Title: Brain abscess
Authors: Qusay Fadel, Rand Al-Qaseer
Editor: Sia Sawan , Dr Omar Jbarah
Keywords: Cerebral abscess, Neuro infection, Hypodense lesion.
Overview
Brain abscess (BA or Cerebral abscess) is a circumscribed collection of purulent exudate in the brain that develops in response to an infection or trauma. The majority of cases are caused by the spread of infected material from a focus of suppuration elsewhere in the body, notably the paranasal sinuses, middle ear, heart, and lungs. Penetrating craniocerebral trauma and neurosurgical procedures may also be associated with this condition. Clinical manifestations include headache; seizures; focal neurologic deficits; and alterations of consciousness. (Adams et al., Principles of Neurology, 6th ed, pp712-6)
Brain abscesses are potentially serious, life-threatening diseases that pose a complex diagnostic challenge not only to neurosurgeons but also to clinical microbiologists, neurologists, psychiatrists, infectologists (1).
Epidemiology
According to studies, brain abscess accounts for a disproportionate percentage of space-occupying intracranial lesions in developing countries compared to developed nations with an approximate incidence of 8% of intracranial masses compared to 1% to 2% in the Western countries with approximately four cases occurring per million. (2)
The prevalence of brain abscess in patients with acquired immunodeficiency syndrome (AIDS) is much higher. (2) The incidence of fungal brain abscesses also has increased because of the higher usage of broad-spectrum antibiotics and immunosuppressive agents like steroids. (2)
Prevalence is highest in adult men younger than 30 years while pediatric disease occurs most frequently in children ages 4 to 7 years. Neonates are third in high-risk groups. Vaccination has reduced the prevalence in young children. Data suggests that brain abscesses are more predominant in males than in females with a male-to-female ratio varying between 2:1 and 3:1.(2)Geographical and seasonal differences have no significant impact. (2)
Etiology
The brain abscess is a pus-filled swelling surrounded by a well-vascularized capsule found in different places in the brain but most commonly exists in the frontal lobe. (3) The etiology of brain abscess is usually polymicrobial, most commonly involving a variety of aerobic and obligate anaerobic bacteria. (4) For example, staphylococcus and streptococcus are found to be the causative agents for cerebral abscess in patients who had surgery in their brain before, while Clostridium and Enterobacteriaceae are common in patients with penetrating head injury. (5)
The immunocompromised patients that are taking chemotherapy or steroids therapy, or with HIV infections or undergo an organ transplant procedure are likely to develop brain abscess due to fungal infection (mainly Aspergillus and candida)(5), toxoplasma, and pseudomonas. (6)
AIDS patients are more susceptible to being infected by Cryptococcus, Listeria, and Nocardia. Additionally, many cases reported that AIDS patients have developed tuberculous abscesses due to mycobacterium tuberculosis which is considered to be a rare condition. (7)
The development of brain abscess occurs in 2 manners:
- Contagious manner mostly due to sinusitis, otitis media, or mastoiditis, which lead to inferior temporal and cerebellar brain abscess. While dental surgeries cause frontal lobe abscesses. (8)
- Hematogenous spread is found in 9% to 43 % of cerebral abscesses cases (46).
Organs that takes part in this process ;
- Primarily, hematogenous spread arises from the lungs due to various lung disorders such as bronchiectasis, cystic fibrosis, and empyema.
- Congenital heart defect (CHD) is a leading cause that disrupts the normal blood flow through the heart and lung, most commonly in children, that results in the right-to-left shunt that affects the ability to carry the oxygen to the different sites in the body, and that will increase the risk of developing a cerebral abscess. (9)
Pathogenesis
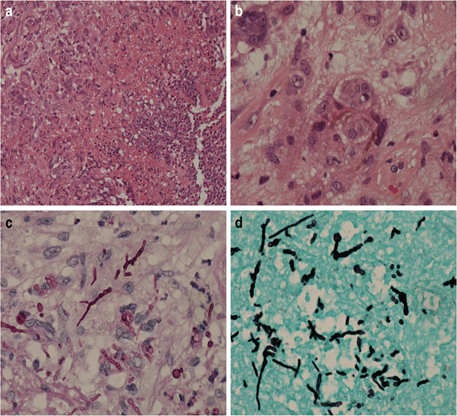
We can classify the development of brain abscess into four stages (6)
- the first stage; early cerebritis (1-4 days) the hallmark of this is stage is neutrophil accumulation, tissue necrosis, and edema. Also, the microglial and astrocyte will be activated.
- The second; is late cerebritis (4-10 days), predominant macrophage, and lymphocyte infiltrate.
- The third; Early capsule formation (11-14days) associated with the formation of a well-vascularized abscess wall.
- The fourth stage is (>14 days), approximately at 3-4 weeks, the capsule becomes thick and is amenable to excision.
Therefore, we can see in the first 1 to 2 weeks acute inflammatory characteristics like edema and vascular congestion. While, in 3 and 4weeksk we start to see necrosis and changes like the capsule, which consists of 3 layers: the inner one contains granulation tissue, the middle one is collagenous, and the outer one is an astroglial layer. (8) We can recognize these histological changes by a sing CT scan or MRI. (6) Activated microglial cells stimulate the antibacterial adaptive immune response by MHC class II and other stimulatory molecules expressions like cytokines IL-1 and TNF-alpha, these pro-inflammatory molecules initiate a response in the brain parenchyma. Thus, the usage of anti-inflammatory therapies can reduce the damage of the brain parenchyma and enhance the neurological condition of the patients. (6)
Clinical presentation and complications
The most frequent clinical manifestation of brain abscess is headache, fever while altered levels of consciousness are frequently absent (10). Neurological indications vary depending on where the abscess is located and can range from mild to severe. For days to weeks, the effect is mild. Changes in behavior may occur in patients who have abscesses in the frontal or temporal lobes. Patients with abscesses in the brain stem or cerebellum may present with cranial nerve palsy, gait disorder, or either headache or altered mental status owing to hydrocephalus (11). Clinical manifestations become more evident as the abscess grows larger and the surrounding edema increases, but these symptoms and signs may be difficult to recognize because of sedation or the nature of the underlying neurologic disease (12). Patients with hematogenous spread of bacteria may present with symptoms of the underlying infection (13).
Diagnosis
Lab tests in patients with brain abscess include the following: Complete blood count and platelet count, erythrocyte, serum C-reactive protein, serologic test (serum immunoglobulin G antibodies, RT-PCR for toxoplasma), blood cultures for microorganisms, etc., (at least 2; preferably before antibiotic therapy).
Lumbar puncture: Because of the threat of cerebrospinal fluid (CSF) leakage and death, it should only be performed after ruling out increased intracranial pressure that used a prior CT and MRI scan. Blood cultures can be done to start antibiotic therapy in acute cases presentation of patients or suspicion of meningitis. An elevated protein level, pleocytosis with a fluctuating neutrophil count, often a normal glucose level, and sterile cultures are the most common findings. When the white blood cell (WBC) count increases, together with elevated CSF lactic acid and numerous red blood cells (Erythrocytes) in the CSF, a lumbar puncture is performed, but this test is rarely used.
Stereotactic Computed Tomography (CT) or Surgical Aspiration: Culture, Gram stain, serology, histopathology, and PCR amplification can be done with the samples obtained.
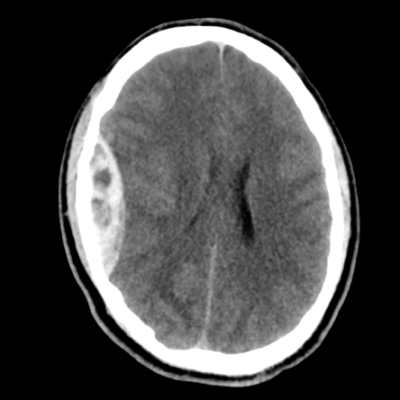
Imaging studies: In the case of a brain abscess, CT scanning has rendered other diagnostics including angiography, ventriculography, pneumoencephalography, and radionuclide brain scanning essentially obsolete. CT scans are less sensitive than MRI scans, but they are easier to administer. CT scanning, preferably with contrast administration, provides a rapid means of detecting the size, the number, and the location of abscesses, and it has become the mainstay of diagnosis and follow-up care. This method is used to confirm the diagnosis, localize the lesion, and monitor the progression after treatment. However, CT scan results can lag behind clinical findings. (14)(15)
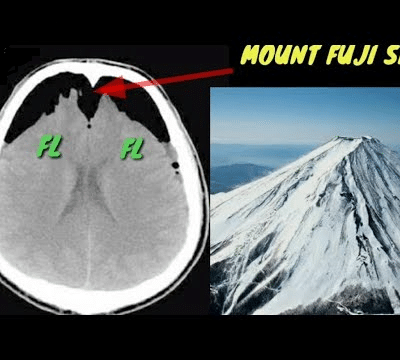
CT scans usually show the brain abscess as a hypodense center with an asymmetrical enhancement ring around it after a contrast substance is injected. A well-organized abscess barrier rarely fails to provide ring augmentation. CT scans indicate nodular enhancement with areas of low attenuation without enhancement in the early stages of cerebritis. Contrast enhancement is seen as the abscess grows. After encapsulation, the contrast material is unable to distinguish the clear core, and the CT image resembles those obtained during the early stages of cerebritis. Figure (1)

FIGURE(1). CT SCAN OF A BRAIN ABSCESS Case courtesy of Assoc Prof Frank Gaillard, Radiopaedia.org, rID: 5150
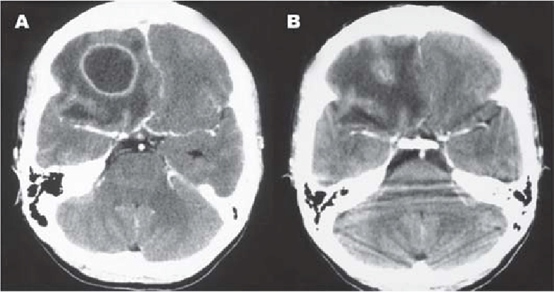
In the diagnosis of a brain abscess, many professionals consider MRI to be the
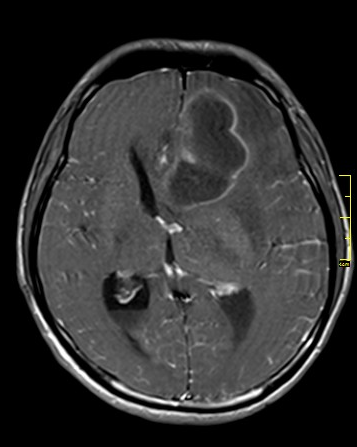
FIGURE (2). MRI FOR BRAIN ABSCESS. Case courtesy of Dr. Pat S. Kwankaew (MD), Radiopaedia.org, rID: 16451
first diagnostic approach. Because of its superior sensitivity and specificity, it enables accurate diagnosis and effective follow-up of lesions. MRI has a superior capacity to detect cerebritis, stronger contrast between cerebral edema and the brain, better visualization of the brainstem, and earlier detection of satellite lesions and inflammation extending into the ventricles and subarachnoid space as compared to CT scanning. Figure (2)
Susceptibility-weighted phase imaging showed evidence of paramagnetic substances in agreement with the presence of free radicals from phagocytosis in a study of 14 patients with brain abscesses. (16) This technique could add to the characterization of pyogenic brain abscesses by providing additional information.
Other tests: On occasion, an EKG will demonstrate a high voltage center with moderate activity. It’s ambiguous, and it’s only used to confirm a diagnosis of a brain abscess on rare occasions. This is the procedure in the diagnostic evaluation that is the least accurate.
Staging
The early stage of brain abscess (first 7-14 days) is called cerebritis and is associated with edema. Necrosis and liquefaction occur after 2-3 weeks, and the lesion becomes gradually surrounded by a fibrotic capsule. (17)
Treatment and Management
An abscess inside the brain can cause increased intracranial pressure, as well as significant morbidity and mortality. Medical and surgical approaches can also be used to manage this disease. Medical management can be considered for deep-seated, small abscesses (less than 2 cm), cases of coexisting meningitis, and a few other selected cases. Usually, a combination of both medical and surgical approaches is considered. (18)
Before abscess encapsulation and localization, antimicrobials, accompanied by measures to control increasing intracranial pressure, are essential. (19) For a single abscess, immediate intervention is required. Abscesses larger than 2.5 cm are excised or aspirated, but those smaller than 2.5 cm or at the stage of cerebritis are just aspirated for diagnostic purposes. Frequent extraction is preferred in cases of numerous abscesses or abscesses in essential tissues. In these patients, a high dose of antimicrobial(s) for an extended length of time may be an alternative.
The abscess is identified and parameters such as size and the number of abscesses are described using CT and MRI brain scanning. Large abscesses (greater than 2 cm) are usually considered for aspiration or excision, based on the surgeon’s skills. Multiple abscesses are managed with a long course of high-dose antibiotics, even without aspirations, based on weekly CT scanning. The selection of an antibiotic regimen should be wisely made based on microorganisms isolated from blood or CSF. Certain antibiotics are unable to cross the blood-brain barrier and are not useful in treating brain abscess; these antibiotics include first-generation cephalosporins, Aminoglycosides, and tetracyclines. (20)
Antibiotic prescriptions aimed at specific microorganisms:
- Gram-positive bacteria including streptococci: third-generation cephalosporin (e.g., cefotaxime, ceftriaxone) or penicillin G are effective. (21)
- Staph aureus, staph epidermis is usually seen in association with penetrating brain trauma and or neurosurgical procedure. It should be covered with vancomycin. It is also effective for Clostridium species. In cases of vancomycin resistance, linezolid, trimethoprim-sulfamethoxazole, or daptomycin can be considered. (20)
- Fungal infections including Candida, Cryptococcus needs to be treated with Amphotericin B. (20)
- Aspergillusand Pseudallescheria boydii. Voriconazole can be considered (20)
- Toxoplasma Gondi infection is treated with pyrimethamine and sulfadiazine, can be combined with HAART in cases of HIV. (20)
Corticosteroids, mannitol, and hyperventilation may be indicated where there is increased intracranial pressure. (21) Corticosteroids are a matter of contention. Steroids can cause encapsulation to be prolonged, necrosis to increase, antibiotic penetration into the abscess to be reduced, CT scans to be altered, and a rebound impact when they are withdrawn. If used to treat cerebral edema, the treatment should be brief. It is uncertain what dosage and when to administer it. Corticosteroids should not be used on a routine basis unless there is an increase in intracranial pressure.
In the treatment of brain abscesses, the surgical approach is extremely important. The procedure used is based on the skills and preferences of the controller. For multiple abscesses, methods include ultrasonography or CT-guided needle aspirations through the stereotactic method, bur hole, and craniotomy. Intravenous or intrathecal agents against specific microorganisms are considered with surgical therapy. (21)
Prevention
An abscess in the brain is a serious medical issue. It is important to take caution. You can reduce your risk by keeping an eye on any diseases that could lead to a brain abscess. At the first symptom of a brain abscess, contact your doctor. Based on many studies, If you have a cardiac disorder, ask your doctor before doing any dental or urological operations. Antibiotics may be given by your doctor before these procedures. This lowers your probability of gaining an infection that spreads to your brain.
Risk factor and comorbidity
- Immunocompromising conditions ( organ transplant, HIV, cancer): The relation between brain abscesses and HIV infection it’s not clear enough to confirm if HIV by itself is responsible for the cerebral abscess. Despite that, many types of research have explained that this disease can be raised due to chronic inflammation that takes apart when there is shedding of HIV proteins that lead to disrupting the integrity of the blood-brain barrier which will lead to an increase in the entrance of bacteria to the brain via hematogenous route. (22) As well AIDS patients are susceptible to infections like Cryptococcus, Listeria androgens Nocardia; which leads to multiple abscesses and tuberculous abscesses. (23)
- While the conjunction between brain abscess and brain tumor is rare, all the cases that conducted show it’s secondary to tumor removal surgery or due to chemotherapy and steroid therapy that suppresses the immunity and affect the blood-brain barrier which eventually will lead to making the area more susceptible to bacterial infections that cause the brain abscess. (24)
- Head trauma and Neurosurgery; any trauma to the brain or skull will increase the risk of nosocomial infections and the most common types of bacteria after a post-traumatic brain abscess are Gram-negative bacilli, especially staphylococcus aureus and Enterobacteriaceae. According to recent studies, the possibility of having brain abscesses after cranial trauma or neurological procedures is 2%-14%. (25)
- Dental infections; the oral cavity is considered as one of the major routes for many oral commensal bacteria especially streptococci (the most common)and Porphyromonas gingivalis, which is an oral anaerobic gram-negative bacterium and was found in 14.3% of cases. (26)
They are followed by dental procedures such as the extraction of infected teeth. These microorganisms can travel to the blood and cause bacteremia and rarely abscess outside the oral cavity like it can cause brain abscess and intracranial empyema (27). Also, dental Caries, missing teeth, and oral poor hygiene are the most commonly reported causes of brain abscesses due to oral infections.
- Liver and kidney disease, many studies found that patients with cirrhosis of the liver have a higher risk of different infections that leads to higher susceptibility of the occurrence of the cerebral abscess. In addition, hemodialysis patients are more prone to various infections that can proceed and cause cerebral abscesses. Also, a patient who had a kidney transplant and was receiving immunosuppressive drugs to prevent the rejection of the transplanted organ is susceptible to having brain abscess. (27) (28)
- Diabetes mellitus; fungal brain abscesses that are caused by dimorphic fungi, molds, and yeast are the most common types of microorganisms that may infect immunodeficient or uncontrolled diabetes patients. Although it is a rare condition there are reported causes for patients who had uncontrolled diabetes and had a past infection like dental infections, developed a thalamic abscess. (29)
- Microorganisms like bacteria, fungus, and viruses; staphylococcus aureus, and streptococcus (Streptococcus milleri and viridian group streptococci) are the main causative agents for brain abscess. Moreover, other gram-negative organisms such as Haemophilus spp, A ggregatibacter, Cardiobacterium hominis, Eikenella corrodens, and Kingella kingae. These types of bacteria can cause brain abscesses and endocarditis, but still, they are rare to cause the abscess. (30)
- Congenital heart disease; the brain abscess can emerge from dental infection, mastoiditis, osteomyelitis, sinusitis, and subdural empyema via hematogenous route especially in patients with cyanotic congenital heart disease (right-to-left shunt), Such as Patent foramen ovale (PFO) is not a common cause of brain abscess in adults as opposed to children. However, it’s still a cause for cerebral abscess in rare cases, especially when the cause of the disease is not clear enough so we should keep this defect in our mind when we are dealing with brain abscesses. (31)
- Lung abscess and bronchiectasis; it’s rare condition that is caused by a septic pulmonary embolism in which emboli-containing microorganisms migrate to the pulmonary artery which leads to the formation of pulmonary embolism and focal lung abscesses (32). This pulmonary abscess can cause the formation of a cerebral abscess. (33)
- Age; Male patients that are older than 40 years are likely to develop cerebral abscess more than female patients and patients under 40 years. (45)
The prognosis (outcome)
With the advent of antimicrobials and imaging studies such as CT scanning and MRI, the mortality rate has reduced from 5% to 10%. Rupture of a brain abscess, however, is more fatal. The long-term neurological sequelae after the infection are dependent on the early diagnosis and administration of antibiotics. (34) However, many studies showed that a brain abscess is nearly always fatal if left untreated. With treatment, the death rate declines to about 10% to 30%. The earlier you receive therapy, the better. The doctor will monitor a person during recovery, as an abscess can recur. This may involve undergoing a weekly CT scan for at least 2 weeks. Also, an abscess can return after months or years, so long-term monitoring is essential. (35)(36)(37)
Latest update on brain abscess therapy
Brain abscess is an urgent medical condition, that can progress anytime could cause pressure on the brain that leads to permanent damage and affect the blood and oxygen supply to the brain. (38) In addition, inter-ventricular rupture of brain abscess is a lethal condition and some researchers have reported that the fatality rates after the abscess ruptured are between 39% and 80% (8). The only treatment for the interventricular rupture is urgent craniotomy with quick removal of the abscess. (6)
While we are treating the patient’s abscess, we should take the clinical history of past infection and the immunity status of the patient into consideration. Also, the early detection and management of the cause of this abscess improve the neurological outcome. (8) The treatment process of the brain abscess is based on a combination of medicines and surgery, but the management processes can vary between individuals because it depends on the size and number. (5)
Antibioticgram-positive bacteria like Staph aureus, staph epidermis are found to be one of the major factors to develop abscesses, we use Cefotaxime/Ceftriaxone/Ceftazidime and metronidazole (6). Also, Vancomycin is effective for staphylococcus and Clostridium species. (9) For Nocardia, we use Sulpha drugs. (6) Fungal infections including Candida, Cryptococcus needs to be treated with Amphotericin B and 5 flucytosine. (39) (9) Toxoplasma gondii infection is treated with pyrimethamine and sulfadiazine (39) (9)
Steroids therapy
Steroids can be used in cerebral abscess management due to their function in reducing inflammation and enhancing the outcomes in some cases that are due to meningitis inducers such as S. pneumoniae, H. influenzae, N. meningitides, and M. tuberculosis. They are considered one of the essential therapy of autoimmune encephalitis. Also, steroids treatment is efficient in reducing the mass and the volume of cerebral edema. (7) (9)
Surgeries and brain abscesses
We use the operation approach when the abscesses are not responding to the medical treatment or still growing and do not shrink after 3 to 4 weeks of usage antibiotics, so here they will be treated by aspiration (41) (40) Also, the surgical application is used for abscesses that are larger than 2.5cm in combination with other treatments. (42) (39) It is known that surgeries must be done when the abscesses are located in essential and sensitive parts of the brain and causing precautions on the underlying place. (40) Now due to the development of neurosurgical techniques, the diagnosis and management of brain abscess enhance in the last decades. Such as stereotactic surgery, when cables are able most unable to a specific part of the brain, and it has a minimally invasive form of surgical intervention that uses a three-dimensional coordinate system. (43) This process is usually used for deep-seated abscesses such as thalamic abscesses. (39) The drainage of the pus enhances the patient’s condition and the outcomes can be seen immediately, multiple abscesses that are causing a direct mass effect should be treated by aspiration. Also, the abscesses that are located peripherally may fail to be treated by aspiration procedure so, we will use craniotomy and excision for these cases. (41)
According to one of the studies that have blended the department of neurosurgery, Istanbul faculty of medicine, one of the efficient ways to treat all types of abscesses regardless of their size and number is using the stereotactic aspiration with 8 weeks of using intravenous antibiotic therapy, which ends up with positive outcomes (43) (44)
The complete resection through craniotomy is rare now, it may be done when patients have a multi-lobulated abscess and advanced cranial hypertension (43) Also, traumatic brain abscesses remove the foreign body. (41) One of the instant cases that need to be treated rapidly with craniotomy is interventricular rupture of abscess and after the surgery is done we give the patient intravenous administration of antibiotics for 6 weeks. (39)