
Article topic: Neuromyelitis Optica Spectrum Disorder (NMOSD)
Author name: Nadine Absy
Keywords: Neuromyelitis optica, Aquaporin 4, antibody, Devic’s disease
Overview :
Neuromyelitis optica spectrum disorder (NMOSD) is a rare but serious inflammatory demyelinating disease of the central nervous system. It is characterized by its classical clinical presentation of myelitis (inflammation of the long segments of the spinal cords) and optic neuritis (often severe and bilateral). The disease may also present with brainstem syndromes, including but not limited to, area postrema syndrome in which patients suffer from episodes of intractable nausea, vomiting and hiccups. (1) Previously, the disease was referred to as Devic’s disease since it was first described by Eugène Devic and his student Fernand Gault in 1894. (2)
Epidemiology:
While NMOSD may occur at any age, the mean age of onset is around 40 years, and about 15-20% of patients present to pediatricians or geriatric physicians. In accordance with other autoimmune diseases, females have a higher susceptibly to have NMOSD-AQP4 than males (3:1-9:1).(3,4)
Interestingly, in regions where multiple sclerosis had a lower prevalence, such as Asia, NMSOD represented a greater proportion of central nervous system demyelinating diseases. This is important to note since the disease should be considered in the differential diagnosis when assessing patients from those regions.
Pathogenesis and Etiology
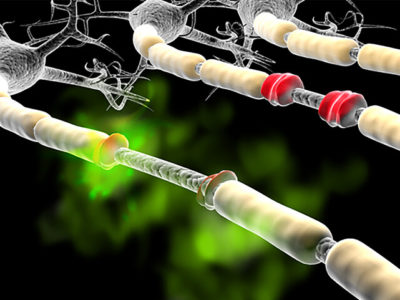
It is known that the majority of patients with NMOSD have AQP4-IgG, those immunoglobulins can pass the blood brain barrier and bind to AQP4 channels that are located on the end-feet of astrocytes. Their binding initiates a cascade of immunologically mediated inflammation that causes secondary demyelination.(5)
The cascade involves the recruitment and activation of the complement system, which results in complement-dependent-cytotoxicity. Antibody-dependent cytotoxicity is also triggered, by the activation of effector cells.(6)
Studies conducted on biopsies and autopsies of patients with NMOSD demonstrate that lesions show loss of myelin, infiltration of inflammatory cells and have both axonal and astrocytic loss. (7) Contrary to MS (multiple sclerosis), AQP4 immunostaining is not found within NMSOD lesions and there are no cortical lesions.(8)
Diagnosis
NMSOD’s neurologic manifestations may mimic those of multiple sclerosis. It is vital to distinguish between these two disorders owing to the differences in both therapeutic and diagnostic implications. This distinction was made possible by the discovery of a specific biomarker for neuromyelitis optica (NMO), namely the aquaporin-4 water channel (AQP4) which was detected through AQP4-Abs.(9)
The current classification (NMOSD), resulted from the recognition that patients can have more restricted forms of the disease (e.g.: recurring transverse myelitis that is not accompanied by optic neuritis) or symptoms surpassing the optic nerve and spinal cord (e.g.: area postrema syndrome). (10)
It is noteworthy to mention that around 20% of patients are seronegative for AQP4-IgG, and a proportion of those seronegative patients have myelin oligodendrocyte glycoprotein antibodies (i.e.: MOG-IgG seropositive).(11) Since AQP4 NMOSD is a disease of astrocytes while MOG NMOSD is a disease of oligodendrocytes, certain controversies have arisen regarding what basis to consider for diagnosis.
Diagnostic criteria are divided into syndrome-based (NMSOD) or biomarker-based (AQP4-IgG, MOG-IgG), currently the 2015 International Panel for NMO Diagnosis criteria is used , as the name implies, a set of criteria used to diagnose (NMOSD) (10,12). It based on a combination of clinical, laboratory, and neuroimaging findings, Table 1.
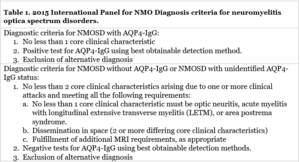

Figure 1.a Transverse myelitis, Case courtesy of Assoc Prof Frank Gaillard(13)

Figure 1.b Transverse myelitis, Case courtesy of Assoc Prof Frank Gaillard.(14)
Figure 1 demonstrates the longitudinally extensive involvement of the cervicothoracic cord. Spinal cord lesion (LESCL) of an abnormal T2 signal with cord swelling. The central cord is involved. No hemorrhage.

Figure 2. The cord demonstrates a longitudinaly extensive spinal cord lesion, with high T2 signal involving almost the entire cord. Case courtesy of Assoc Prof Frank Gaillard.
Clinical presentation:
Principally, the three classic clinical presentations for NMOSD are: optic neuritis, transverse myelitis, and area postrema syndrome.(15) Most patients have a relapsing course, and some patients have severe attacks that result in lasting neurological deficits that persist even after long periods of remission. A distinction that may be significant in separating MS from NMSOD, is that in the latter a secondary progressive course is exceedingly rare.(16)
The bouts of transverse myelitis may present with conventional findings of myelitis including: numbness, weakness, bladder or bowel dysfunction, and Lhermitte phenomenon (electric shock like sensation extending down the spine or extremities when the neck is flexed). The progression of these symptoms beyond 1 month should warrant concerns for alternative diagnosis. Another point to highlight in the differences between MS and NMOSD is that unlike MS the attacks of myelitis in NMOSD are often disabling. Episodes of painful involuntary flexion called tonic spasms may occur after episodes of myelitis. Those tonic spasms are triggered by movement, they last less than 1 minute, and respond well to low doses of carbamazepine and occur frequently with NMSOD. (17)
Area postrema syndrome, the third cardinal feature, results in bouts of intractable nausea and vomiting that may or may not be accompanied by hiccups. (10) The bouts may be a patient’s first presentation and may cause the patient to initially believe the condition is due to a pathology in the gastrointestinal system. (18) furthermore, they may occur in isolation, be accompanied by other brainstem features or develop into a myelitis episode.(19)At times, NMOSD presents in paraneoplastic contexts.(5)
Autoimmune disorders, such as systemic lupus erythematos, Sjögren syndrome, and antiphospholipid antibody syndrome, were found to frequently coincide with NMSOD. This association warrants AQP4-IgG testing if the patient presents with optic neuritis, transverse myelitis, or intractable vomiting in patients with any of these systemic autoimmune disorders. If a positive result ensues, this would confirm the existence of an autoimmune neurologic disorder along with the rheumatologic disorder, in lieu of a neurologic manifestation of one of these disorders.(20) Noticeably, patients who have both NMSOD and antiphospholipid antibodies or the syndrome might have an increased risk of have developing clotting disorders (resulting in deep vein thrombosis, miscarriages and other manifestations).(21) Myasthenia gravis (MG) was also found to coexist frequently with NMSOD. Usually, MG would precede a NMSOD diagnosis by years or decades.(22)
As mentioned before 20% of patients are seronegative for AQP4 most of those patients have MOG antibodies. Other than NMSOD that is seronegative for AQP4-IgG these patients present with optic neuritis, acute disseminated encephalomyelitis, transverse myelitis, and brainstem demyelinating episodes.
Summary of clinical features:
Cardinal clinical features (15,18,23,24)
- Transverse myelitis, classically longitudinally extensive (involving three or more vertebral segments; frequently followed by tonic spasms and rarely elements of pain or pruritus present)
- Optic neuritis (usually severe and may be bilateral at times)
- Bouts of intractable nausea and vomiting or hiccups due to involvement of area postrema.
Other Clinical Features(25–34)
- Narcolepsy
- Hydrocephalus
- Syndrome of inappropriate secretion of antidiuretic hormone (SIADH)
- Differing hypothalamic presentations (e.g., anorexia)
- Acute myopathy with elevated serum CK levels (hyperCKemia)
- Brainstem syndromes (such as, ophthalmoplegia, hearing loss, opsoclonus or myoclonus)
- Myeloradiculitis
- Encephalopathy (similar to acute disseminated encephalomyelitis; or posterior reversible encephalopathy syndrome)
- Cognitive dysfunction (of subcortical pattern)
Treatment and Management
It is important to keep in mind while approaching the management of NMSOD, that the disorder has high attack related disability, poor prognosis, and a generally high risk of mortality in patients who remain untreated.(35)
The principles of treatment are based on the evidence on the role of humoral immunity in the pathogenesis of the disease
- Acute attacks:
Initially patients might be given a high dose of intravenous methylprednisolone, which is given daily over 3-5 days in 1 gram doses. If patients suffer from symptoms that are severe and unresponsive to glucocorticoids, the suggested “rescue” treatment is plasma exchange.(36) This management protocol applies to both seronegative and seropositive NMOSD.
2. Attack prevention:
Recurrent attacks are one of the features of NMOSD; these attacks often lead to accumulated disability since there is little to no recovery after each attack unlike MS. Hence, long-term immunotherapy is indicated for those diagnosed with NMOSD. In patients who are seropositive for AQP4-IgG treatment with monoclonal antibodies such as eculizumab, inebilizumab and satralizumab is recommended, rather than other immunosuppressant drugs.(36)However, many clinicians use rituximab, mycophenolate mofetil, azathioprine and other immunotherapies. Drugs containing antibodies targeting IL-6 which plays a role in the pathogenesis of the disease are being trialed.(37)
It is recommended that immunosuppression is continued for at least five years in patients who have AQP4 antibodies, even if the patient had only one previous attack since those patients would have a high risk of relapse or developing NMOSD.(38) Due to the devastating nature of the disease, some physicians recommend life-long therapy as the appropriate way of approach. Others suggest that the severity of attacks and disability should guide physicians to treatment durations.
The risks of long-term immunosuppression are not yet established well enough. Retinal infections caused by opportunistic microorganisms such as toxoplasmosis and cytomegalovirus may present similarly to optic neuritis attacks.(39) Studies are needed to explore whether maintenance immunotherapy can be stopped safely, consequently reducing the risk associated with long-term suppression of the immunity. Currently, other approaches are under development amongst which are: AQP4 blocking antibodies used on animal models and inhibitors of neutrophils (sivelstat) or eosinophils (cetirizine). (40)
Risk Factors:
No well-established risk factors are known. However, patients with NMOSD are likely to have a history of other autoimmune diseases, malignancy, or recent non-neurological systemic diseases all of which may trigger the onset of NMOSD or predispose the patient to developing the disorder.(41)
Prognosis:
Recurrent attacks lead to the accumulation of motor, sensory, visual, and bladder deficits. Thus, causing a stepwise deterioration in the patient’s condition. Attacks or relapses usually worsen over a number of days and patients take several weeks to months to recover, though never fully since attacks leave significant sequels each time. A worse outcome is expected according to the number of replaces during the first two years, being older at the onset of disease, the severity of the first attack, and if the patient has associated autoimmune disorders.(42–44) It is noteworthy to mention that these prognostic factors require confirmation via larger prospective studies.
Respiratory failure due to neurogenic causes is a frequent secondary cause of mortality. In general, mortality rates tend to be high in patients with NMOSD. (36)Due to the progress in both the diagnosis and treatment of NMOSD patients, mortality rates are expected to decrease. In patients with optic neuritis that is recurrent, retrospective evidence has shown that seropositivity for AQP4-IgG is linked to worse visual outcomes.(24)
Recent updates (clinical trials)
A recent study that compared the usage of intravenous methylprednisolone (IVMP) with succeeding plasma exchange (PLEX) that is used as an add-on and the combination of concurrent IVMP and PLEX in patients suffering from severe attacks of NMOSD. The study found that early treatment with PLEX ought to be implemented in those with severe acute attacks since the outcome and response were better than their counterparts. (45)
Another recent clinical trial explored the efficacy and safety of satralizumab as monotherapy in NMOSD found that the immunosuppressive agent reduced the rate of relapse compared with placebo and had an overall satisfactory safety profile. Both seropositive and seronegative patients were included in the trial. (46)
References
- Huda S, Whittam D, Bhojak M, Chamberlain J, Noonan C, Jacob A. Neuromyelitis optica spectrum disorders. Clin Med. 2019 Mar;19(2):169–76.
- Jarius S, Wildemann B. The history of neuromyelitis optica. J Neuroinflammation. 2013 Jan;10:8.
- Hor JY, Asgari N, Nakashima I, Broadley SA, Leite MI, Kissani N, et al. Epidemiology of Neuromyelitis Optica Spectrum Disorder and Its Prevalence and Incidence Worldwide. Front Neurol. 2020;11:501.
- Quek AML, McKeon A, Lennon VA, Mandrekar JN, Iorio R, Jiao Y, et al. Effects of age and sex on aquaporin-4 autoimmunity. Arch Neurol. 2012 Aug;69(8):1039–43.
- Pittock SJ, Lennon VA. Aquaporin-4 autoantibodies in a paraneoplastic context. Arch Neurol. 2008 May;65(5):629–32.
- Wu Y, Zhong L, Geng J. Neuromyelitis optica spectrum disorder: Pathogenesis, treatment, and experimental models. Mult Scler Relat Disord. 2019 Jan;27:412–8.
- Lucchinetti CF, Guo Y, Popescu BFG, Fujihara K, Itoyama Y, Misu T. The pathology of an autoimmune astrocytopathy: lessons learned from neuromyelitis optica. Brain Pathol. 2014 Jan;24(1):83–97.
- Popescu BFG, Guo Y, Jentoft ME, Parisi JE, Lennon VA, Pittock SJ, et al. Diagnostic utility of aquaporin-4 in the analysis of active demyelinating lesions. Neurology. 2015 Jan;84(2):148–58.
- Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet (London, England). 2004 Dec;364(9451):2106–12.
- Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015 Jul;85(2):177–89.
- Waters PJ, McKeon A, Leite MI, Rajasekharan S, Lennon VA, Villalobos A, et al. Serologic diagnosis of NMO: a multicenter comparison of aquaporin-4-IgG assays. Neurology. 2012 Feb;78(9):665–71; discussion 669.
- Hacohen Y, Palace J. Time to separate MOG-Ab-associated disease from AQP4-Ab-positive neuromyelitis optica spectrum disorder. Neurology [Internet]. 2018 May 22;90(21):947 LP – 948. Available from: http://n.neurology.org/content/90/21/947.abstract
- radiopedia. Transverse myelitis.
- axial section.
- Wingerchuk DM, Hogancamp WF, O’Brien PC, Weinshenker BG. The clinical course of neuromyelitis optica (Devic’s syndrome). Neurology. 1999 Sep;53(5):1107–14.
- Wingerchuk DM, Pittock SJ, Lucchinetti CF, Lennon VA, Weinshenker BG. A secondary progressive clinical course is uncommon in neuromyelitis optica. Neurology. 2007 Feb;68(8):603–5.
- Kim S-M, Go MJ, Sung J-J, Park KS, Lee K-W. Painful tonic spasm in neuromyelitis optica: incidence, diagnostic utility, and clinical characteristics. Arch Neurol. 2012 Aug;69(8):1026–31.
- Apiwattanakul M, Popescu BF, Matiello M, Weinshenker BG, Lucchinetti CF, Lennon VA, et al. Intractable vomiting as the initial presentation of neuromyelitis optica. Ann Neurol. 2010 Nov;68(5):757–61.
- Asgari N, Skejoe HPB, Lennon VA. Evolution of longitudinally extensive transverse myelitis in an aquaporin-4 IgG-positive patient. Neurology [Internet]. 2013 Jul 2;81(1):95 LP – 96. Available from: http://n.neurology.org/content/81/1/95.abstract
- Wingerchuk DM, Weinshenker BG. The emerging relationship between neuromyelitis optica and systemic rheumatologic autoimmune disease. Mult Scler. 2012 Jan;18(1):5–10.
- Guerra H, Pittock SJ, Moder KG, Fryer JP, Gadoth A, Flanagan EP. Frequency of Aquaporin-4 Immunoglobulin G in Longitudinally Extensive Transverse Myelitis With Antiphospholipid Antibodies. Mayo Clin Proc. 2018 Sep;93(9):1299–304.
- McKeon A, Lennon VA, Jacob A, Matiello M, Lucchinetti CF, Kale N, et al. Coexistence of myasthenia gravis and serological markers of neurological autoimmunity in neuromyelitis optica. Muscle Nerve. 2009 Jan;39(1):87–90.
- Kanamori Y, Nakashima I, Takai Y, Nishiyama S, Kuroda H, Takahashi T, et al. Pain in neuromyelitis optica and its effect on quality of life: a cross-sectional study. Neurology. 2011 Aug;77(7):652–8.
- Matiello M, Lennon VA, Jacob A, Pittock SJ, Lucchinetti CF, Wingerchuk DM, et al. NMO-IgG predicts the outcome of recurrent optic neuritis. Neurology. 2008 Jun;70(23):2197–200.
- Viegas S, Weir A, Esiri M, Kuker W, Waters P, Leite MI, et al. Symptomatic, radiological and pathological involvement of the hypothalamus in neuromyelitis optica. J Neurol Neurosurg Psychiatry. 2009 Jun;80(6):679–82.
- Suzuki K, Nakamura T, Hashimoto K, Miyamoto M, Komagamine T, Nagashima T, et al. Hypothermia, hypotension, hypersomnia, and obesity associated with hypothalamic lesions in a patient positive for the anti-aquaporin 4 antibody: a case report and literature review. Arch Neurol. 2012 Oct;69(10):1355–9.
- Iorio R, Lucchinetti CF, Lennon VA, Costanzi C, Hinson S, Weinshenker BG, et al. Syndrome of inappropriate antidiuresis may herald or accompany neuromyelitis optica. Neurology. 2011 Oct;77(17):1644–6.
- Baba T, Nakashima I, Kanbayashi T, Konno M, Takahashi T, Fujihara K, et al. Narcolepsy as an initial manifestation of neuromyelitis optica with anti-aquaporin-4 antibody. Vol. 256, Journal of neurology. Germany; 2009. p. 287–8.
- Suzuki N, Takahashi T, Aoki M, Misu T, Konohana S, Okumura T, et al. Neuromyelitis optica preceded by hyperCKemia episode. Neurology. 2010 May;74(19):1543–5.
- Kremer L, Mealy M, Jacob A, Nakashima I, Cabre P, Bigi S, et al. Brainstem manifestations in neuromyelitis optica: a multicenter study of 258 patients. Mult Scler. 2014 Jun;20(7):843–7.
- Hage RJ, Merle H, Jeannin S, Cabre P. Ocular oscillations in the neuromyelitis optica spectrum. J neuro-ophthalmology Off J North Am Neuro-Ophthalmology Soc. 2011 Sep;31(3):255–9.
- Takai Y, Misu T, Nakashima I, Takahashi T, Itoyama Y, Fujihara K, et al. Two cases of lumbosacral myeloradiculitis with anti-aquaporin-4 antibody. Neurology. 2012 Oct;79(17):1826–8.
- Blanc F, Noblet V, Jung B, Rousseau F, Renard F, Bourre B, et al. White matter atrophy and cognitive dysfunctions in neuromyelitis optica. PLoS One. 2012;7(4):e33878.
- Clardy SL, Lucchinetti CF, Krecke KN, Lennon VA, O’Toole O, Weinshenker BG, et al. Hydrocephalus in neuromyelitis optica. Neurology. 2014 May;82(20):1841–3.
- Collongues N, de Seze J. Current and future treatment approaches for neuromyelitis optica. Ther Adv Neurol Disord. 2011 Mar;4(2):111–21.
- Sellner J, Boggild M, Clanet M, Hintzen RQ, Illes Z, Montalban X, et al. EFNS guidelines on diagnosis and management of neuromyelitis optica. Eur J Neurol. 2010 Aug;17(8):1019–32.
- Araki M, Matsuoka T, Miyamoto K, Kusunoki S, Okamoto T, Murata M, et al. Efficacy of the anti-IL-6 receptor antibody tocilizumab in neuromyelitis optica: a pilot study. Neurology. 2014 Apr;82(15):1302–6.
- Carroll WM, Fujihara K. Neuromyelitis optica. Curr Treat Options Neurol. 2010 May;12(3):244–55.
- George JS, Leite MI, Kitley JL, Jones N, Cortes N, Donati M, et al. Opportunistic infections of the retina in patients with aquaporin-4 antibody disease. JAMA Neurol. 2014 Nov;71(11):1429–32.
- Flanagan EP, Weinshenker BG. Neuromyelitis optica spectrum disorders. Curr Neurol Neurosci Rep. 2014 Sep;14(9):483.
- Akaishi T, Takahashi T, Fujihara K, Misu T, Abe M, Ishii T, et al. Risk factors of attacks in neuromyelitis optica spectrum disorders. J Neuroimmunol. 2020 Jun;343:577236.
- Ghezzi A, Bergamaschi R, Martinelli V, Trojano M, Tola MR, Merelli E, et al. Clinical characteristics, course and prognosis of relapsing Devic’s Neuromyelitis Optica. J Neurol. 2004 Jan;251(1):47–52.
- Wingerchuk DM, Weinshenker BG. Neuromyelitis optica: clinical predictors of a relapsing course and survival. Neurology. 2003 Mar;60(5):848–53.
- Kitley J, Leite MI, Nakashima I, Waters P, McNeillis B, Brown R, et al. Prognostic factors and disease course in aquaporin-4 antibody-positive patients with neuromyelitis optica spectrum disorder from the United Kingdom and Japan. Brain. 2012 Jun;135(Pt 6):1834–49.
- Songthammawat T, Srisupa-Olan T, Siritho S, Kittisares K, Jitprapaikulsan J, Sathukitchai C, et al. A pilot study comparing treatments for severe attacks of neuromyelitis optica spectrum disorders: Intravenous methylprednisolone (IVMP) with add-on plasma exchange (PLEX) versus simultaneous ivmp and PLEX. Mult Scler Relat Disord. 2020 Feb;38:101506.
- Traboulsee A, Greenberg BM, Bennett JL, Szczechowski L, Fox E, Shkrobot S, et al. Safety and efficacy of satralizumab monotherapy in neuromyelitis optica spectrum disorder: a randomised, double-blind, multicentre, placebo-controlled phase 3 trial. Lancet Neurol. 2020 May;19(5):402–12.












Excellent