Article topic: Brain Hemorrhage
Author: Kafa Alzoubi
Editors : Yazan Zamer
Keywords: hematoma, epidural hematoma, subdural hematoma(SDH), chronic subdural hematoma(CSDH)
Hematoma
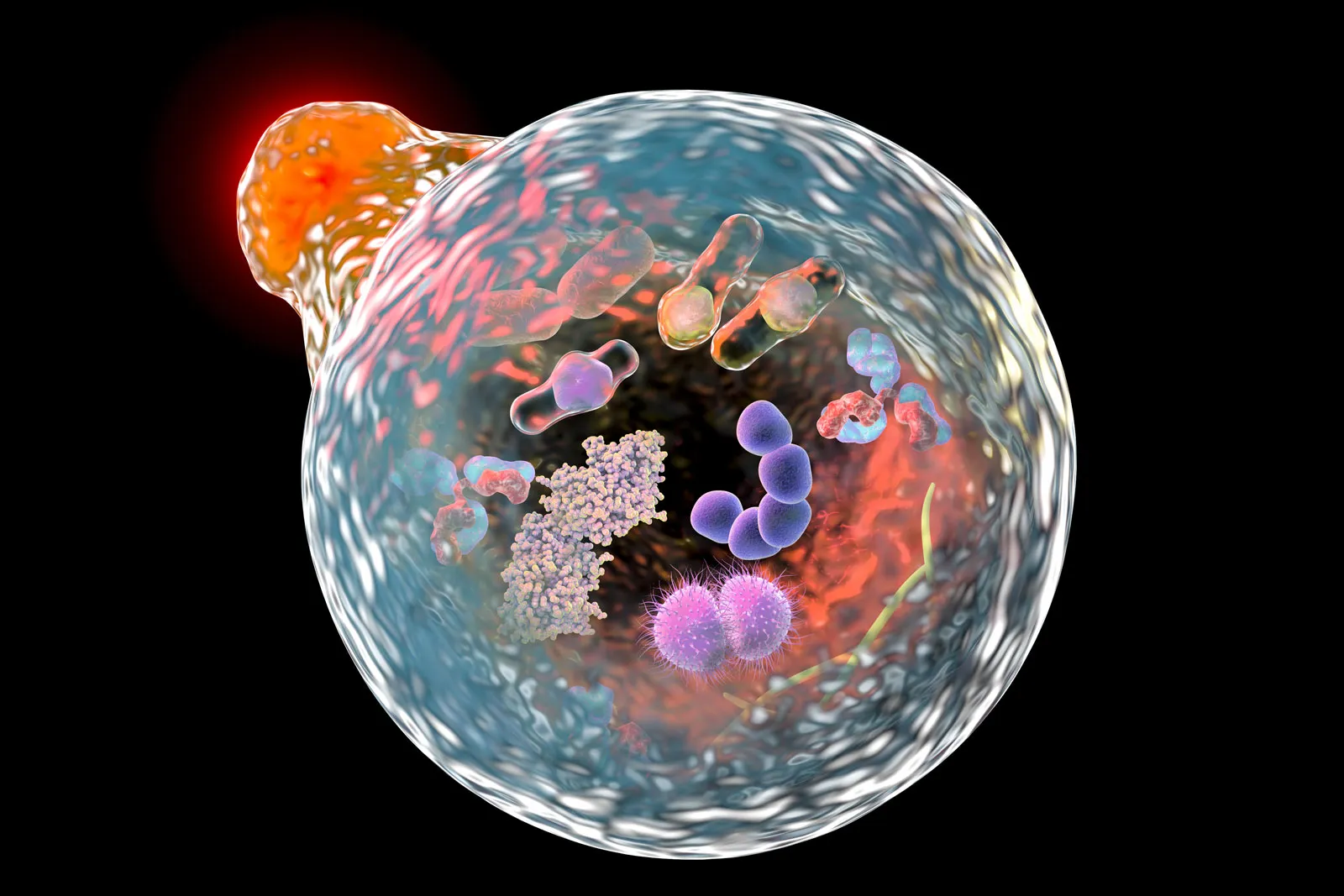
Hematoma is a localized collection of blood and can occur anywhere in the body. It is derived from Greek roots (heme) means blood and (oma) means process but as the pathological term indicates a mass. It can be spontaneous due to coagulation disorders or anticoagulant therapy and can be secondary to trauma or surgery. Hematoma may be hyperacute or persistent in length and therefore its internal contents range from fresh hemorrhage to chronic breakdown products of hemoglobin (such as hemosiderin and ferritin) and sometimes, a combination of various aged components. (1)
The collection’s physical stability can often range from a strictly liquid hyperacute collection to a chronic solidified mass-like state, but mostly a mixed cystic-solid state. When first developed, hematomas are normally sterile, and the majority remain uninfected.
There are three types of intracranial hematoma: epidural hematoma, subdural hematoma, and intracerebral (intraparenchymal) hematoma. (1)
Epidural hematoma
Epidural hematoma is also known as extradural hematoma which is an abnormal collection of blood within the potential space between the outer layer of the dura mater and the skull (2). Epidural hematomas form less than 4% of traumatic brain injuries. It is considered one of the most significant complications because of that the bleeding grows quickly and compresses the brain that leads to herniation and brain death, it can be life-threatening. (3)
The mortality rate varies from 10% to 40% and has declined due to early treatment and development of diagnosis and testing instruments. (4). The location of hematoma is grouped as frontal when the hematoma is confined to the anterior cranial fossa, vertical when it overlays the sagittal sinus, basal when it is on the floor of the middle fossa, and occipital when it is above the transverse sinus. (5)
The majority of hematoma is located in the lateral region due to the thinness of the temporal squamous (5). Also, epidural hematoma affects young adults more than elderly people because with age the dura mater becomes more adherent to the overlying bone. (6)
Etiology
The majority of cases related to a traumatic mechanism are a result of head injuries due to motor vehicle collisions, physical assaults, or accidental falls. Non-traumatic mechanisms include the following: (5)
- Infection/Abscess
- Coagulopathy
- Hemorrhagic Tumors
- Vascular Malformation

Figure1
Figure1: epidural hematoma, Case contributed by Dr. Heba Abdelmonem (https://radiopaedia.org/users/heba%20mohamed?lang=us)(7)
Pathogenesis
The majority of epidural hematomas are due to bleedings of arterial origin usually from the middle meningeal artery which is a branch of the maxillary artery. whereas non-arterial epidural hematoma can be caused by injuries to the dural venous sinuses, the arachnoid villi, or the emissary veins (9). The pathological effect of epidural hematoma is caused by intrinsic brain compression and later by distortion and elevated intracranial pressure. (10) Based on radiographic progression, it can be classified into one of the following:
Class I: Acute happens on day 1 and is usually associated with an un-clotted blood “swirl”
Class II: Subacute occurring from days 2 to 4 and is for the most part solid
Class III: Chronic from days 7 to 20, either mixed or light presence with contrast .
A subdural hematoma is a collection of blood between the dura mater and arachnoid mater of meninges surrounding the brain (11). It usually affects elderly patients because brain weight decreases with rising age, which contributes to a rise in extracerebral volume. Thus, after mild head trauma in elderly patients, an arachnoid tear can quickly occur and subdural hygromas develop into chronic subdural hematoma in around one-quarter of them (12).
Etiology
In most cases, acute SDH is associated with a clear traumatic incident, but acute SDH may occur spontaneously in some cases. The use of anticoagulants or antiplatelet agents and the collapse of an intracranial aneurysm are significant causes of spontaneous SDH, less commonly, SDH also can result from bleeding due to arteriovenous malformation, vascular meningiomas, dural metastases, and spontaneous intracranial hypotension (13). It is found in about 10% to 20% of traumatic brain injury patients, mostly related to road collisions, violent aggression, and unintentional Sport crashes (13). The most frequent cause of subdural hematoma in pediatric patients is trauma. Blunt and shearing accidents are contributory causes. Most subdural hematoma in the newborn period is caused by the use of cranium extraction instruments and traumatic birth delivery (14).
Pathogenesis
A subdural hematoma results from the tearing of the veins that bind the cerebral cortex and the dural sinuses, which induces blood to accumulate between arachnoid and dura maters(15). Subdural hematoma based on their acuity is categorized into acute, subacute, and chronic subtypes. Without rapid surgical intervention, acute subdural hematomas are highly dangerous and sometimes fatal. Symptoms grow gradually, and based on a variety of primary and secondary causes, mortality rates differ tremendously (16). Around 1% to 6% of untreated acute subdural hematomas undergo development into CSDH on average 3 weeks after initial trauma (17).
In younger individuals, acute subdural hematomas typically occur following serious damage, frequently associated with structural brain damage, and within 72 hours. CSDHs often occur in the elderly after a small injury without any damage to the underlying brain, and often there is a period of weeks to months before it becomes clinically obvious (18).
The evolving hematoma capsule demonstrates gradual changes with development in the age of the hematoma in the cell and vascular organization (17). The primary changes include angiogenic and aseptic inflammatory reactions. It is followed by fibroblastic-proliferation and the development of collagen fibrils. Young hematomas (15-21 days after trauma) show multiple blood vessels ,suggesting the formation of new blood vessels. Older hematomas (40 days after trauma) usually show several capillaries and thin-walled sinusoids accompanied by patent, larger diameter blood vessels. (17)

Figure 3: epidural and subdural hematoma
References:
- radiopedia. hematoma [Internet]. Available from: https://radiopaedia.org/articles/haematoma?lang=us
- Khairat A, Waseem M. Epidural Hematoma. In Treasure Island (FL); 2020.
- Rosenthal AA, Solomon RJ, Eyerly-Webb SA, Sanchez R, Lee SK, Kiffin C, et al. Traumatic Epidural Hematoma: Patient Characteristics and Management. Am Surg. 2017 Nov;83(11): e438–40.
- Pereira ELR, Rodrigues DB, Lima LO, Sawada LA, Hermes M de NJ. Bilateral asymmetric epidural hematoma. Vol. 6, Surgical neurology international. 2015. p. 14.
- Jamieson KG, Yelland JD. Extradural hematoma. Report of 167 cases. J Neurosurg. 1968 Jul;29(1):13–23.
- Chicote Álvarez E, González Castro A, Ortiz Lasa M, Jiménez Alfonso A, Escudero Acha P, Rodríguez Borregán JC, et al. Epidemiology of traumatic brain injury in the elderly over a 25-year period. Rev Esp Anestesiol Reanim. 2018 Dec;65(10):546–51.
- radiopedia. epidural hematoma.
- anatomical justice. No Title [Internet]. Available from: https://images.app.googl/1gPPhEvLMqs22wMJ9
- Giannakaki V, Triantafyllou T, Drossos D, Papapetrou K. Post-Traumatic Bifrontoparietal Extradural Hematoma with Superior Sagittal Sinus Detachment: A Case Report and Review of the Literature. World Neurosurg. 2016 Sep; 93:489. e17-20.
- ML Babu, SK Bhasin AK-JS. Extradural hematoma-an experience of 300 cases. 2005.
- Sahyouni R, Goshtasbi K, Mahmoodi A, Tran DK, Chen JW. Chronic Subdural Hematoma: A Historical and Clinical Perspective. World Neurosurg. 2017 Dec; 108:948–53.
- Uno M, Toi H, Hirai S. Chronic Subdural Hematoma in Elderly Patients: Is This Disease Benign? Neurol Med Chir (Tokyo). 2017 Aug;57(8):402–9.
- Al-Mufti F, Mayer SA. Neurocritical Care of Acute Subdural Hemorrhage. Neurosurg Clin N Am. 2017 Apr;28(2):267–78.
- Pierre L, Kondamudi NP. Subdural Hematoma. In Treasure Island (FL); 2020.
- Lim M, Kheok SW, Lim KC, Venkatanarasimha N, Small JE, Chen RC. Subdural hematoma mimics. Clin Radiol. 2019 Sep;74(9):663–75.
- Adelman JSK and EE. Subdural hematoma. Available from: https://www.britannica.com/science/subdural-hematoma
- Yadav YR, Parihar V, Namdev H, Bajaj J. Chronic subdural hematoma. Asian J Neurosurg. 2016;11(4):330–42.
NSC-Hematoma-Kafa Alzoubi-1