Article topic: Status Epilepticus
Author: Farah Moh’d Sbeih Fuad Awayes
Editors: Ethar Hazaimeh, Yaman B. Ahmed
Keywords: Epilepsy, Status Epilepticus, Epilepsy Emergencies.
Introduction
Status Epilepticus (SE) is a neurological emergency; it varies in definition due to lack of a clear understanding of its pathophysiology but according to recent guidelines it is said to be “5 min or more of (i) continuous clinical and/or electrographic seizure activity or (ii) recurrent seizure activity without recovery (returning to baseline) between seizures” with a notable morbidity and mortality rates [1].
SE can be classified in various ways but as recommended by The Neurocritical Care Society, it is mainly classified as convulsive and non-convulsive [1]. Convulsive SE represents a generalized tonic-clonic activity that is easily identified, while the non-convulsive SE does not show an obvious activity and is further divided into simple and complex depending on its effect on the consciousness and mental status [2].
Refractory SE is defined as SE that is resistant to two antiepileptic drugs (AED) where one of them is benzodiazepine [3].
Super refractory SE is referred to as the SE that occurs after the initiation or cessation of anesthetic therapy and may last 24 hours or more [4].
Epidemiology
The incidence of SE lies between 18-41 patients per 100,000 per year [5]. Non-convulsive SE affects up to 10% of patients with the greatest risk in patients who have had previous epilepsy, elderly patients, and patients with sepsis [6]. The mortality of SE increases with increasing age and it ranges from 19% to 26% [5]. About 40% develop subsequent epilepsy attacks after their first episode of SE [7].
Pathophysiology
SE happens when the mechanism that stops the seizure fails because there is either inefficient inhibition due to decreased γ-aminobutyric acid (GABA), the main inhibitory neurotransmitter, or due to excessive stimulation from excitatory amino acids like glutamate and its analogues [8].
As SE persists, more calcium enters the neurons via NMDA receptor which leads to the activation of many enzymes like NADPH oxidase, nitric oxide synthase, and calpains; this can generate reactive oxygen species which can cause cell damage or accumulate in the mitochondria causing ATP depletion [9,10].
Etiology
There are wide possible etiologies that can cause SE and they can be divided into:
- Acute symptomatic: an acute neurological or a systemic cause like stroke, metabolic disturbances, CNS infection, and others [11,12].
- Remote symptomatic: like traumatic brain injury and brain tumors [11,12].
- Epileptic patients taking inadequate antiseizure drug doses [11,12].
- Unknown/Cryptogenic when there is no clear etiology found [11,12].
Diagnosis
All patients require a thorough history and physical examination with consideration to the patient’s clinical and mental state, neuroimaging with a non-contrast head Computed Tomography (CT) scan, and basic laboratory studies like complete blood count (CBC), blood glucose level, serum electrolytes (sodium, potassium, calcium, and magnesium), AED blood levels if known to have previous seizures.
Depending on the clinical presentation, patients may need brain Magnetic Resonance Imaging (MRI), a lumbar puncture, a toxicology panel, and other laboratory studies.
Electroencephalography (EEG) is a vital test where electrodes attached to a patient’s head detect electrical impulses generated. In a non-convulsive SE, the waves’ amplitude is higher compared to a normal EEG with regular patterns (Figure 1). After administering an anesthetic drug, a suppressed pattern will be noticed (Figure 2), this is useful when prescribing the desired drug dose to the patient [13].
![Figure (1): An EEG of a patient with non-convulsive SE [13].Status Epilepticus , Neuropedia](https://neuropedia.net/wp-content/uploads/2021/07/Picture1-1-300x194.png)
Figure (1): An EEG of a patient with non-convulsive SE [13].
![Figure (2): An EEG with a suppressed pattern of a patient after administering an anesthetic drug [13].Status Epilepticus , Neuropedia](https://neuropedia.net/wp-content/uploads/2021/07/Picture3-1-300x196.png)
Figure (2): An EEG with a suppressed pattern of a patient after administering an anesthetic drug [13].
Once an etiology has been figured, it must be controlled rapidly with a clear management plan. According to the American Epilepsy Society, guidelines are summarized in Figure (3) [14].
Prognosis
Prognosis is influenced greatly by the underlying cause; other factors include the patient’s history of chronic illnesses, the duration in which the episode lasts, and the patient’s age [8].

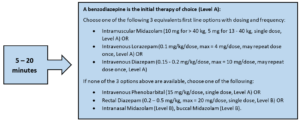

Figure (3) American Epilepsy Society Treatment Guidelines [14].
References...