Article topic: Myelomeningocele
Author: Lubna Al-Rawabdeh
Editor: Omar Jbarah
Reviewer: Ethar Hazaimeh
Keywords: Myelomeningocele, Spina bifida, Hydrocephalus, Chiari Malformation
Overview
Myelomeningocele is classified as a development defect represented by a neural tube progenitor. Such a condition is observed in one in every 2900 live births and is classified under the severe category of spina bifida [1]. This condition results from neural tube closure defects and is characterized by the clinical signs of bony column fusion in the posterior vertebral region [2]. In such circumstances, due to abnormal development of the cord and the meninges, motor and sensory deficits are below the lesion level [2]. Furthermore, persons with myelomeningocele can have several other associated problems including; musculoskeletal deformities, bladder and bowel incontinence, as well as impaired cognitive functioning [2].
Etiology
The occurrence of myelomeningocele arises from a combination of genetics and environmental factors. Genetic factors contribute to the inherited traits, particularly, myelomeningocele. For instance, polymorphisms within a gene associated with planar cell polarity (PCP) have been documented to contribute to the defects of the tube the most notable of which is myelomeningocele [3]. These genes are associated with the control of the orientation of the cells and the arrangement of tissues during the period of growth.
Mice experiments have shown that there are mutations in the PCA gene leading to similar problems regarding the closing of the neural tube during development which are characteristic of myelomeningocele. Certain detrimental mutations within the PCP have also been observed in suffering human samples with target tube defects suggestive of a common underlying cause [3].
It is worth mentioning that environmental factors are not the only cause of myelomeningocele. Studies have shown that there is a high prevalence of SIBO in cases of myelomeningocele and constipation [4]. SIBO is caused by bowel flora overgrowth in the intestines, which may lead to other bowel symptoms including constipation. Also, some research has pointed out, that several women with myelomeningocele have motility problems and anorectal anomalies that may lead to some blockade and severe constipation [4].
Moreover, McClone and Knepper (1989) gave a theory regarding the cause of Chiari II malformations which are commonly associated with the myelomeningocele [5]. The Chiari Il malformation is believed to have arisen as a result of the Chiari system that does not dilate due to open neural tube and closure defects. In such children with myelomeningocele, this kind of abnormality which is also accompanied by a reduction in the size of the posterior cranial fossa, and disorganization of the cranium, becomes a cause of death. The authors stressed that for the brain to develop, growth and pressure in the cranial saccules are required [5]. Additionally, a study by Ortiz Cruz et al. (2021) linked the aberrations in the myelomeningocele phenotypes with various genotypes and suggested the importance of HH PCP cilia and WNT signaling pathways [6]. These researchers also found that specific genes regulating these complex pathways had mutations that caused manifestations of myelomeningocele. This means that if these signaling pathways are modified, there are chances that myelomeningocele will come about in the patient [6].

Pathophysiology
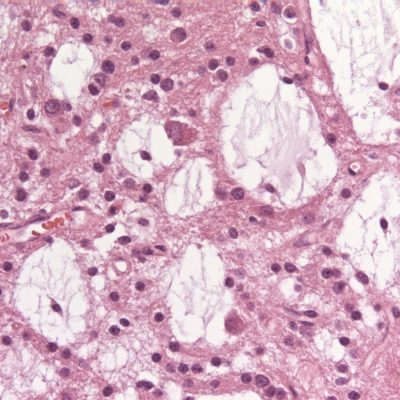
One of the factors being associated with the development of myelomeningocele is a deficiency, in folate which is considered to be a type of vitamin. Scientific studies have found evidence that vitamin deficiencies in folic acid play a factor in causing neural tube defects [7]. Multivitamin therapy with folic acid was shown to prevent tube defects, including myelomeningocele [7], before pregnancy. Thus, this underscores the need to ensure that a pregnancy will have proper intake of folate as a means of lessening the risk for myelomeningocele. Beyond deficiency, certain factors that can contributory to incidence and development exist for myelomeningocele. Such influences may be due to environmental influences and interruptions in development [8]. However, how these factors may combine to cause myelomeningocele has not yet been fully established.
The natural course of myelomeningocele is characterized by a deterioration of impairments, which may be complicated by hydrocephalus and Arnold Chiari malformation [8]. Hydrocephalus: a condition where there is an accumulation of fluid in the brain. It is a complication commonly associated with myelomeningocele. Surgical intervention is usually necessary to reroute the fluid by inserting a shunt [8]. Another more common association with myelomeningocele is Arnold Chiari malformation where there is herniation (bulging) of parts of the brain called cerebellum and brainstem through an opening at the base of the skull known as foramen magnum 8. These days, over the years there has been growing interest to perform surgery for myelomeningocele while still inside the womb as a potential treatment option.
This procedure involves the closing of a defect in a growing fetus. Preliminary studies have shown that the repair of the defect in utero may have the potential to reduce the burden, of shunt-dependent hydrocephalus treatment and even improve leg function [8]. However, broad studies are required to establish the long-term effects of in-utero intervention and to determine the critical time and method, of such repairs [8].
Clinical presentation
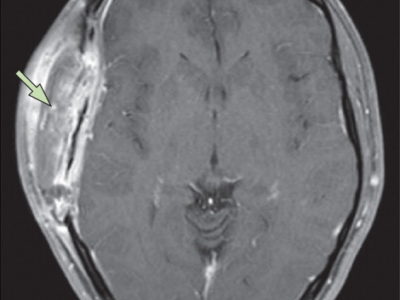
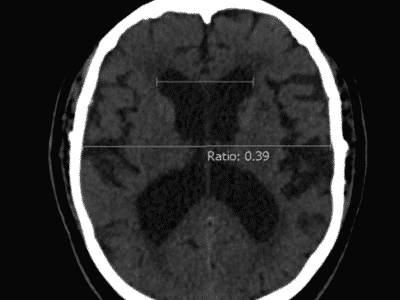
The way myelomeningocele is shown can vary depending on how severe and where the defect is located. One common clinical feature of myelomeningocele is hydrocephalus, which happens when cerebrospinal fluid accumulates in the brain. Doctors can detect this by looking for things, like an increased head circumference for a baby’s age bulging spots on the skull, or certain measurements in imaging tests [9].
Hydrocephalus can further result in difficulty swallowing, noisy breathing or stridor, stops and starts in breathing, or apnoea. Bradycardia or slowing down of the heart rate. All the symptoms mentioned above indicate Chiari malformation [10]. One more complication of myelomeningocele includes syringomyelia which means the fluid-filled cavity present within the cord. This is due to fluid movements as a result of a defect brought by myelomeningocele [11]. In the presence of syringomyelia along with ventricles or Chiari malformation symptoms, it could further affect the myelomeningocele clinical manifestations. Other than hydrocephalus and syringomyelia, myelomeningocele has other possible nerve-related problems. This is due to an unknown exact cause. It may be caused by pressure on nerves, compression of the part of the brainstem, or an abnormal development of certain parts of the brain [10]. Due to these cranial nerve abnormalities, symptoms may develop in a child, such as difficulties in swallowing, noisy breathing or stridor, and other respiratory complications.
A patient with myelomeningocele generally presents with symptoms of hydrocephalus, syringomyelia, and abnormalities of nerves. These complications need to be identified and treated for better quality of life in patients suffering from myelomeningocele. The routine symptoms observed are motor dysfunction, sensory dysfunction, bowel and bladder dysfunction, and musculoskeletal deformity [12]. Motor defects are the significant clinical features of myelomeningocele. In one study, in a fetal myelomeningocele model, the use of PMSCs resulted in significant improvement in neurological function at birth. 67% of sheep treated with PMSCs were able to move independently, whereas no sheep treated with vehicle alone were able to move [12]. This shows that PMSCs can improve paralysis in children with myelomeningocele.
Workup and Investigations
Investigations of myelomeningocele involve a variety of diagnostic tests and consults. In examining myelomeningocele, an important diagnostic tool is the use of fetal MRI.
Mangels et al. (2000) showed that prenatal MRI represents an excellent and non-invasive technique for studying the fetal “CNS” anatomy [13]. The investigators found that fetal MRI, even without anesthesia, produces very good image quality with a minor interobserver variation in grading ventricular dilatation and hindbrain herniation, though the spinal lesion was misdiagnosed and mislocated. Fetal MRI surpassed ultrasonography in uncovering posterior fossa anatomy but was equal in the assessment of hydrocephalus and the level and nature of the spinal lesion. The study concluded that incorporating fetal MRI into the routine diagnostic work-up may need further development in speed and resolution [13]. Apart from imaging, assessment of body composition and fat distribution assumes significance about myelomeningocele, especially in juveniles and adolescents. Mueske et al. (2014) conducted a study in which it was found that children with myelomeningocele had increased total body fat and leg fat compared to their peers [14]. This finding indicates the importance of an exact assessment of body composition, which steers treatment and decision-making because obesity can lead to serious health conditions in individuals affected by myelomeningocele 14. Similarly, prenatal diagnosis and counseling are very valuable in evaluating myelomeningocele. According to Meller et al. (2021), prenatal diagnostic study needs to be conducted for the cases that might be suffering from myelomeningocele 15. Prenatal diagnosis allows for early detection of the condition, which, in turn, can help provide appropriate counseling to parents about prognosis, complications that might arise, and treatment options available, including fetal surgery [15].
Management
The management of myelomeningocele has been well-studied, in surgery. Antenatal myelomeningocele surgery has some benefits. It also entails risks, to both the mother and fetus compared to surgical repair after birth [16]. A multicenter study found that surgery at a gestational age and amniotic membrane separation were some of the conditions that increased the risk for membrane rupture [16]. Oligohydramnios, which is defined by levels of fluid is associated with a higher risk of preterm birth [16]. First-time motherhood (nulliparity) is also a risk factor for hysterectomy during delivery [16]. A systematic review of postnatal surgical repair methods for myelomeningocele, as investigated in the MOMS trial, stresses the need for follow-up and further randomized trials to investigate possible complications and advantages [1]. This analysis encompassed 27 articles published between 2011 and 2021 that met inclusion criteria [1]. With growing experience and advancements in laparoscopic fetal examination techniques, there is potential for enhanced outcomes in managing myelomeningocele and related conditions while minimizing risks, for both mother and fetus [1].
Goals
The goals of myelomeningocele reconstruction can be summarized as follows:
1. Improvement of outcomes; Prenatal repair of myelomeningocele has been shown to lead to functional outcomes compared to postnatal repair. Children who underwent repair attained scores on tests assessing their functionality and were more likely to walk without the need, for orthotics or assistive devices [17].
2. Reduced herniation; Intrauterine repair of myelomeningocele has demonstrated a reduction in the incidence of hindbrain herniation [18]. This is important because hindbrain herniation may lead to complications and disabilities.
3. Reduction of hydrocephalus; Intrauterine repair has also been seen to reduce, though moderately, the incidence of shunt dependence. [18]. This is important because hydrocephalus is one of the complications of myelomeningocele and may require shunt placements and revisions.
4. Improvement of the quality of life; Parents of children who had gone through repair reported scores regarding quality of life compared to parents who chose postnatal repair [17].
Myelomeningocele reconstruction aims to improve the quality of life for the child and the family. It is worth noting that while myelomeningocele reconstruction may impact herniation, hydrocephalus, and functional outcomes, it does not necessarily improve leg function 18. Thus, it is of paramount importance to manage expectations and counsel the patients appropriately.
Prognosis
The prognosis among patients with myelomeningocele may vary in many ways, including the size and number of abnormal changes in the bone marrow and any associated condition, including hydrocephalus water. Other conditions that may further impede their recovery will be surgery time. The work of Houtrow et al. (2020), discussed functional outcomes among children with prenatal myelomeningocele surgery. In children in the prenatal repair group, functional outcomes were significantly improved. The children in the prenatal group were more likely to walk without orthotics or assistive devices, with higher rehabilitation assessments with lower rates of the posterior encephalocele and shunt-related complications. Parents also reported a higher quality of life for children who had surgical repair before birth.
The results indicate that repair, in myelomeningocele may result in better outcomes and an improved quality of life for affected individuals [17]. Another study by Kshettry et al.
(2014) researched trends and determinants of outcomes for myelomeningocele individuals in the United States. The study indicates that 80% of individuals with myelomeningocele undergo shunt placement [19]. Shunt-related complications, such as revision are also frequent with 51 55% of the patients needing revision within their year of life. Further, the study has elucidated health care disparities and significantly points out that the risk of hospital mortality among non-white patients is high due to either differences in illness severity or service access. These findings demonstrate the importance of monitoring and management in individuals affected with myelomeningocele [19].
In summary, multiple factors predict the prognosis of individuals with myelomeningocele. Prenatal repair has been associated with outcomes and quality of life [17]. However, in light of the rate of shunt placement and associated complications as well as potential disparities in healthcare provision, vigilant monitoring and effective management strategies are essential to maintain hydrocephalus in individuals with spinal cord hernias [19].