Article topic: Lateral Pontine Stroke
Authors: Chrystelle El Achkar, Luna Sakr
Editors: Odette El Ghawi, Joseph Akiki
Reviewer: Ethar Hazaimeh
Keywords: Marie-Foix Syndrome, neurology, stroke, cognition.
Abstract
Lateral Pontine Stroke, also known as Marie-Foix Syndrome or Marie-Foix Alajouanine syndrome [1], is a type of stroke that occurs in the blood vessels supplying the pons, a structure in the brainstem that controls essential processes such as the sleep-wake cycle, movement coordination, breathing, and balance. Lateral Pontine Stroke is more common in adults over the age of 65 [2], particularly those with a history of cardiovascular diseases. Pontine strokes can cause a variety of symptoms, including paralysis or difficulty coordinating movements, depending on which part of the pons is affected. Symptoms may improve over time, depending on the severity of the stroke and the course of treatment. Several methods are available for diagnosing Lateral Pontine Stroke, including computed tomography (CT) scans and magnetic resonance imaging (MRI) to pinpoint the location of the stroke. Additional tests, such as electrocardiograms, carotid ultrasounds, and cerebral angiography, may also be utilized. Furthermore, blood tests can help determine the underlying cause of the stroke. Treatment options include medication and surgery [3].
Introduction
The pons is the second-lowest section of the brainstem, situated above the medulla oblongata. It serves as a critical connection between the brain and the spinal cord, linking the medulla oblongata to the midbrain. Marie-Foix syndrome, also known as Lateral Pontine Syndrome, results from a stroke in the anterior inferior cerebellar artery, which supplies the pons.
Neuroanatomy of the pons
The pons contains key junctions for four of the twelve cranial nerves, located in the dorsal tegmentum, which directly connect to the brain:
- Trigeminal nerve (Cranial Nerve V): Responsible for providing sensations of touch and pain to the face, as well as controlling the muscles involved in chewing.
- Abducens nerve (Cranial Nerve VI): Controls the muscles responsible for eye movement.
- Facial nerve (Cranial Nerve VII): Governs most facial expressions and provides taste sensation from the anterior two-thirds of the tongue.
- Vestibulocochlear nerve (Cranial Nerve VIII): Divides into the vestibular nerve, responsible for balance and spatial orientation, and the cochlear nerve, which governs hearing.
Anatomically, the pons has a bulbous shape and is composed of two major parts: the basis pontis (basal or ventral part) and the pontine tegmentum (dorsal part). The basis pontis consists primarily of white matter tracts with transverse fibers that contribute to the bulk of the pons, while the pontine tegmentum is continuous with the tegmentum of the medulla and midbrain. It contains multiple white matter tracts and gray matter nuclei [4,5].
Figures 1, 2, and 3 show the neuroanatomy of the pons through axial sections taken at the level of the upper, middle, and lower pons, respectively [13].
![Axial section at the level of the upper pons [13].](https://neuropedia.net/wp-content/uploads/2024/08/13-1.jpeg)
Figure 1: Axial section at the level of the upper pons [13].
![Axial section at the level of the middle pons [13].](https://neuropedia.net/wp-content/uploads/2024/08/13-2.jpeg)
Figure 2: Axial section at the level of the middle pons [13].
![Axial section at the level of the lower pons [13].](https://neuropedia.net/wp-content/uploads/2024/08/13-3.jpeg)
Figure 3: Axial section at the level of the lower pons [13].
Epidemiology
Pontine stroke is a common subtype of stroke occurring in the posterior part of the brain. It affects both sides of the brain in about 10 to 33 percent of cases [3].
Pontine strokes account for approximately 7% of all ischemic strokes (pontine infarctions) and 10% of hemorrhagic strokes [6]. Ischemic stroke incidence tends to be higher in men than in women and is more prevalent in Black and Hispanic adults compared to their white counterparts, although this varies by geographic region. However, studies focusing specifically on pontine infarctions are limited [2].
A 2018 review of studies reported a 48.1% mortality rate within 30 days of a pontine stroke [3].
Etiology and Pathogenesis
The lateral pontine syndrome refers to a brainstem stroke affecting the lateral pons, typically due to an infarction in the distribution of the basilar artery and the anterior inferior cerebellar artery (AICA) [7].
Several predisposing conditions can increase the risk of developing this syndrome, including diabetes mellitus, hypertension, atherosclerosis of the basilar artery, dyslipidemia, vertebrobasilar insufficiency, smoking, and a history of heart disease. The risk of ischemic stroke also rises with age.
However, younger individuals are not exempt from the risk of lateral pontine stroke, particularly those with cardiovascular disorders such as cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL), hypercoagulable states, or vertebral artery dissections.
Other common causes of stroke include diseases affecting the arteries, such as small artery disease and large artery atherosclerosis, where plaque builds up and thickens the arterial walls. Additionally, cardiogenic emboli, in which a blood clot from the heart travels to the brain, are also notable contributors to stroke [8].
Figure 4 shows the neuroanatomical distribution of the vascular territories supplied by each cerebral artery [14].
![Cerebral vascular territories for a better understanding of the affected blood supply in the case of lateral pontine stroke [14].](https://neuropedia.net/wp-content/uploads/2024/08/14.jpeg)
Figure 4: Cerebral vascular territories [14].
Clinical Features
Brainstem strokes, including those affecting the pons, can present with symptoms that differ from more typical strokes, which commonly include facial drooping, slurred speech, and unilateral weakness. Given the pons’ role in coordinating balance, breathing, and eye movements, strokes in this area can disrupt these essential functions. Symptoms such as vertigo, dizziness, and severe loss of balance may arise due to the impact on vestibular pathways. These symptoms can sometimes be mistaken for inner ear issues or other non-cerebral conditions, potentially delaying diagnosis. Pontine strokes may also cause slurred speech (dysarthria), double vision (diplopia), and altered consciousness, reflecting the pons’ involvement in cranial nerve function and overall brainstem activity [8].
A lateral pontine stroke may present with sudden weakness on one side of the body, facial deviation, and vomiting. Ipsilateral loss of facial pain and temperature sensation, along with contralateral loss in the arm and leg, is common.
Motor and Sensory Impairments
Pontine strokes often result in motor and sensory deficits. Pure motor hemiparesis involves weakness of the face, arms, and legs on one side of the body (contralateral to the stroke) without other abnormalities. Ataxic hemiparesis, which presents as weakness and ataxia on the same side of the body as the infarction (ipsilateral), is often associated with cerebellar involvement due to their shared blood supply. Additionally, pure sensory deficits may also arise, affecting touch, pain, temperature, pressure, vision, hearing, and taste [6].
Speech and Cranial Nerve Issues
Dysarthria, or difficulty speaking due to impaired control of speech muscles, differs from aphasia, which involves cognitive difficulties with language. Dysarthria-Clumsy Hand Syndrome combines severe dysarthria, dysphagia, facial weakness, and weak hand coordination, typically following internal capsule or pontine strokes.
Cranial nerve paralysis may also occur, impacting areas served by the affected cranial nerves, usually on the same side as the stroke.
Severe Conditions
Locked-in syndrome is a severe condition where the patient experiences tetraplegia (paralysis of all four limbs) and facial muscle paralysis but retains cognitive functions and awareness. Communication is possible only through eye movements if the areas controlling eye movements are intact.
Complications
Common Complications
Pontine infarctions can lead to several common issues. Dysphagia is frequent and may require tube feeding. Urinary incontinence might necessitate catheterization, increasing the risk of urinary tract infections. Post-stroke depression is also common. Aspiration pneumonia is a concern, often resulting from pseudobulbar palsy or locked-in syndrome, which is considered one of the most severe complications.
Long-Term and Neurological Issues
Prolonged immobilization can result in pressure ulcers, deep venous thrombosis, and pulmonary embolism. Persistent motor weakness may lead to a higher risk of falls and long-term disability, often assessed using the Barthel Index, Glasgow Outcome Scale, and the modified Rankin Scale (mRS).
Neurological complications may include cerebral edema, hemorrhagic transformation of the infarcted area, palatal myoclonus, and ongoing neurological deterioration despite treatment [2].
Clinical Evaluation
Patient History and Neurological Examination
The initial step in diagnosing a lateral pontine stroke is a thorough clinical evaluation. The patient’s history and presenting symptoms are crucial.
A detailed neurological examination helps assess motor and sensory deficits, coordination, and cranial nerve function. Key findings in lateral pontine stroke include [6]:
- Motor impairment on one side of the body (contralateral to the stroke)
- Sensory loss affecting the face (ipsilateral) and body (contralateral)
- Dysarthria and potential facial weakness
- Ataxia or loss of balance
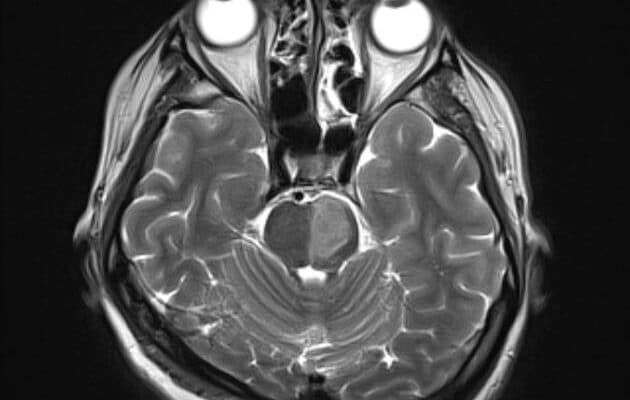
Imaging Studies
Magnetic Resonance Imaging (MRI) is the primary imaging modality for diagnosing a lateral pontine stroke, as it provides detailed information about acute ischemia or infarction in the pons, along with revealing edema, hemorrhage, and structural abnormalities that may explain the patient’s symptoms.
While MRI is more sensitive in detecting early ischemic changes and subtle abnormalities, Computed Tomography (CT) scans are also valuable, especially in acute settings, for quickly ruling out hemorrhagic stroke and identifying large areas of infarction. CT is often used as an initial screening tool, but MRI remains the preferred method for a comprehensive assessment of pontine stroke [8].
Figures 5 and 6 show CT scans of the brain demonstrating infarctions on the left and right sides of the pons, respectively [15,16].
![CT scan of the brain showing infarction on the left side of the pons in a case diagnosed with lateral pontine stroke [15].](https://neuropedia.net/wp-content/uploads/2024/08/15-1-300x300.jpg)
Figure 5: CT scan of the brain showing infarction on the left side of the pons [15].
![CT scan of the brain showing infarction on the right side of the pons in a case diagnosed with lateral pontine stroke [16].](https://neuropedia.net/wp-content/uploads/2024/08/16-300x300.jpg)
Figure 6: CT scan of the brain showing infarction on the right side of the pons [16].
Additional Diagnostic Tests
Magnetic Resonance Angiography (MRA) and Computed Tomography Angiography (CTA) are crucial for evaluating the cerebral vasculature to identify any occlusions or stenosis that could have contributed to the stroke, helping to detect large vessel disease or embolic sources. In cases where more detailed visualization of blood vessels is required or the exact cause of the stroke needs clarification, conventional cerebral angiography may be performed.
Additionally, blood tests play a role in identifying underlying risk factors or conditions contributing to the stroke, such as abnormalities in coagulation profiles (e.g., prothrombin time, activated partial thromboplastin time), lipid levels, and blood glucose levels.
Electrocardiogram (ECG) and echocardiogram are used to detect potential cardiac sources of emboli, such as atrial fibrillation or cardiac thrombi, which might have played a role in the stroke’s etiology [6].
Differential Diagnosis
Treatment and management
Pontine stroke can be severe and requires immediate medical attention. The blockage of blood flow in the arteries supplying the pons, typically due to blood clots, leads to a pontine stroke [9]. Therefore, the primary goal of treatment is to dissolve these clots and restore normal pons activity. Pontine stroke can also result from plaque buildup in the small vessels within the pons [9]. Treatment may involve prescribing aspirin or similar anticoagulants (e.g., dabigatran, warfarin, apixaban) and antiplatelet agents to reduce blood clotting [2].
In emergencies, patients may undergo mechanical thrombectomy (within 24 hours of symptom onset) or thrombolysis (within 4.5 hours of symptom onset). Thrombolysis involves the use of medication to dissolve blood clots, which can be administered intravenously or delivered directly to the clot through a minimally invasive procedure [2].
For hemorrhagic strokes, emergency surgery is required to stop the bleeding and prevent further complications [3, 9].
Management also includes speech therapy to assist with communication and swallowing difficulties, and physiotherapy to address muscle paralysis. In addition, home therapy that keeps the brain stimulated, along with sensory retraining (exposing the skin to different temperatures and textures and sending stimulatory impulses to the brain), may be beneficial [3, 6].
Given the severe impact of pontine stroke on quality of life, including physical, emotional, and mental aspects, therapy and meditation are crucial in managing the disease and achieving the best possible outcomes.
Prevention
For individuals with a history of blood clotting disorders, it is crucial to consult with a healthcare provider regarding appropriate medications or anticoagulants to reduce the risk of pontine stroke.
Additionally, controlling dietary intake by maintaining a balanced diet low in fats, salts, and sugars, combined with regular physical exercise and effective blood pressure management, is vital for stroke prevention. Avoiding tobacco use and limiting alcohol consumption are also important measures in reducing the risk of lateral pontine stroke [3].
Risk factors
The risk factors for pontine stroke are similar to those for strokes affecting other areas of the brain and include several health and lifestyle conditions.
Cardiovascular disease, including coronary artery disease and heart failure, significantly increases stroke risk. The use of certain drugs and an unhealthy diet high in cholesterol and fats contribute to the risk by promoting atherosclerosis. Lifestyle factors such as smoking and excessive alcohol consumption are also major contributors to stroke risk. Hypertension is a critical risk factor, as high blood pressure can lead to the formation of blood clots. Obesity, diabetes, and irregular heartbeats, such as atrial fibrillation, further elevate the risk by affecting blood vessels and promoting clot formation. Additionally, advancing age and a family history of ischemic stroke are important considerations [10].
Managing these risk factors through lifestyle changes, medical interventions, and regular monitoring is essential in reducing the risk of a lateral pontine stroke.
Prognosis
The prognosis for recovery from a pontine stroke is primarily influenced by the size of the stroke. A systematic review by Behrouz (2018) found that while the size of the stroke is the main determinant of recovery, the specific location within the pons also plays a role in the outcome [1]. Additionally, a study by Smith et al. (2022) on recurrent pontine infarction reported rates of recurrence at 4.1% at 1 month, 6.3% at 6 months, and 7.8% at 8 months, highlighting the varying likelihood of stroke recurrence over time [11].
The prognosis for pontine stroke can vary widely. Patients with unilateral pontine stroke, affecting one side of the pons, generally experience a more favorable recovery. Similarly, those with strokes affecting the lateral to mid-pons tend to have a better prognosis. In contrast, patients with bilateral or caudal pontine infarctions often face a poorer prognosis [6]. It is essential to recognize that prognosis can differ significantly based on individual factors and the specifics of each stroke case.
Recent updates
A study published in March 2024 investigated the relationship between cognitive decline and pontine stroke. The primary aim was to identify the characteristics of cognitive impairment and disabilities that occur post-stroke, to enhance clinical diagnostics and rehabilitation interventions.
The study identified a correlation between cognitive decline and damage to brain regions involved in knowledge acquisition and intellectual skills, such as memory, attention, and executive functions. It also examined recovery patterns and cognitive function restoration post-stroke. Findings revealed that while some patients showed improvement in specific cognitive domains, others experienced deterioration and dementia. Factors influencing recovery included the lesion’s location and the patient’s age, with older age generally associated with more severe neurological deficits and poorer recovery.
A significant aspect of the study was the emphasis on employing multimodal neuroimaging techniques to explore the neural mechanisms underlying cognitive decline after a pontine stroke. Techniques used included MRI, Single Photon Emission Computed Tomography (SPECT), and Near-Infrared Spectroscopy.
The study concluded that the techniques used to investigate morphological and neurodegenerative changes due to pontine stroke were effective. MRI results indicated that pontine stroke could disrupt crucial brain circuits, such as the prefrontal-cerebellar circuit, contributing to cognitive decline [12].
References...