral hemorrhage. Among extracranial causes, patient who experiences cardiopulmonary arrest shows a progression to brain death in 8.9% of cases post-resuscitation. For those presenting with TBI, the rate of progression to brain death ranges from 2.8% to 6.1%. Regarding intracranial etiologies, patients with a subarachnoid hemorrhage proceed to brain death in 8.5% to 10.7% of cases, while those with intracerebral hemorrhage progress at a rate of 6.1% to 9.6% [12][13]. Notably, brain death is associated with a 100% mortality rate.
Pathophysiology
The pathophysiology of brain death involves a series of events that ultimately result in the cessation of brain function. This process can include:
- Primary injury, such as trauma or stroke, directly damages brain cells and disrupts normal brain function.
- Secondary injury following the initial insult, triggers various secondary mechanisms including inflammation and oxidative stress.
- Disruption of cerebral blood flow.
- Loss of brainstem function, responsible for regulating breathing and heart rate. When brainstem function is compromised, the body cannot maintain vital functions independently, leading to brain death.
This cascade provides a widely accepted understanding of the processes leading to brain death. However, the specific sequence and mechanisms may vary depending on the nature of the injury and individual factors.
Histopathology
Microscopic evaluation of postmortem brain-dead patients reveals varying degrees of neuronal ischemic changes. The hemispheric lobes and basal ganglia are the most common areas to experience severe ischemic change, followed by the pons, medulla oblongata, midbrain, and thalamus respectively. Autolysis of the cerebellum can also be appreciated in many autopsies [14].
Clinical presentation of brain death
Determination of brain death can be done with a clinical examination that demonstrates coma, brainstem areflexia, and apnea. This is seen when:
- There is no evidence of arousal or awareness of maximal external stimulation, including noxious visual, auditory, and tactile stimulation
- Pupils are fixed in a midsize or dilated position and are nonreactive to light
- Corneal, oculocephalic, and oculovestibular reflexes are absent
- There is no facial movement to noxious stimulation
- The gag reflex is absent to bilateral posterior pharyngeal stimulation
- The cough reflex is absent to deep tracheal suctioning
- There is no brain-mediated motor response to noxious stimulation of the limbs
- Spontaneous respirations are not observed when apnea test targets reach pH <7.30 and Paco2 ≥60 mm Hg.
If the clinical examination cannot be completed, ancillary testing may be considered with blood flow studies or electrophysiological testing. Special consideration is needed for children, for persons receiving extracorporeal membrane oxygenation, and for those receiving therapeutic hypothermia, as well as for factors such as religious, societal, and cultural perspectives, legal requirements and resource availability [2].
Diagnostic criteria for brain death
The diagnosis of brain death (BD) is legally and medically accepted [8]. To confirm the absence of brain function, protocolized bedside neurologic examinations are performed that evaluate for complete loss of responsiveness, spontaneous or induced movements, and brainstem reflexes [5].
Before deciding to proceed with the diagnosis of brain death, several conditions must be evaluated and met [16]:
- We should know what’s causing the coma and make sure there aren’t other serious health problems like major issues with metabolism, hormones, or body chemistry that could be confusing [5][15].
- Body temperature should be above 36 degrees Celsius.
- Systolic blood pressure (SBP) above 100 mm Hg.
- If there’s suspicion of drug intoxication or recent use of neuromuscular blocking agents, it’s important to wait for five times the drug’s half-life for it to clear from the body, considering any changes in kidney and liver functions.
If these conditions are present and there is an identified cause of coma and complete lack of brainstem reflex, you may proceed with apnea testing which performed using the following protocol as is recommended by the AAN:
- Adjust vasopressors to maintain SBP ≥100 mm Hg.
- Administer pre-oxygenation with 100% FiO2 for at least 10 minutes to achieve PaO2 >200 mm Hg.
- Decrease ventilator frequency to 10 breaths per minute.
- Lower positive end-expiratory pressure to 5 cm H2O.
- If SpO2 remains >95%, obtain baseline blood gas.
- Disconnect the patient from the ventilator and maintain oxygenation with 100% FiO2 at 6 L per minute near the carina through the endotracheal tube.
- Monitor for respiratory movements for 8 to 10 minutes.
- Repeat blood gas analysis for around 8 minutes if no respiratory effort is observed.
- A positive apnea test result is indicated if there are no respiratory movements and PaCO2 exceeds 60 mm Hg or shows a 20 mm Hg increase over baseline.
If the above list is completed and leads to coma, brainstem areflexia, and a positive apnea test is present, the diagnosis of brain death can be made [16].
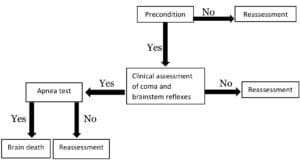
Figure 1: Diagnostic process used to determine brain death.
Ancillary tests are used when apnea testing is inconclusive or patients are too unstable to proceed with apnea testing [17]. These tests include:
- Cerebral angiography, specifically four-vessel angiography, is considered the gold standard for assessing cerebral blood flow. It confirms brain death by revealing the absence of blood flow to the brain.
- Transcranial ultrasound (US) enables the evaluation of bilateral pulsations in arteries such as the middle cerebral, vertebral, basilar, anterior cerebral, or ophthalmic arteries. It confirms brain death by detecting either small, peaked systolic pulsations or the absence of diastolic pulsations.
- Computed tomography (CT) and magnetic resonance angiography (MRA) of the brain can be employed to demonstrate the cessation of cerebral blood flow.
- Somatosensory evoked potentials (SSEPs) these imaging techniques can validate EEG results, as they are less susceptible to the influence of drug intoxication; however, they may still be impacted by hypothermia [18][19].
-
The Connection Between Brain Beath and Organ Donation
The potential organ donor with brain death is a patient in the intensive care unit (ICU) who has sustained a severe brain injury. For instance, this could include patients with anoxic brain injury, head trauma, or cerebral vascular accident. Before the declaration of brain death, the patient is under the care of the intensivist and the ICU team. During their ICU stay, there comes a point when it is deemed that further treatment is futile in terms of saving the patient’s life. However, it remains essential for the healthcare team to maintain hemodynamic stability.
Although they may not be able to save the patient’s life, it is crucial for the care team to consider the potential for organ donation, which could save the lives of others. By continuing aggressive care, the ICU team not only preserves the opportunity for organ donation for the patient and their family but also significantly influences organ function and the ultimate yield if the patient becomes a donor. Through the management of such patients, the ICU team actively contributes to providing the gift of life to others [20].
-
Prognosis
The prognosis of brain death, is 100% fatal and there is no cure [16].
-
Conclusion
Confirming brain death requires demonstrating permanent damage to the entire brain, including the brainstem. Current guidelines rely on thorough bedside clinical examination to ensure the patient has irreversible coma caused by conditions that can lead to brain death, absence of certain reflexes, and inability to breathe. However, there’s a lot of variation in how different healthcare providers, institutions, states, and professional organizations handle this process [21].
To avoid legal conflicts, the use of a standardized protocol of brain death is crucial. The brain death protocol must be performed in all patients with unresponsiveness, brainstem areflexia, and apnea. The exclusion of reversible causes of coma is essential and the investigation of brain death must be carried out regardless of whether the patient is an organ donor or not [22].