Article Topic: Miller-Fisher Syndrome
Authors: Joyce Labaky, Jim Dagher
Editors: Odette El Ghawi, Joseph Akiki
Reviewer: Ethar Hazaimeh
Keywords: Miller Fisher Syndrome, Guillain Barré Syndrome, peripheral neuropathy, autoimmune disorder
Abstract
Miller-Fisher Syndrome (MFS) is a rare, immune-mediated neurological disorder that is considered a variant of Guillain Barré Syndrome (GBS). It is primarily characterized by the clinical triad of ophthalmoplegia, ataxia, and areflexia. The pathophysiology of MFS is associated with autoantibodies, particularly anti-GQ1b antibodies, which target gangliosides at the neuromuscular junction, especially in areas rich in these gangliosides, such as the oculomotor nerves. MFS typically follows a preceding viral or bacterial infection, most commonly caused by pathogens like Campylobacter jejuni or Mycoplasma pneumoniae, which trigger an aberrant immune response leading to antibody production. Diagnostic evaluation involves the detection of anti-GQ1b antibodies, which are highly specific for MFS, and cerebrospinal fluid (CSF) analysis may reveal albuminocytologic dissociation. Electrodiagnostic studies may show reduced sensory nerve action potentials. Although MFS can cause significant neurological impairment, it is typically self-limiting and has a generally favorable prognosis, with most patients recovering fully within weeks to months. Severe complications, such as respiratory failure, are rare but can occur in some cases. Treatment typically includes intravenous immunoglobulin (IVIG) or plasma exchange therapy, both of which have been shown to accelerate recovery by modulating the immune response. Early intervention with these therapies may be beneficial, particularly in more severe cases. Long-term outcomes are generally positive, with most patients achieving full or near-full recovery.
Introduction
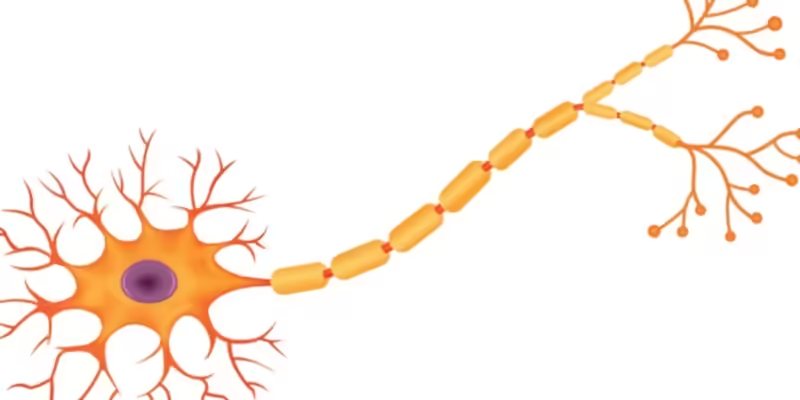
Miller Fisher Syndrome (MFS) is a rare variant of Guillain Barré Syndrome (GBS), classified as an acute immune-mediated polyneuropathy. First described as a distinct clinical entity by Charles Miller Fisher in 1956, MFS arises when the immune system mistakenly targets specific components of the peripheral nervous system, particularly gangliosides found on nerve cell membranes, such as GQ1b. This immune-mediated attack often occurs following a preceding infection, such as Campylobacter jejuni, and is associated with a range of infectious, autoimmune, and neoplastic conditions [1].
Unlike the more common GBS, which primarily affects motor neurons in the limbs and can cause ascending paralysis, MFS predominantly involves the cranial nerves, particularly those responsible for ocular motility and muscle coordination, leading to the characteristic ophthalmoplegia, ataxia, and areflexia seen in this condition.
Although MFS is rare in the general population, its prevalence shows regional variation. In the United States and Europe, it accounts for about 3% of GBS cases, whereas in Asia, the incidence is notably higher, comprising 20-25% of GBS cases, suggesting possible genetic or environmental factors influencing susceptibility [2].
Etiology and Pathogenesis
Similar to GBS, MFS is thought to result from an abnormal acute autoimmune response triggered by a preceding infection. Approximately two-thirds of cases are preceded by symptoms of an upper respiratory infection or diarrhea, with around 50% occurring after a confirmed infection. The most commonly implicated pathogens include Campylobacter jejuni, Cytomegalovirus, Epstein-Barr virus, and human immunodeficiency virus [3].
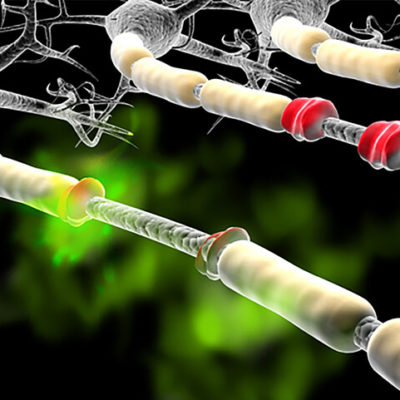
The inflammatory process in MFS is believed to be driven by molecular mimicry, where similarities between microbial antigens and peripheral nerve gangliosides activate the adaptive immune system, leading to humoral and cell-mediated lymphocyte mobilization. Numerous studies have shown that antibodies against gangliosides, particularly the anti-GQ1b antibody, are a hallmark of MFS. Once formed, these antibodies directly affect the neuromuscular junctions between cranial nerves and ocular muscles, resulting in ophthalmoparesis [4].
Clinical Presentation and Complications
Miller-Fisher Syndrome (MFS) is distinguished by a characteristic clinical triad:
- Cranial nerve involvement, primarily manifesting as ophthalmoplegia.
- Ataxia, reflecting impaired coordination and balance.
- Areflexia, indicating the absence of deep tendon reflexes.
In addition to these hallmark features, patients with MFS may experience other symptoms. Paresthesia, or numbness and tingling in the extremities, can occur, along with back pain. Some individuals may also present with signs of bulbar palsy, resulting from bilateral damage to the cranial nerve nuclei (particularly CN IX, X, XI, and XII). This can lead to dysphagia (difficulty swallowing), drooling, anarthria (inability to articulate speech), tongue fasciculations, and loss of the gag reflex [5].
The involvement of bulbar muscles and cranial nerve dysfunction in MFS further differentiates it from other Guillain-Barré syndrome (GBS) variants, highlighting the distinctive neuroanatomical pattern of impairment that primarily affects the cranial and peripheral nervous system in this condition.
Workup and Diagnosis
The workup and diagnosis of Miller-Fisher Syndrome (MFS) involve a combination of clinical evaluation, cerebrospinal fluid (CSF) analysis, serological tests, and neuroimaging to confirm the diagnosis and differentiate it from other neurological conditions, particularly Guillain-Barré Syndrome (GBS).
Lumbar Puncture and CSF Analysis
A lumbar puncture is a critical diagnostic tool in the workup of MFS.
Albuminocytologic dissociation, characterized by elevated protein levels with a normal white cell count, is typically seen. This finding reflects blood-brain barrier disruption and is a hallmark of both MFS. CSF protein levels may rise to 45-100 mg/dL or higher, though this elevation might not be apparent until after the first week of symptoms.
Normal cell counts in the presence of increased protein help rule out infectious or inflammatory processes involving the central nervous system, making this a key diagnostic criterion [5].
Serological Testing
Anti-GQ1b antibodies are highly specific for MFS and are present in up to 90% of cases. These antibodies target gangliosides, particularly those involved in the neuromuscular junctions of the oculomotor system, leading to the ophthalmoplegia seen in MFS.
Although the detection of anti-GQ1b antibodies strongly supports the diagnosis, their absence does not rule out MFS, as a minority of patients may not test positive for these antibodies. Therefore, a clinical diagnosis can still be made in the absence of anti-GQ1b if the clinical presentation aligns with MFS [6].
Nerve Conduction Studies
Nerve conduction studies (NCS) may show diminished or absent sensory nerve action potentials (SNAPs), especially in cases of axonal involvement. However, sensory conduction velocities are typically preserved, as MFS is not primarily a demyelinating disorder.
H-reflex testing, which evaluates the integrity of the reflex arc, is often absent in MFS, reflecting the areflexia that is characteristic of the syndrome.
Motor conduction studies are usually normal, further distinguishing MFS from some variants of GBS that may demonstrate motor conduction abnormalities [1].
Imaging
While imaging is not required for the diagnosis of MFS, it can provide supportive evidence in cases where there is diagnostic uncertainty.
Magnetic Resonance Imaging (MRI) of the spine may reveal thickening and enhancement of the intrathecal nerve roots and cauda equina, indicating inflammation. Enhancement of specific spinal nerve roots, particularly those innervating cranial and bulbar structures, may also be observed [6].
CT scans are less sensitive for nerve root involvement but may still be useful to rule out other causes of neuropathy, such as compressive lesions.
Figure 1 shows the enhancement of the anterior nerve roots of the cauda equina, a typical finding in cases of Miller-Fisher Syndrome (MFS) [7].
![Figure 1: Obvious enhancement of anterior nerve roots of cauda equina, a typical finding in cases diagnosed with Miller Fisher Syndrome [7].](https://neuropedia.net/wp-content/uploads/2024/09/unnamed-file-300x300.jpeg)
Figure 1: Obvious enhancement of anterior nerve roots of cauda equina [7].
Differential Diagnosis
To differentiate between Miller-Fisher syndrome (MFS) and Guillain Barré syndrome (GBS), several clinical features, diagnostic tests, and pathophysiological factors should be considered:
Clinical Features
Miller-Fisher Syndrome (MFS) is characterized by the classic triad of ophthalmoplegia, ataxia, and areflexia, typically occurring without significant limb weakness [6].
In contrast, Guillain Barré Syndrome (GBS) presents with ascending paralysis, which usually begins in the lower extremities and progresses upward, often with loss of reflexes and sensory disturbances. The weakness in GBS can become severe and may involve respiratory muscles, necessitating respiratory support in severe cases [8].
Cerebrospinal Fluid (CSF) Analysis
Both MFS and GBS typically show albuminocytologic dissociation in the CSF, characterized by elevated protein levels with a normal white blood cell count. However, in MFS, the elevation in protein may be more pronounced compared to GBS [8].
Electrodiagnostic Studies
In MFS, nerve conduction studies (NCS) often reveal reduced nerve action potentials and absent H reflexes.
In GBS, the findings vary depending on the subtype (e.g., acute inflammatory demyelinating polyneuropathy [AIDP] or acute motor axonal neuropathy [AMAN]), but may include evidence of demyelination (e.g., prolonged distal latencies, slowed conduction velocities) or axonal damage (e.g., reduced motor and sensory responses) [9].
These clinical and diagnostic distinctions aid in the differential diagnosis and appropriate management of MFS and GBS.
Treatment
(MFS) is mainly treated with supportive care, pain control, respiratory support as needed, and intravenous immunoglobulin (IVIg) or plasma exchange (PE) are the mainstays of therapy, last studies showed that IVIG and PE have similar curative effects.
Corticosteroids are ineffective in the majority of cases and are no longer recommended.
Risk factors and prognosis
Current evidence suggests that factors such as sex, age, history of prior infection, level of disability at the peak of illness, and the latency to peak symptoms do not significantly influence the overall outcome of Miller-Fisher Syndrome (MFS). Regardless of these variables, ataxia typically resolves within a median of 1 month, and ophthalmoplegia resolves within approximately 3 months after the onset of symptoms. By 6 months, the vast majority of patients experience either no disability or only minimal residual disability. This demonstrates that the natural course of MFS is generally associated with a favorable prognosis and high rates of recovery [14, 16].
While recurrent episodes of MFS are rare, a recent review by Ishii et al. reported that approximately 12% of patients experienced a recurrence of the condition, underscoring the need for ongoing clinical awareness, even in cases that initially resolve [17].
References...