Article topic: Antipsychotic Drugs.
Author: Ahmad Aljbali
Editor: Yazan S. Al-Zamer
keywords: psychosis, schizophrenia, depression
OVERVIEW
History
The history of the concept of psychosis is stemmed from the time it was referred to in 1845 to the present day. within a time, it had become synonymous (scientifically not true) with the two terms “psychopathy” and “psychoneurosis”. Soon, all psychiatric disorders became subsumed under its umbrella heading amidst a confusing set of terminology. Psychosis is examined as it then became distinct from psychopathy and neurosis.[1]
Pathophysiology
Based mainly on the dopamine hypothesis that the dopamine pathway changes may result in signs and symptoms of psychosis. As we know the dopamine may be found as a chemical substance or act as neurotransmitters in CNS (the important one). So the dopamine is the messenger between the sender and receiver structures inside the CNS that have receptors for that neurotransmitter. Dopamine receptors may be inhibitory or excitatory. And this theory has its pros and cons and even that the pathophysiology is not well understood generally.
Psychosis (disease)
Psychosis is an abnormal condition of the mind (mental) that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations. Other symptoms may be incoherent speech and behavior that is inappropriate for the situation. There may also be sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. Then Psychosis can have serious outcomes.[2]
Causes
Psychosis has different causes. These include mental illness, such as schizophrenia or bipolar disorder, sleep deprivation, some medical conditions, certain medications, and drugs such as alcohol or cannabis. One type, known as postpartum psychosis, can occur after giving birth (concomitant with conditions). The neurotransmitter dopamine is believed to play a role (dopamine hypothesis). [2] Psychosis may be considered primary if it results from a psychiatric condition and secondary if it is caused by a medical condition.[2]
Diagnosis
The diagnosis of a mental illness requires excluding other potential causes. Testing may be done to check for central nervous system diseases, toxins, or other health problems as a cause.[2]
Treatment
Here the topic which we will focus on may include antipsychotic medication, counseling, and social support (essential role). Early treatment appears better to improve outcomes. Medications appear to have a moderate effect so they are not only the choice. Outcomes depend on the causes.[2]
Pharmacology of psychotic drug
The antipsychotic drugs (also called neuroleptics or major tranquilizers) are used basically to treat schizophrenia, but they are also effective in other psychotic and manic (agitated) states. So these drugs are able to reduce psychotic symptoms in a wide variety of conditions, including schizophrenia, bipolar disorder, psychotic depression, senile psychosis, various organic psychosis, and drug-induced psychosis.[3]
They are not curative and do not eliminate chronic thought disorders, but they often decrease the intensity of hallucinations and delusions and permit the person with schizophrenia to function in a supportive environment. [3]
The antipsychotic drugs are divided into first-(Typical, Classic, conventional, or traditional antipsychotics) and second-generation (atypical, or newer antipsychotics) agents. The first-generation drugs are further classified as “low potency” or “high potency”. This classification does not indicate the clinical effectiveness of the drugs but rather specifies affinity for the dopamine D2 receptor, which, in turn, may influence the adverse effect profile of the drug.[4]
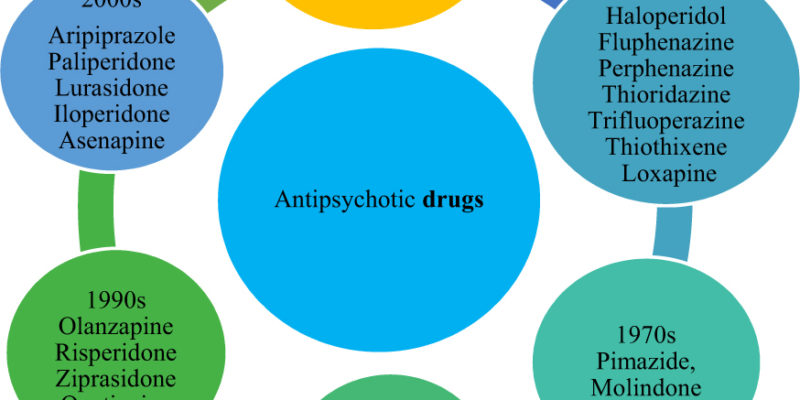
In more details about the generations of the antipsychotic drugs:[4]
The first generation:
They are competitive inhibitors at a variety of receptors, but their antipsychotic effects reflect competitive blocking of dopaminergic D2 receptors. These antipsychotics are classified as high-potency, mid-potency, or low-potency based on their potency for the D2 receptor.
First-generation antipsychotics are more likely to be associated with movement disorders (like side effects) known as extrapyramidal symptoms (EPS, or extrapyramidal side effects), particularly drugs that bind tightly to dopaminergic neuroreceptors, such as haloperidol and other examples.
Examples of first-generation are Chlorpromazine, Haloperidol, and Fluphenazine. We know that each drug has its own mechanism of action, therapeutic uses, and adverse effects. So that we will discuss briefly them.
The second generation:
They have a lower incidence of EPS than the first-generation agents but are associated with a higher risk of metabolic side effects, such as diabetes, hypercholesterolemia, and weight gain. The second-generation drugs appear to owe their unique activity to blockade of both serotonin and dopamine and, perhaps, other receptors. The Second-generation agents are generally used as first-line therapy for schizophrenia to minimize the risk of debilitating EPS associated with the first-generation drugs that act primarily at the dopamine D2 receptor.
The second-generation antipsychotics exhibit an efficacy that is equivalent to and may exceed, that of the first-generation antipsychotic agents. Examples of some drugs are in figure (1).
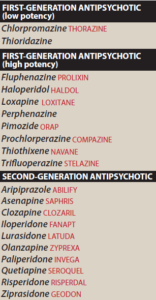
figure (1) Examples of some antipsychotic drugs.
Mechanism of action
Mechanism of action of antipsychotics is exerted at a variety of receptors such as dopamine, serotonin, and others.
Dopamine antagonism:
Dopamine hypothesis- The dopamine hypothesis proposes that the disorder is caused by a relative excess of activity of the neurotransmitter dopamine in specific neuronal tracts in the brain. So, all of the first-generation and most of the second-generation antipsychotic drugs block D2 dopamine receptors in the brain and the periphery.[4]
Remember that the dopamine pathways in the brain are fives pathways: [5]
1. The first pathway—the one most closely related to behavior and psychosis—is the mesolimbic-mesocortical pathway which projects from cell bodies in the ventral tegmentum in separate bundles of axons to the limbic system and neocortex.
Note that each pathway has its own beginning and ending inside the brain.
2. The second pathway—the nigrostriatal pathway— blocking of the D2 receptors in the nigrostriatal pathway is responsible for EPS.
3. The third pathway is the tuberoinfundibular pathway that the Dopamine released by these neurons physiologically inhibits prolactin secretion from the anterior pituitary.
4. The fourth pathway is the medullary-periventricular pathway that may be involved in eating behavior.
5. The fifth pathway is the incertohypothalamic pathway.
Serotonin receptor–blocking activity: [6]
Most of the second-generation agents appear to exert part of their unique action through inhibition of serotonin receptors (5-HT), particularly 5-HT2A receptors.
Therapeutic uses[4]
1. Treatment of schizophrenia: The antipsychotics are considered the only efficacious pharmacological treatment for schizophrenia specifically.
2. Prevention of nausea and vomiting: Older antipsychotics are useful in the treatment of drug-induced nausea.
3. Other uses: Antipsychotic drugs can be used as tranquilizers (major tranquilizers) to manage agitated and disruptive behavior secondary to other disorders.
Absorption and metabolism[3]
After oral administration, the antipsychotics show variable absorption that is unaffected by food and these agents readily pass into the brain and have a large volume of distribution. They are metabolized to many different metabolites, usually by the cytochrome P450 system in the liver.
Adverse effects[3][4][7]
Adverse effects of antipsychotic drugs can occur in practically all patients and are significant in about 80%.
- Extrapyramidal effects
The inhibitory effects of dopaminergic neurons are normally balanced by the excitatory actions of cholinergic neurons in the striatum. Blocking dopamine receptors alters this balance, causing a relative excess of cholinergic influence, which results in extrapyramidal motor effects.
- Neuroleptic malignant syndrome
This potentially fatal reaction to antipsychotic drugs is characterized by muscle rigidity, fever, altered mental status and stupor, unstable blood pressure, and myoglobinemia.
- Tardive dyskinesia (TD)
Long-term treatment with antipsychotics can cause this motor disorder. Patients display involuntary movements, including bilateral and facial jaw movements and “fly-catching” motions of the tongue. A prolonged holiday from antipsychotics may cause the symptoms to diminish or disappear within a few months.
- Other effects
Drowsiness occurs due to CNS depression and antihistaminic effects, usually during the first few weeks of treatment. Confusion sometimes results and so on.




