Article Title: Zuranolone; A Novel Oral Treatment for Postpartum Depression.
Author: Amani Alfdool.
Editor: Rahmeh Adel.
Reviewer: ُEthar Hazaimeh
Keywords: Postpartum depression, Zuranolone, Brexanolone, Neuroactive steroids, gamma-aminobutyric acid, Neuromodulation, Depression.
Abbreviation: Postpartum depression (PPD), major depressive disorders (MDD), gamma-aminobutyric acid type A (GABAA) receptors, positive allosteric modulators (PAMs), gamma-aminobutyric acid (GABA), selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs).
Abstract
Postpartum depression (PPD) is a serious concern for maternal mental health, and the relationship between a mother and her baby, potentially impacting the child’s growth and cognitive development. Various therapeutic interventions, such as pharmacotherapy, psychotherapy, neuromodulation, and hormonal therapy, among others, are accessible for addressing postpartum depression. While antidepressants have traditionally been utilized in the management of postpartum depression (PPD), recent findings challenge their effectiveness, encouraging a critical need for the exploration of novel therapeutic modalities. In 2023, a breakthrough in the treatment of postpartum depression (PPD) was achieved with the recent approval by the FDA of zuranolone, a selective positive allosteric modulator of the gamma-aminobutyric acid type A (GABAA) receptor. The utilization of zuranolone in postpartum depression (PPD) treatment has the potential to be groundbreaking, as it is the first oral medication to be introduced for this purpose.
This article reviews the clinical significance of zuranolone in alleviating the symptoms of postpartum depression (PPD). Consequently, this treatment option holds promise for enhancing the well-being of mothers, particularly in the context of managing Postpartum depression (PPD).
Introduction
The period following childbirth is widely acknowledged as a difficult phase for mothers, and the occurrence of postpartum depression increases as a woman advances through her life (1). Postpartum depression is typically characterized by intense sadness, anxiety, and fatigue, which are detrimental to a woman’s ability to engage in daily activities, including taking care of herself. Moreover, it affects the motor, cognitive, language, social, and emotional development of infants (2).
Postpartum depression (PPD) is influenced by various risk factors, including demographic characteristics and psychosocial variables. These factors consist of younger age, African-American race, public insurance, single status, lower education level, low occupational prestige, and having multiple offspring (3). Also, intimate partner violence, adverse childhood experiences, self-reported previous psychiatric diagnosis, low social support, and a higher number of stressful life events during pregnancy have shown significant associations with the development of Postpartum depression (PPD)(4). Postpartum depression (PPD) has the potential to sustain over an extended period (5). Consequently, screening for the disease and initiating early intervention is crucial, especially considering that the four to six weeks following delivery are considered a high-risk period (6).
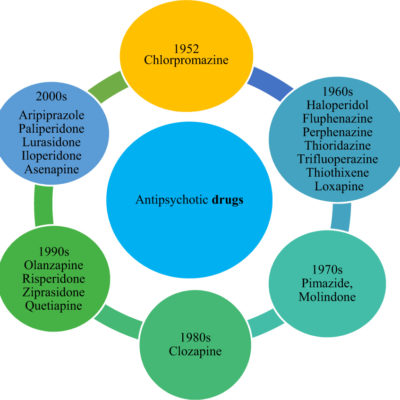
Once postpartum depression (PPD) has been diagnosed, the implementation of psychosocial interventions to enhance self-care, maintain practical and emotional social support, and mitigate the occurrence of stressors should be considered. However, if psychological measures fail to yield positive outcomes, the utilization of antidepressant medication, either as a monotherapy or in conjunction with non-pharmacological interventions, may be warranted (7). The treatment options for postpartum depression (PPD) encompass psychotherapy, antidepressants, hormonal treatments, and neuromodulation. Psychotherapy, specifically cognitive behavioral therapy and interpersonal psychotherapy, has been extensively employed. However, it is important to note that these therapeutic methods have been adapted from the treatment of other depressive disorders. However, recent advancements in comprehending the pathophysiology of postpartum depression (PPD) have resulted in the development of novel antidepressants that target this condition specifically.
As the work to find effective treatments progresses, the admiration of gamma-aminobutyric acid type A (GABAA) receptor selective positive allosteric modulators (PAMs) antidepressants has been increased for managing postpartum depression (PPD)(8). Zuranolone is an outstanding neuroactive steroid and a positive allosteric modulator of gamma-aminobutyric acid type A (GABAA) receptors.
GABAA receptors in modulating PPD
The study of neuroactive steroids and gamma-aminobutyric acid (GABA) extends to various neuropsychiatric disorders, with a particular focus on postpartum depression (PPD) (9, 10). GABA functions as an essential inhibitory neurotransmitter within the central nervous system, exerting significant influence over the regulation of brain activity (11). By interacting with ligand-gated ion channel receptors on the cell membrane, such as gamma-aminobutyric acid type A (GABAA) receptors, neuroactive steroids quickly change neuronal excitability (12). Postpartum depression (PPD) has been associated with GABAergic deficits, which are confirmed by the diminished GABA levels observed in the plasma, CSF, and cortical tissue of women suffering from PPD (11).
By positively modulating the GABAA receptor, Allopregnanolone holds promise as a potential therapeutic approach for the treatment of PPD (13). Brexanolone, an allopregnanolone derivative, has received FDA approval as the first-line medication for postpartum depression (14). Despite its significant promotion in treating PPD, the administration of Brexanolone is constrained by its intravenous route (IV), necessitating a total dosing period of 60 hours (8). Brexanolone infusion requires hospital admission and monitoring due to adverse effects like sedation, disturbed mental state, and loss of consciousness. Also, the use of Brexanolone is contraindicated in end-stage renal disease patients (8). Consequently, more research into alternative treatment options for PPD is needed due to its safety profile, inconvenient administration, and high cost in the US,
presenting a potential barrier to accessing this treatment (14).
Zuranolone
All the challenges proposed by Brexanolone therapy were effectively addressed with the FDA’s approval of zuranolone for the management of postpartum depression on August 4, 2023 (15). Zuranolone takes a different therapeutic approach with its neuroactive properties, it serves as a positive allosteric regulator of the GABAA receptor, carrying the possibility of effectively improving depressive symptoms beyond the capabilities of traditional medications (16). Clinical trials have been carried out to investigate its potential in managing postpartum depression (16). According to a study, zuranolone achieved the third highest position on the cumulative ranking curve (SUCRA) at 58.8% in the context of managing postpartum depression (17).
Zuranolone, a neuroactive steroid, was formulated as an oral medication and functions as a GABAA receptor-positive allosteric modulator, highlighting that Zuranolone is distinct from Brexanolone in oral form. It regulates the function of both synaptic and extrasynaptic GABAA receptors (18). Additionally, it acts rapidly as an antidepressant, with effects observed as early as day 3 during a 15-day treatment trial.
Clinical trials in phases 2 and 3 have shown the effectiveness and safety of zuranolone compared to a placebo in treating outpatient adult women with PPD (19). Additionally, zuranolone has been investigated for major depressive disorder (MDD) beyond the postpartum period (20). Two phase 3 trials for postpartum depression (PPD) have exhibited efficacy, as indicated by HAM-D changes from baseline on day 15 of treatment. The initial phase 3 postpartum depression study examined zuranolone 30 mg/day, while the second study involved zuranolone 50 mg/day (19). Both trials reported a good tolerance of the drug, with mild side effects such as somnolence and drowsiness. Primarily, the results of clinical trials have exhibited marked enhancements in depressive symptoms and a well-tolerated treatment course of zuranolone in women diagnosed with PPD (21). As a result, zuranolone received FDA approval in August 2023 as the first oral treatment for postpartum depression (22).
Zuranolone has been formulated as an oral medication, prescribed once daily for 14 days, considering its drug metabolic and pharmacokinetic (DMPK) profile, to effectively address postpartum depression (23). Since zuranolone is taken orally once daily, it does not require hospital admission, making it more patient-friendly efficacious drug for the treatment of PPD (14). The most frequent side effects associated with Zuranolone are drowsiness, dizziness, diarrhea, fatigue, common cold, and urinary tract infection. It is important to note that the use of this medication may result in suicidal thoughts and behavior, as well as potential harm to a fetus. It is advised that women use effective contraception during treatment and for one week following the treatment as well. The FDA approval for PPD includes a boxed warning regarding the risk of sedation while driving for up to 12 hours post-administration. Additionally, patients are advised to take the medication at bedtime to minimize the sedation side effects. To ensure optimal results, it is recommended to take Zuranolone at a daily dosage of 50mg. This should be done once a day for a period of 14 days, preferably in the evening along with a meal containing fats (22).
Conclusion
Postpartum depression (PPD) poses significant challenges for mothers and infants, highlighting the need for effective pharmaceutical interventions to control the anxiety and stress associated with it. Zuranolone, a positive allosteric modulator (PAM) of the GABAA receptor, offers a targeted solution to this issue. Zuranolone has shown a wide range of benefits in comparison to traditional treatments like selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs). As it provides a quicker onset of action, delivering rapid relief unlike the delayed response seen with conventional therapies. Moreover, zuranolone delivers sustained effects even after discontinuation, surpassing the short-term advantages of standard treatments. Additionally, zuranolone has demonstrated significantly higher rates of remission in patients when compared to traditional therapies. Zuranolone exhibits superiority over brexanolone, as the latter necessitates continuous intravenous (IV) infusion for either 60 or 90 hours, while zuranolone can be taken orally on a daily basis.
Considering that postpartum depression is often overlooked in many regions due to limited awareness and the stigma surrounding depression, zuranolone emerges as a practical choice for mothers, sparing them with the need for prolonged hospitalization that may also negatively impact the well-being of their infants. The demanding administration regimen of Brexanolone therapy may affect patient adherence, whereas zuranolone offers the advantage of easy drug administration, increased flexibility, and improved feasibility for patients. However, certain limitations are associated with zuranolone, such as the relatively small sample sizes utilized in clinical trials and the limited duration of patient exposure, typically lasting 45 days, leaving the relationship between breastfeeding and zuranolone efficacy undiscovered.
References
Read more
1. masroor P, Mehrabi E, Nourizadeh R, Pourfathi H, Asghari-Jafarabadi M. The comparison of the effect of non-pharmacological pain relief and pharmacological analgesia with remifentanil on fear of childbirth and postpartum depression: a randomized controlled clinical trial. BMC Pregnancy Childbirth. 2024;24(1):1–9.
2. Serati M, Carnevali G. Perinatal depression. Clin Cases Psychiatry Integr Transl Neurosci Approaches. 2018;155–70.
3. Wisner KL, Sit DKY, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70(5):490–8.
4. Mersky JP, Janczewski CE. Adverse Childhood Experiences and Postpartum Depression in Home Visiting Programs: Prevalence, Association, and Mediating Mechanisms. Matern Child Health J [Internet]. 2018;22(7):1051–8. Available from: http://dx.doi.org/10.1007/s10995-018-2488-z
5. Ph D, Bergemann N, Ph MDD, Muzik M. A MULTIRISK APPROACH TO PREDICTING CHRONICITY OF. 2011;25(8):718–24.
6. Agrawal I, Mehendale AM, Malhotra R. Risk Factors of Postpartum Depression. Cureus. 2022;14(10):1–8.
7. Stewart DE, Vigod SN. Postpartum depression: Pathophysiology, treatment, and emerging therapeutics. Annu Rev Med. 2019;70:183–96.
8. Edinoff AN, Odisho AS, Lewis K, Kaskas A, Hunt G, Cornett EM, et al. Brexanolone, a GABAA Modulator, in the Treatment of Postpartum Depression in Adults: A Comprehensive Review. Front Psychiatry. 2021;12(September):1–9.
9. Butterfield MI, Stechuchak KM, Connor KM, Davidson JRT, Wang C, MacKuen CL, et al. Neuroactive steroids and suicidality in posttraumatic stress disorder. Am J Psychiatry. 2005;162(2):380–2.
10. Luchetti S, Bossers K, Van de Bilt S, Agrapart V, Morales RR, Frajese GV, et al. Neurosteroid biosynthetic pathways changes in prefrontal cortex in Alzheimer’s disease. Neurobiol Aging [Internet]. 2011;32(11):1964–76. Available from: http://dx.doi.org/10.1016/j.neurobiolaging.2009.12.014
11. Ghit A, Assal D, Al-Shami AS, Hussein DEE. GABAA receptors: structure, function, pharmacology, and related disorders. J Genet Eng Biotechnol [Internet]. 2021;19(1):123. Available from: https://doi.org/10.1186/s43141-021-00224-0
12. Frieder A, Fersh M, Hainline R, Deligiannidis KM. Pharmacotherapy of Postpartum Depression: Current Approaches and Novel Drug Development. CNS Drugs. 2019;33(3):265–82.
13. Chen S, Gao L, Li X, Ye Y. Allopregnanolone in mood disorders: Mechanism and therapeutic development. Pharmacol Res [Internet]. 2021;169(May):105682. Available from: https://doi.org/10.1016/j.phrs.2021.105682
14. Nashwan AJ, Rehan ST, Imran L, Abbas SG, Khan SF. Exploring the clinical potentials of zuranolone in managing postpartum depression: A new therapeutic horizon. Prog Neuro-Psychopharmacology Biol Psychiatry [Internet]. 2024;132(February):110983. Available from: https://doi.org/10.1016/j.pnpbp.2024.110983
15. Parikh S V., Aaronson ST, Mathew SJ, Alva G, DeBattista C, Kanes S, et al. Efficacy and safety of zuranolone co-initiated with an antidepressant in adults with major depressive disorder: results from the phase 3 CORAL study. Neuropsychopharmacology. 2024;49(2):467–75.
16. Porta-Casteràs D, Vicent-Gil M, Serra-Blasco M, Navarra-Ventura G, Solé B, Montejo L, et al. Increased grey matter volumes in the temporal lobe and its relationship with cognitive functioning in euthymic patients with bipolar disorder. Prog Neuro-Psychopharmacology Biol Psychiatry. 2024;132(October 2023).
17. Ahmad A, Awan AR, Nadeem N, Javed AS, Farooqi M, Daniyal M, et al. Zuranolone for treatment of major depressive disorder: a systematic review and meta-analysis. Front Neurosci. 2024;18(April).
18. Hoffmann E, Nomikos GG, Kaul I, Raines S, Wald J, Bullock A, et al. SAGE-217, A Novel GABAA Receptor Positive Allosteric Modulator: Clinical Pharmacology and Tolerability in Randomized Phase I Dose-Finding Studies. Clin Pharmacokinet [Internet]. 2020;59(1):111–20. Available from: https://doi.org/10.1007/s40262-019-00801-0
19. Deligiannidis KM, Meltzer-Brody S, Gunduz-Bruce H, Doherty J, Jonas J, Li S, et al. Effect of Zuranolone vs Placebo in Postpartum Depression: A Randomized Clinical Trial. JAMA Psychiatry. 2021;78(9):951–9.
20. Deligiannidis KM, Citrome L, Huang MY, Acaster S, Fridman M, Bonthapally V, et al. It is illegal to post this copyrighted PDF on any website. J Clin Psychiatry. 2023;77(September):22–7.
21. Zhang Q, Dai X, Li W. Comparative efficacy and acceptability of pharmacotherapies for postpartum depression: A systematic review and network meta-analysis. Front Pharmacol. 2022;13(November):1–10.
22. U.S. Food and Drug Administration [Internet]. 2023 [cited 2024 May 23]. p. 1–2 FDA Approves First Oral Treatment for Postpartum Depression | FDA. Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-first-oral-treatment-postpartum-depression
23. SAMHSA (Substance Abuse and Mental Health Services Administration). Results from the 2019 National Survey on Drug Use and Health : Detailed Tables Prevalence Estimates , Standard Errors , P Values , and Sample Sizes. Subst Abus. 2020;I(August):6–7.
[/read]