Article topic: Carotid Occlusive Artery Disease – Carotid Artery Stenosis
Author: Yusra Ghassan (Moh’d Akram) Arafeh
Scientific editor: Dr.Omar Jbara
Linguistic editor: Philip Sweidan
Anatomy
The vascularization of the brain and the spinal cord depends entirely on two sources: the right and left vertebral arteries, which arise from the right and left subclavian arteries and the right and left internal carotid arteries, which arise at the base of the neck where the common carotid arteries bifurcate into external and internal carotid arteries.
After arising from the subclavian arteries, the vertebral arteries then proceed superiorly and travel across the posterior arch of C1, subsequently entering the foramen magnum. When meeting at the base of the pons they join to form the basilar artery in the midline. The basilar artery being the main blood supply to the brainstem. The basilar artery eventually forms the Posterior Cerebral Circulation.
Regarding the latter, the internal carotid arteries form two major arteries, the anterior and middle cerebral arteries, which form the Anterior Cerebral Circulation. The Anterior and Posterior Cerebral Circulations form the arterial ring called the Circle of Willis.
The internal carotid arteries and their branches supply blood to the frontal lobe and the lateral surface of the temporal and parietal lobes. Those areas are majorly responsible for the control of logical thinking, personality. It is also where the primary motor and sensory areas reside. [1]

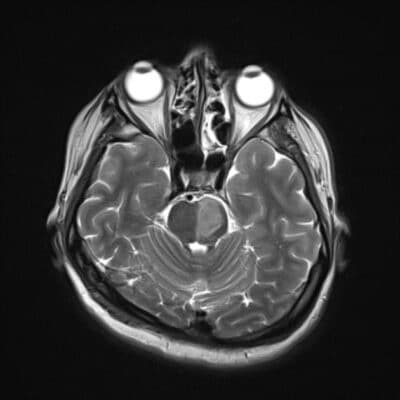
Figure 1: Brain blood supply and vertebral artery segments ,
Pathophysiology
Carotid occlusive artery disease, also called Carotid artery stenosis, is the progressive narrowing of the carotid arteries which could result in severe consequences. The mentioned stenosis or narrowing is mostly secondary to the development of atherosclerosis. Atherosclerosis is described to be a disease of the arterial intima; it is a pathological progressive process characterized by the build up of atheromatous plaques inside the vessels [3]. This plaque is made up of cholesterol, fat, calcium and other substances circulating in the bloodstream. Overtime, the presence of the plaque gradually reduces the lumen of the vessel. This decreases the blood flow through the affected vessels, which according to the size and area of the lesion results in a wide spectrum of symptoms [4]. In the cervical carotid artery, the bifurcation of the common carotid artery creates shear stress secondary to the turbulence and high-pressure of the arterial blood flow. This subsequently causes endothelial damage and recurrent inflammatory cascades. The recurrent bouts of inflammation lead to progressive deposition of plaque. This is followed by secondary migration of mononuclear cells and lymphocytes and consequent stimulation of smooth muscle cells in the arterial media to migrate and proliferate. Moreover, lipids, most notably by low-density lipoproteins, are taken up and deposited by the macrophages. Lipid-laden macrophages, or foam cells, continue to accumulate alongside calcium and other substances. Gradually, this compromises the integrity of the carotid arterial lumen and decreases the cerebral blood supply. Furthermore, if a portion of the carotid plaque happens to rupture and migrate distally into the intracranial circulation, partial or complete obstruction of the blood flow can occur secondary to the breaking off and the lodging of the thromboembolism.
Strokes—a term that refers to the death or dysfunction of brain tissue due to vascular disease. Ischemic stroke remains a leading cause of death and disability in the developed world. Carotid artery stenosis is relatively common and the atherosclerotic plaques formed are a source of emboli that can cause disturbance to the cerebral blood flow.
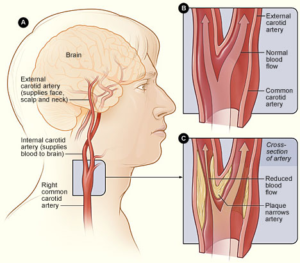
Figure 2: A shows the location of the right carotid artery in the head and neck. Figure B shows the inside of a normal carotid artery that has normal blood flow. Figure C shows the inside of a carotid artery that has plaque build up and reduced blood flow. [5]
Presentation and complications
The clinical presentation of a stroke or TIAs is composed of a wide spectrum of possible signs and symptoms. Due to the significance and the consequences of such a thromboembolic event, recognizing the signs and symptoms of a symptomatic carotid stenotic disease is critical.
The most common neurological examination findings include: dysarthria, facial weakness, contralateral hemiparesis or hemiplegia, or a pronator drift.
One particular neurological symptom experienced by the patients is Amaurosis fugax, an acute, atraumatic monocular visual loss described as a curtain being lowered over the patient’s symptomatic eye caused by marginal perfusion related to diminished retinal blood flow or retinal micro-emboli.
Approximately 10% to 15% of those who experience a stroke have a history of a sentinel TIA. The consequence of the thromboembolic event is highly dependent on the size and the vessel blocked.
The most commonly affected vessel by thromboembolic events is the middle cerebral artery. Manifestation of an infarction in the territory supplied by the MCA is variable due to its large area. These manifestations mostly include: contralateral weakness and hemisensory loss. If the lesion was on the dominant side, this would lead to aphasia. While a lesion was on the nondominant side, would more likely present as hemineglect and apraxic syndromes.
Infarctions in the anterior cerebral arteries lead to contralateral weakness that is more profound on the lower extremities compared to the upper extremities .
Infarctions in the ACA that supplies the frontal lobe will cause cognitive or psychiatric disturbances.
The anterior choroidal artery supplies the posterior limb of the internal capsule, the posterolateral thalamus, and the lateral geniculate body, infarctions of which present clinically as the triad of contralateral hemiparesis, hemisensory loss, and hemianopsia(visual field cut).
The classic deficit in posterior cerebral artery infarctions is a contralateral visual field cut. Yet, It is noted that sensory or visual disturbances or deficits are rare[6][7].
Work up and Diagnostic Imaging
There are several neuroimaging modalities that can be utilized to diagnose, localize, and measure the degree of the carotid artery stenosis. However, the most frequently used screening tool for the detection of the carotid artery stenosis is the doppler ultrasonography, which uses real-time imaging to detect changes in the velocity of the flow of the blood through the vessel in question. Moreover, the patient is usually asymptomatic, and the setting is usually non-emergent. It is requested by the physician after the detection of a carotid bruit in a physical examination. Remarkable elevation in the velocity of the flow is associated with significant reduction of the arterial lumen, and thus, is usually the finding of a symptomatic carotid artery stenosis case.
There are other common modalities like Computed Tomography Angiography (CTA) and Magnetic Resonance Angiography (MRA) that are used in an emergency setting or to confirm the findings of the doppler ultrasound. CTA is particularly useful in a patient with a pacemaker or a stent. However, the gold standard imaging modality for exact calculations of the degree of the stenosis is Digital Subtraction Angiography (DSA) that is a fluoroscopy technique used in interventional radiology. It can be used on the carotid arteries bilaterally and on the vertebral arteries as well. [8]
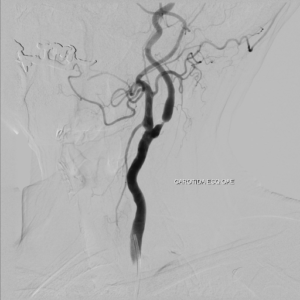
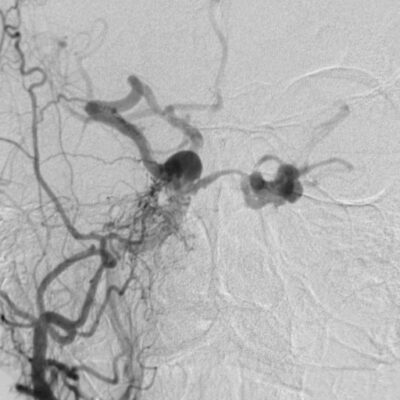
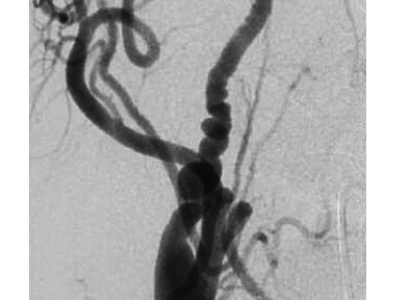
Figure 3: Angiography study confirms stenosis greater than 70% in the left ICA.[9]
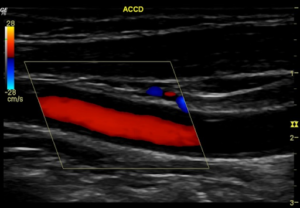
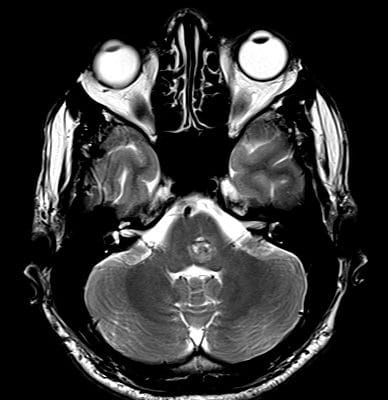
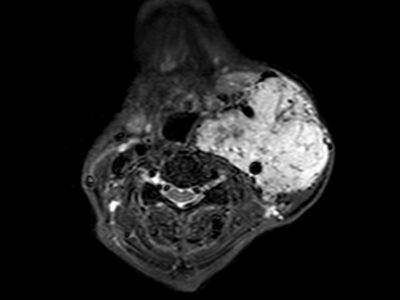
Figure 4 :Carotid Doppler study demonstrates bilateral atherosclerotic mixed plaques on bulbs (calcified and hypoechoic), being more important on the left, where it is practically sub-occlusive (near occlusion of the ICA)[9]
![Left ICA PSV is greater than 230 cm/sec (267.5 cm/sec). Left CCA PSV is 81.9 cm/sec. ICA/CCA index > 2.[9]](https://neuropedia.net/wp-content/uploads/2021/02/unnamed-1-300x220.png)
Left ICA PSV is greater than 230 cm/sec (267.5 cm/sec). Left CCA PSV is 81.9 cm/sec. ICA/CCA index > 2.[9]
To minimize the incidence of ischemic strokes in patients diagnosed with carotid artery stenosis, there are standard treatment algorithms that are dependent on each individual’s particular modifiable and nonmodifiable risk factors. Treatment of carotid artery stenosis includes medical and surgical approaches.
Regarding medical management as an approach, the pharmacologic mainstay is platelet antiaggregating.
Aspirin’s mechanism of action is characterized by irreversible inhibition of platelet cyclooxygenase, which subsequently thwarts the production of thromboxane A2. Moreover, thromboxane A2 works as a vasoconstrictor and a platelet aggregation inducer. Thus, by inhibiting the production of thromboxane A2 we prevent further exacerbation of the stenotic lesion, or complete sudden blockage of the arterial lumen.
Studies have shown that one hour post-ingestion of a single aspirin results in 98% inhibition of the formation of thromboxane A2 and, thus, prevents its aftermath from taking place. Adding to that, randomized trials of platelet antiaggregating therapy in patients with history of transient ischemic attack or stroke showed 25% reduction in the risk of nonfatal stroke and death from a vascular cause [10]. This reduction of risk was independent of patient’s age, sex, and any other risk factors.[11]
After undergoing the carotid endarterectomy, which is the traditional surgical approach to this disease, aspirin has been associated with reduction in mortality rates and is considered to be a standard of care for patients suffering from this disease, regardless of whether the medical or the surgical approach was the mainstay of their treatment. However, the medical evidence is still in controversy regarding the dosage of aspirin that is associated with the best outcome for patients. Nonetheless, studies that were trying to evaluate its efficacy have utilized doses ranging from 30 to 1500 mg/day.[12]
In the Aspirin in Carotid Endarterectomy trial, a total of 2804 patients who had undergone the surgery were randomized to compare the benefits of low-dose aspirin (81 to 325 mg/day) and high-dose aspirin (650 to 1300 mg/day). The goal of the trial was to assess the risk reduction in stroke, myocardial infarction, and death secondary to vascular causes. Three months postoperatively, the risk reduction was 6.2% to 8.4% favouring the high-dose aspirin group. [13]
Also, another antiplatelet aggregate is Ticlopidine. Regarding the mechanism of action, it consists of inhibiting the adenosine phosphate pathway. It was not tested or studied specifically for patients with carotid stenotic disease. However, its usage has led to reduction in the risk of stroke, myocardial infarction, or death secondary to a vascular cause after a cardio-embolic stroke. It was reported that the relative risk of subsequent strokes, whether fatal or nonfatal, have been reduced by 12%; in comparison with aspirin[14-15].Nonetheless, the dose recommended for ticlopidine to be beneficial in this condition is 250 mg twice daily.
However, the side effects profile thwarts its widespread implementation. The worrisome side effects include significant hematologic side effects including reversible neutropenia and thrombotic thrombocytopenic purpura.
Clopidogrel, an adenosine diphosphate receptor antagonist, is also used for medical management. In a study that included 19,000 patients suffering from a vascular disease secondary to atherosclerosis, a Clopidogrel of 75 mg/day was found to be more effective than 325 mg of aspirin in the risk reduction for a subsequent stroke, myocardial infarction, or death secondary to a vascular cause [16]. In patients who suffered from strokes, there was a relative risk reduction of 7.3% in favour of Clopidogrel.
Considering the favourability of Clopidogrel, the side effects profile is relatively benign, when compared to ticlopidine and aspirin, which is responsible for increased incidences of gastrointestinal bleed and gastric or duodenal ulcers. However, the tests did not test the effects of Clopidogrel use on patients with isolated carotid artery stenosis.
Dipyridamole is a phosphodiesterase inhibitor. It works by increasing the levels of intracellular cyclic adenosine monophosphate. Its side effects profile consists of gastrointestinal distress and headaches, neither of which cause significant impairment.
A study called the European Stroke Prevention Study-2 (ESPS-2) randomized patients with documented previous TIA or stroke to a treatment with low-dose aspirin, modified release dipyridamole, a combination of both agents, or a placebo. The study reported that the combination of the two agents reduced the stroke rate. Suggesting that the dipyridamole has a synergic effect when used with aspirin [17].
Clinicians use combinations of platelet antiaggregant therapy but there’s still controversy regarding their superiority to one agent therapy in the prevention of stroke. There have been studies evaluating the usage of platelet glycoprotein IIb-IIIa receptor inhibitors for cardiovascular disease. However, more trials are required to evaluate their validity in carotid artery stenosis. Warfarin has also been utilized in stroke prevention in patients with non-valvular atrial fibrillation. Warfarin is undoubtedly effective in decreasing the incidence of stroke in patients who suffer from cardiogenic emboli, but their effectiveness with atherothrombotic TIA or stroke is yet to be evaluated. However, some clinicians use it for severe internal carotid stenosis.
The surgical standard of care at most institutions for the definitive treatment is CEA. Endovascular treatments such as catheter-based procedures, such as carotid artery stenting have also been performed for carotid artery stenosis.
The results of the Stenting and Angioplasty with Protection in Patients at High Risk of Endarterectomy and Carotid Revascularization Endarterectomy versus Stenting Trial (CREST) suggested that carotid artery stenting with the use of a distal protection device is a superior therapeutic intervention for high-risk patients who met the surgical criteria outlined previously by the NASCET.[19-23].
In 2010, the European International Carotid Stenting Study reported an increase in the incidence of strokes after undergoing the carotid endarterectomy procedure, despite the usage of distal protection devices. However, stenosis can recur after the stenting procedure.
Regardless of the number of trials conducted evaluating the medical and surgical managements, and differentiating between stenting and CEA. No neurosurgical procedure has demonstrated better outcomes in the treatment of carotid artery stenosis than CEA. It is also widely believed in the surgical community that CEA is superior to medical management alone for symptomatic patients with greater than 50% carotid stenosis and for asymptomatic patients with greater than 60% carotid stenosis.[24,25]
Risk factors and Prevention
There are several modifiable risk factors for stroke. Most prevalently is hypertension. Studies and evidence-based medicine has confirmed that control of blood pressure substantially reduces the patient risk of stroke. [26]Even a reduction in diastolic blood pressure of 5 to 6 mm Hg has the capacity to decrease the risk of stroke by almost 42%. Also, control of isolated systolic hypertension decreases the risk of stroke by 36%. [27-28]
Cardiologists advise that systolic blood pressure greater than 140 mm Hg, and diastolic blood pressure greater than 90 mm Hg requires treatment, whether in the form of lifestyle modification or medical therapy.
Diabetes mellitus increases the risk of stroke. This increase is secondary to hyperinsulinemia which propagates the formation of plaques and accelerates the atherosclerosis of large arteries. It has been reported that serum glucose levels less than 126 mg/dL are optimal. [26], [29], [30]
Nonetheless, other modifiable risk factors for an ischemic stroke are heavy alcohol consumption and cigarette smoking. [31] Interestingly, studies have shown that light to moderate alcohol drinking demonstrates a protective effect. It was also documented that individuals who drink lightly had a lower incidence of experiencing an ischemic stroke in comparison to those who indulge in heavy alcohol consumption, or those who are abstinent. Preferably, patients should be encouraged to quit smoking.