Article topic: Phases and Phenotypes of Multiple Sclerosis
Author: Bayan Khasawneh
Editor: Ethar Hazaimeh
Keywords: Multiple Sclerosis, Phases, Phenotypes, Relapsing, Remitting.
Overview
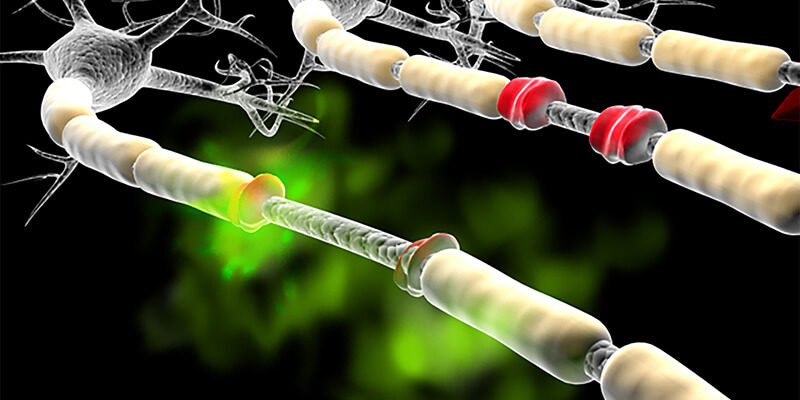
Multiple sclerosis (MS) is a chronic, non-traumatic, disabling inflammatory disease of the central nervous system that leads to demyelination and neurodegeneration. (1) MS usually affects young adults and the incidence of it is increasing worldwide. Multiple sclerosis has been classified as an organ-specific T-cell mediated autoimmune disease. It is considered a two-stage disease, with early inflammation responsible for relapsing-remitting disease and delayed neurodegeneration causing non-relapsing progression, i.e. secondary and primary progressive MS.
Pathogenesis and Etiology
The underlying cause of Multiple Sclerosis remains uncertain. There are many factors that are believed to increase the susceptibility to have MS; including genetic factors (HLA-DRB1*15), and a few environmental factors, such as Vitamin D deficiency or ultraviolet B light (UVB) exposure, Epstein-Barr virus (EBV) infection, smoking and obesity. (2)
The characteristic pathological hallmark of MS is periventricular inflammatory lesions, forming demyelinating plaques. The inflammatory infiltrates contain T-lymphocytes, dominated by MHC class I restricted CD8+ T-cells; B-cells and plasma cells are also present but in smaller numbers. As a consequence of inflammation, Oligodendrocytes are damaged and demyelination occurs. Axons are initially reasonably intact, but as the disease advances, irreversible axonal damage occurs.
Phases and disease course in Multiple Sclerosis
The disease course in MS is characterized by the interaction of two phenomena: relapses and progression. At different stages of the disease, these manifestations may overlap. Approximately 80% of patients eventually evolve to the progressive phase of the disease, Each phase of MS is further defined as active or inactive at any given time. (3)
Multiple sclerosis (MS) was classified as relapsing-remitting, primary progressive, secondary progressive, or progressive relapsing as of 1996. With a better understanding of MS and its pathology, several clinical characteristics have been re-examined and the main recommendations of the 2013 revisions were provided. After that, the Clinically isolated syndrome was added to the clinical course description, and progressive relapsing MS was eliminated.
All types of MS should be further subdivided into two groups: active and non-active, The occurrence of a clinical relapse or the presence of new T2 or gadolinium-enhancing lesions over a set length of time, is considered active MS (contrast-enhancing T1-hyperintense lesions, new T2-hyperintense lesions, or enlarging T2-hyperintense lesions). (4) The absence of active disease for a period of one year or more is referred to as “No evidence of disease activity” (NEDA). (5)
Relapses, Pseudorelapses and Progression
Relapses suggest an acute inflammatory demyelination episode with or without axonal damage. The biological basis for why some MS presentations are asymptomatic is currently unknown. Asymptomatic relapse usually peaks over days to weeks, and then a recovery period begins, this phase of recovery is referred to as remission, and it includes some restoration of myelin and axonal integrity.
After a relapse, maximum clinical recovery usually occurs within the first three months and seldom lasts longer than six months. The majority of patients return to baseline clinically; some recover partially, and a small percentage of patients do not recover at all.
A recurrence of symptoms from a previous clinical relapse or a subclinical disease is known as a Pseudorelapse. A pseudorelapse most likely means that the earlier CNS damage was not fully recovered. A pseudorelapse can be triggered by any stress to the neurological system that exceeds a threshold that the damaged nervous system can withstand (e.g., heat, infection, exercise, fatigue).
If symptoms attributed to a pseudorelapse last longer than 24 hours or do not improve within a few days despite identifying and treating a potential trigger (e.g., urinary tract infection), an MRI should be obtained to distinguish it from a symptomatic relapse recurrent in the same location or close vicinity on the same neural pathway.
Progression is the gradual and permanent deterioration of neurologic function over time. Progressive axonal damage or loss is the most common underlying pathology. Because imaging technology is improving, detecting subclinical progression will become a more essential part of the therapeutic decision-making process in MS in the future.
- Relapsing-Remitting Phase
The relapsing-remitting phase begins in many people as subclinical activity, usually long before they present with a clinically isolated syndrome. A relapse causes nerve signal disruption due to new injury in the brain or spinal cord. As a result, the patient may have new symptoms or the recurrence of previous ones. Relapses last at least 24 hours and it will be followed by a remission. During remission, symptoms partly or completely go away.
Multiple clinically distinct events affecting different areas of the CNS separated in time (at least 1 month apart) are required for the diagnosis of relapsing-remitting MS. The term “Dissemination in time and space” refers to this core operational diagnostic rule. However, in practice, typical lesions in location, shape, and orientation must be seen on MRI. Sequential lesions may develop in less than 1-month intervals in some patients with severe presentations.
Activity status is used to describe whether the patient is having active or inactive relapsing-remitting MS during a specific time period.
- Progressive Phase
After one year of clinical progression, the progressive phase of MS is assumed to be established. Because of the temporal overlap between the relapsing and progressive phases, patients can still have an active disease with symptomatic relapses or asymptomatic MRI activity during this phase. After that, the patient is classified as having active progressive MS or inactive progressive MS.
The presence or absence of prior clinical relapses before the onset of a progressive disease course divides the progressive phase into subgroups. The term Primary progressive MS refers to a radiologically isolated syndrome that progresses. (6)
Secondary progressive MS refers to Relapsing-Remitting MS followed by the progressive phase. If solitary sclerosis leads to a progressive phase, it is described as progressive solitary sclerosis. (7)(8)
Understanding the primary progressive MS diagnosis should be given special consideration because, in most cases, patients have evidence of MRI activity compatible with a previous radiologically isolated syndrome at the time of primary progressive MS presentation, even if a formal diagnosis of the radiologically isolated syndrome had not been established previously. However, it is reasonable to believe that if these patients had been imaged earlier, they would have been diagnosed with a radiologically isolated syndrome.
The differences between the progressive MS subtypes do not seem to be because of different progression mechanisms but rather because of why the disease activity remains subclinical in some individuals.
- Clinically Isolated Syndrome
The clinically isolated syndrome is used after a first-ever or single clinical incident. It becomes clinically definite relapsing-remitting MS when a patient has another clinical relapse (clinically active disease). (9)
MRI activity can meet “dissemination in time and space” criteria without the need for any further clinical relapse, according to the 2016 Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) and 2017 McDonald criteria updates. (10)(11)
The clinically isolated syndrome can be further subgrouped into two categories. Patients with solitary sclerosis have imaging results that do not meet the minimal MRI criterion for an MS diagnosis at the time of clinically isolated syndrome (at least three of the four imaging criteria), but the existing CNS lesions are unexplained by any other pathology and are typical of MS in location, orientation, and shape. When a patient with solitary sclerosis meets the MRI criteria for an MS diagnosis (at least three of the four imaging criteria)(12), the diagnosis of single-attack MS may be utilized.
Conclusion
Multiple sclerosis is a demyelinating disease of the Central Nervous System (CNS); including the brain and spinal cord. Every patient begins with a period of high risk, which is dictated by genetic and environmental factors. This is followed by the presymptomatic active phases of MS, the relapsing-remitting phase, and, eventually, the progressive phase of MS in the majority of individuals.
Therefore, MS is a dynamic progression of phenotypic phases. Each phase is associated with a change in disability worsening caused by poorly recovered relapses, progression, and non-MS-related causes.
As a result, it’s clear that different types of interventions, such as currently existing disease-modifying therapies, future reparative or regeneration therapies, or even preventive methods, have ideal windows of opportunity. For existing disease-modifying therapies, the best time is earlier in life, when the disease is more likely to be active. However, our current treatment strategy of escalating from lesser to stronger medications may not be the right thing to do.
References...














A great article Dr. Bayan, waiting your coming ones.