Article Title: Blunt Cerebrovascular Injury
Author: Nancy Abu Amoud
Editors: Dr.Omar Jbarah , Zain Alsaddi
Keywords: Cartotid Injury, Vertebral Injury , Stroke
Overview
Blunt cerebrovascular injury (BCVI) is a range of intracranial or extracranial traumatic injuries to the carotid and vertebral arteries in around 1-2% of patients presenting with blunt trauma to the head, neck, and chest. Although uncommon, it may lead to high mortality and morbidity as a devastating brain injury.(8, 9) It is important to note that ischemic stroke occurs in a large portion of patients with BCVI at a rate of 10% as reported in studies.(7)
Etiology and Pathogenesis
High energy, non-penetrating trauma causes cerebrovascular injury resulting in defects in one or more of the arterial walls.(7) This results in intimal tear that exposes the collagen of the endothelium, thus initiating platelet aggregation to create a healing thrombus, which could possibly induce stenosis or vessel occlusion. Having that said, an intimal tear could produce a space for dissecting blood to narrow or occlude the vessel or even for a traumatic aneurysm.(5)
Multiple injury mechanisms have been suggested, longitudinal stretching of the artery with subsequent partial or complete failure of arterial mural integrity is the main suspected mechanism.(12) Direct injury to the carotid or vertebral arteries can be caused via displacement of bone fragments from skull base or cervical spine fractures.(4, 12) Carotid injury could be caused by intra-oral trauma, or direct blow to the neck (e.g.; impact against a steering wheel, seatbelt or near hanging).(12) Blunt vertebral injuries have been associated with facet-joint dislocations, subluxations, as well as fractures extending into the foramen transversarium.(4)
In most cases, the potential mechanisms of stroke in BCVI are thromboembolism and hemodynamic insufficiency. Although, research shows that thromboembolism is the more likely mechanism of injury supported by analysis of vascular lesions and the presence of micro emboli in patients with BCVI.(6)
Clinical presentation
Most BCVI are asymptomatic lesion discovered on screening CT angiography based on screening criteria.(13) For symptomatic BCVIs, presentation is often like that of spontaneous dissections, with the classic triad of neck/head pain, Horner syndrome, and brain ischemia. Other presentations could involve headache or neck pain, cranial nerve palsies, distal ischemia, spinal cord ischemia, traumatic fistulae, or hemorrhage/ hematoma.(5)
Risk factors and screening
Multiple screening tools have been developed to identify patients at risk of BCVI, modified Memphis criteria and Denver criteria. The recommended criteria are the expanded Denver screening criteria, which encompass indicators from the Memphis screening tool.(3)
- The expanded Denver screening criteria for BCVI: (3)
CT angiography is indicated if one or more of the criteria are present.
Signs/symptoms of BCVI
- Arterial hemorrhage from neck/nose/mouth
- Cervical bruit in patients < 50 years
- Expanding cervical hematoma
- Focal neurological deficit
- Neurological exam incongruous with head CT findings Stroke on secondary CT scan
Risk factors for BCVI
(High-energy transfer mechanism plus):
- Le Fort II or III Mandible fracture
- Complex skull fracture/basilar skull fracture/occipital condyle fracture
- Severe traumatic brain injury (TBI) with GCS < 6
- Cervical spine fracture, subluxation or ligamentous injury at any level
- Near hanging with anoxic brain injury
- Seat belt abrasion with significant swelling, pain or altered mental status
- TBI with thoracic injury
- Scalp degloving
- Thoracic vascular injury
- Blunt cardiac rupture
- Upper rib fracture
Imaging (1, 10)
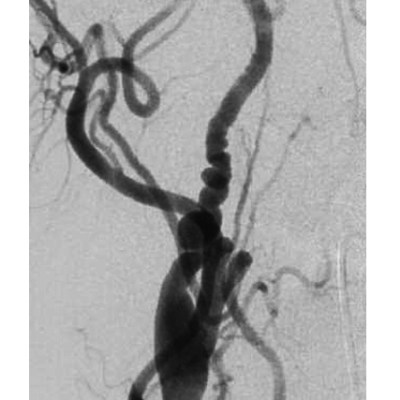
Digital subtraction angiography (DSA) is the imaging gold standard for detection of BCVI due to its high sensitivity and ability to detect collateral circulation. However, it falls behind due to its failure to provide information about vessel wall, and the associated complication rate of 1.3%, since it is an invasive technique. Arterial dissection, thromboembolism, and IV contrast-induced renal injury are possible complications for DSA. Therefore, its use is limited for patients with equivocal or negative CTA findings with strong clinical suspicion or when therapeutic intervention is needed.
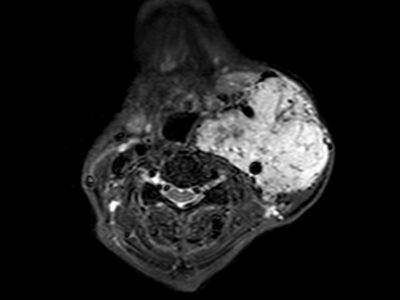
Computed tomography angiography (CTA) is considered the screening choice for BCVI, with sensitivity and specificity reaching 100% with the use of 16-sections or higher CT scans. Moreover, it is cheaper, widely available, non-invasive and saves time in reaching diagnosis and observation of non-vascular injuries.
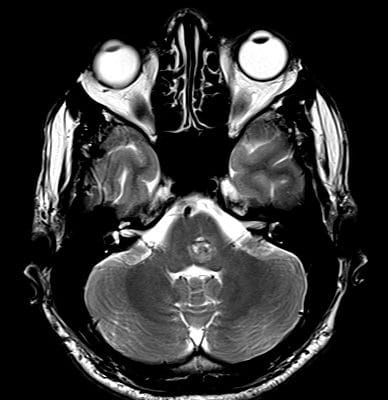
Magnetic resonance angiography (MRA) is not recommended as a single tool for diagnosis with a reported sensitivity of 50%. However, it is useful for detection of dissections and intramural hematoma and therefore could be used as a complimentary tool to CTA.
Duplex sonography has little role and is an inappropriate tool for screening of BCVIs, with a sensitivity rate of 38.5%.
In conclusion, digital subtraction angiography (DSA) remains the gold standard in detecting BCVI but it is time-consuming and not offered by all institutions. Thus, the recommended imaging study is CT angiography of the precerebral carotid and vertebral arteries reaching through the base of the skull together with the circle of Willis. (3)
Grading
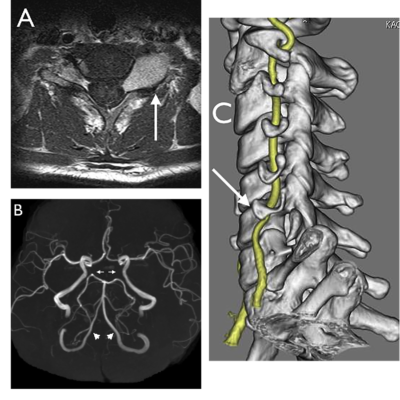
The Biffl/Denver scale is a commonly used grading system which describes injury according to angiography on a scale from I to V.(11) The risk of stroke increases with the increasing grade. (2)
- grade I: vessel wall irregularity or dissection with <25% stenosis
- grade II: dissection or intramural hematoma with ≥25% stenosis, intraluminal thrombus, or raised intimal flap
- grade III: pseudo aneurysm
- grade IV: complete vessel occlusion
- grade V: transection with free extravasation and/or high flow arteriovenous fistula
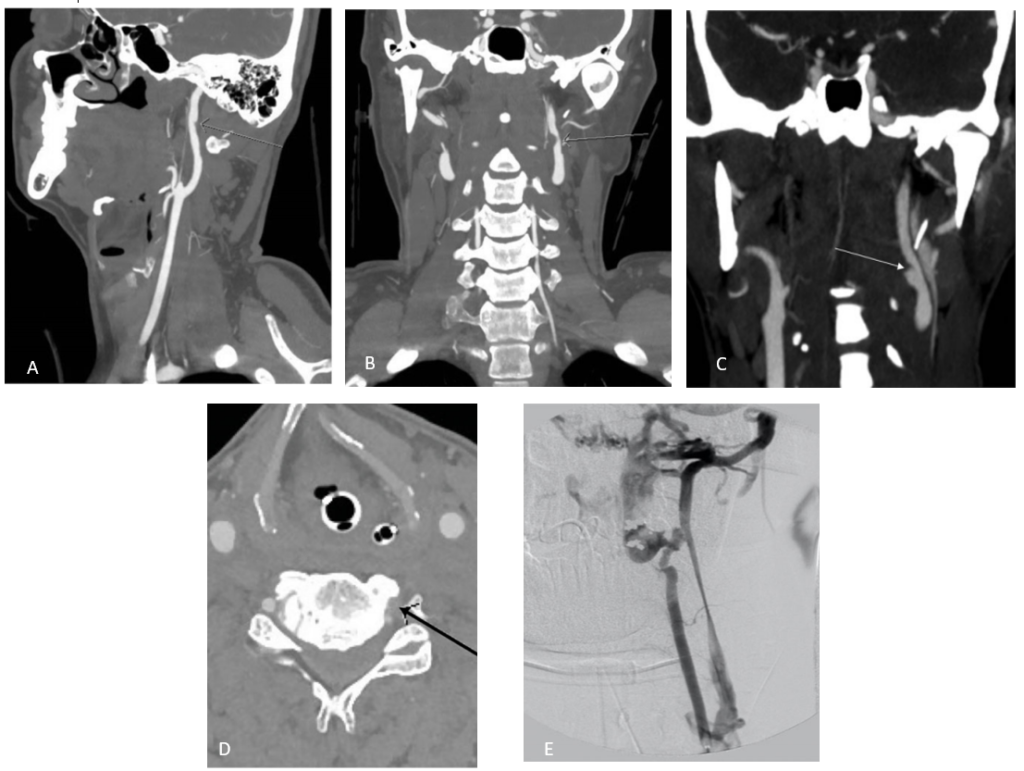
Figure 1: (Abu Mughli, 2020)(1)Biffl grade I injury. Sagittal CTA showing small intimal flap of the right cervical ICA, with <25% stenosis (A).Biffl grade II injury, coronal CTA showing moderate left sided extracranial ICA dissection with intramural hematoma causing >25% stenosis (B). Biffl grade III injury. Follow up imaging showing pseudo aneurysm on coronal imaging of a 31-year-old male with a history of polytrauma 6 days prior with initial scanning revealing Biffl grade II (C). Biffle grade IV injury. Left vertebral artery occlusion on axial image (D).Biffle grade V injury. DSA showing left vertebral artery irregularity at C3 level, at C2/3 level there is complete artery occlusion with an AV fistula draining into enlarged epidural veins (E).
Management
- The management of BCVIs remains somewhat controversial. (5) Due to the nature of ischemic stroke being identified primarily as thromboembolic in origin, antithrombotic therapy is the primary method of treatment. Studies report the use of anticoagulation (42.8%), antiplatelet (32.5%) or both (17.1%).(7) It is of importance to note that many patients with BCVI have polytrauma and require surgery. Therefore, the increased risk of bleeding must be weighed with the risk of ischemic stroke in these patients. (7) The use of antiplatelet therapy as an alternative to anticoagulation has shown a favorable risk for complications with equivalent if not superior neurologic outcomes. (5) Endovascular and surgical treatments are reserved for patients with severe injury (grade V), or patients with pseudo aneurysm (grade III), which if not treated, commonly does not resolve. Options include; stenting, resection and embolization. (1)
Prognosis
Overall mortality rates depend on the injured artery; reports show 7–21% mortality for carotid artery injury and 4-8% for vertebral artery injury. Similarly, stroke rates related to BCVI also depend on the injured artery; infarctions are more likely to occur with carotid artery injuries than injuries in vertebral arteries reported at 26-41% and 14-24% respectively. (11)
Additionally, stroke rate increases with increasing injury grade regarding carotid artery injury, while stroke rate in vertebral artery injury is not remarkably influenced by injury grade. (11)
External links
*Endovascular reconstruction of enlarging traumatic internal carotid artery pseudoaneurysm – Vedio
*Open Repair of Carotid Artery Pseudoaneurysm (Rahimi, MD, Rojo, MD, & Mohamed, MD) -Vedio