Article Topic: Adult Focal Epilepsy
Author: Leen Sawalha
Editors: Yaman B. Ahmed, Dr.Ethar Hazaimeh
Key Words: Adult Focal Epilepsy, Temporal Lobe Epilepsy, Mesial Temporal Lobe Epilepsy, Lateral/Neocortical Temporal Lobe Epilepsy, Frontal Lobe Epilepsy, Hippocampal Sclerosis
Overview and Epidemiology
Epilepsy is a condition characterized by recurrent seizures which are not provoked. It affects about 0.5% – 3% of the world, mostly occurring in extremes of age – young children and the elderly [1].
Adult Focal epilepsy is the most frequent type of epilepsy to be first seen and diagnosed in adulthood. It can appear at any stage of life with the presentation differing depending on the age of the individual. Adult focal epilepsy can be subdivided into the following:
- Temporal lobe epilepsy, which is further divided into mesial and lateral temporal lobe epilepsy
- Frontal lobe epilepsy
- Insular lobe epilepsy
- Cingulate lobe epilepsy
- Parietal lobe epilepsy
- Occipital lobe epilepsy [2].
Pathogenesis and Etiology
Temporal Lobe Epilepsy (TLE) is the most common presentation of focal epilepsy [3], TLE most frequently happens due to [4] :
- Infections
- Mutations
- Hippocampal sclerosis
- Tumors
- Brain injury
- Vascular deformities
- Cryptogenic causes
It is classified into:
- Mesial Temporal Lobe Epilepsy (MTLE):
It is the most commonly encountered subdivision of TLE, affecting the parahippocampal gyrus, amygdala, and hippocampus. It is usually associated with hippocampal sclerosis (HS). HS is a condition where gliosis of the hippocampus and neuronal cell death is apparent. Patients undergoing surgery who have HS are more likely to have a better prognosis than those without HS [5][4].
Other conditions that can also cause MTLE include dysembryoplastic neuroepithelioma, focal cortical dysplasia, cysts, heterotopias, cicatrices, heterotopias, cavernous malformations, and vascular deformities [6].
Additionally, MTLE has also been known to be genetically acquired (familial) [7]. Some studies suggest that in order for MTLE to happen, bilateral hippocampal involvement is required for the onset of seizures [8].
- Lateral/Neocortical Temporal Lobe Epilepsy (LTLE) is much less frequently seen. It can be familial (autosomal dominant LTLE) or sporadic (idiopathic partial epilepsy). Autosomal dominant LTLE is said to be caused by a genetic mutation in LGI1. This can cause dysfunction in AMPA receptors or potassium channels [2][6].
Frontal Lobe Epilepsy (FLE) can occur due to a multitude of reasons, these include:
- Tumors
- Cortical dysplasia
- Gliosis
- Encephalitis
- Hamartomas and other dysgenetic lesions
- Vascular malformations
- Trauma lesions [9][10]
In addition to that, it can also be caused by genetic mutations (such as CHRNA4 and CHRNB2) that code for nicotinic acetylcholine receptor subunits. This is referred to as autosomal dominant nocturnal frontal lobe epilepsy [9].
Parietal and Occipital Lobe Epilepsy is relatively uncommon [2].
One of the most common causes of insular epilepsy is the presence of a low-grade CNS tumor affecting the insula, most significantly gliomas [11].
Cingulate lobe epilepsy can be caused by the following:
- Gliosis
- Cortical dysplasia
- Cavernoma
- Meningioma
- Astrocytoma [12]
Clinical Presentation and Complications
Patients suffering from mesial temporal lobe epilepsy may experience the following symptoms:
- Auras
- Fear
- Olfactory hallucinations
- A feeling of butterflies in their stomach
- Sensations of gastric rising [2]
Symptoms associated with lateral/neocortical temporal lobe epilepsy are varied due to the lobe’s extensive connections to other areas of the brain. They are mostly dependent on the area of origin of the seizure [2]. Generally, symptoms include:
- Visual distortions [2]
- Vertiginous symptoms [2]
- Aphasia [13]
- Aura, which can be accompanied by auditory hallucinations [2][13].
- Single-sided clonic jerking of the upper extremities [14].
The clinical manifestations occurring in the frontal lobe in frontal lobe epilepsy are classified depending on location. The following table summarizes the symptoms associated with each area of the frontal lobe.
TABLE 1: Symptoms associated with Frontal Lobe Syndromes [15].
Insular and cingulate lobe epilepsy are relatively rare. Patients complaining of choking sensations due to contraction of the larynx/oropharynx or painful somatosensory aura should be suspected to be suffering from insular seizures [16][17].
As for cingulate lobe epilepsy, it is very hard to tell apart from other types of focal epilepsies. It is known to have very similar symptoms to temporal and frontal lobe seizures. This is due to the cingulate lobe’s extensive connections with those areas [18].
Parietal and occipital lobe epilepsy are uncommon. Symptoms are usually not useful for differentiating these types of epilepsies from frontal and temporal lobe epilepsy (since they also have extensive attachments with these areas) [2].
Occipital lobe epilepsy can manifest with the following symptoms:
- Visual auras [2]
- Ictal blindness [19]
- Movements of the eyes [19]
- Blinking [19]
Parietal lobe epilepsy is characterized by contralateral somatosensory auras (may also be bilateral) [20].
Workup and Diagnosis
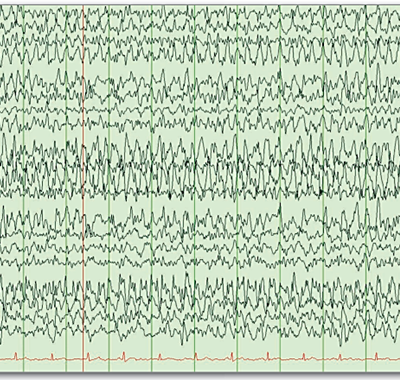
Mesial temporal lobe epilepsy is diagnosed by performing an EEG (usually with sleep recording). On the electroencephalogram, spikes can be seen in the temporal lobe’s front or tip (especially in mesial temporal lobe epilepsy). Spikes can be noticed while the person is either awake or asleep. A T1 and T2 MRI can also be used to check for discrepancies in the temporal lobe. It is also of great significance that the patient be questioned about the seizures and have them described to the physician.
Moving to neocortical lobe epilepsy, the patterns on EEG closely resemble those of mesial temporal lobe epilepsy but may present with temporal foci leaning more towards the mid or posterior region (electrodes T4/T3 and T6/5 are involved) [2].
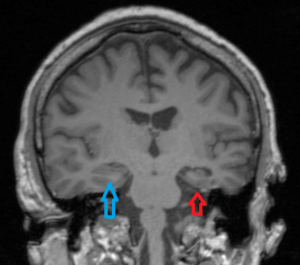
Figure 1: Temporal lobe atrophy, case courtesy of Dr Ian Bickle [22].
An invasive EEG is necessary for identifying insular and cingulate lobe epilepsy in cases where there is no obvious lesion seen on MRI [2].
EEG patterns seen in occipital and parietal lobe epilepsy can either be found focally or seen localized in the frontal and temporal lobe areas due to the abundance of connections found between them. Bilateral hypersynchrony may also be noticed [2].
Treatment and Management
Focal epilepsy can be treated using antiepileptic drugs. Examples of first-line agents used for the treatment of focal epilepsy include carbamazepine, phenytoin, oxcarbazepine, and valproic acid [24].
Additionally, ketogenic diets can be used for the management of epilepsy. A study that included 49 adults on a ketogenic diet concluded that 32 of those adults, who were diagnosed with idiopathic epilepsy, had shown significant improvement [25].
Moreover, vagus nerve stimulation can also be used for the treatment of focal epilepsy. Some studies indicated a decrease in seizures of more than 50% in those receiving this type of treatment [26].
In some cases, epilepsy can be unresponsive to antiepileptic drugs (drug-resistant epilepsy), most notably mesial temporal lobe epilepsy accompanied by mesial temporal sclerosis. The most prevalent surgical procedures done in hope of eliminating the aforementioned type of epilepsy include anterior temporal lobectomy in addition to amygdalohippocampectomy [27].
Risk Factors and Prevention
Alcohol consumption in alcoholics prone to seizures should be avoided. A study indicated that 86% of alcoholics who had previously experienced focal seizures had those seizures occur 48 hours after ceasing alcohol consumption. They concluded that alcohol withdrawal increases the probability of the occurrence of focal seizures [28]. Furthermore, caffeine has been shown to protect and increase susceptibility to seizures based on the dose, whether the administration was chronic or acute, and the stage of development at which caffeine was first given [29].
Nicotine has also been shown to be implicated in the development of convulsive seizures at large doses (30-4 mg/kg). However, this effect was short-lived and disappeared after 10 minutes [30]. Stressful life events can also lead to seizure onset. Some studies showed that people reported seizure onset following major life events [31]. Sleep fragmentation can also be a substrate for the occurrence of intra-sleep seizures [32].
Prognosis
Prognosis vastly depends on the underlying etiology and the presence of comorbidities. Surgery remains to be a great long-term treatment that substantially reduces the recurrence of seizures. However, it is of limited use.
The quality of life for those suffering from epilepsy is severely impacted. Additionally, epilepsy increases the probability of dying prematurely, primarily in those whose seizures prevail [33].
Recent Updates
Recently, genome sequencing techniques have become much more affordable. One method used in epilepsy investigation is known as array comparative genomic hybridization (array-CGH) [34]. This paved the way for precision medicine, which is mainly used for reversing the pathological consequences caused by certain gene mutations. However, disease-specific treatments for epilepsy are not yet widespread [35].