Article Topic: Secondary Stroke Prevention
Author: Manar Ezzat Mahmood
Editor: Haneen A. Banihani, Haneen Al-Abdallat
Reviewer: Neebal Algallab
Keywords: Embolic, hemorrhage, infarction, hypertension.
Overview
Stroke is a neurological deficit attributed to focal injury of the central nervous system (CNS) due to a vascular cause and is considered a significant cause of disability and death worldwide.1
Stroke can affect the old and the young, though less commonly published, but young stroke patients are faced in clinical practice and have a disproportionately large economic impact.2
Stroke recurrence is defined as an event resulting in a neurological deficit different from the initial stroke, as it may involve a different anatomic site or vascular territory or a different stroke subtype from that of the initial stroke. 3,4 Risk of recurrence poststroke is higher in the first year 5,6 which explains the high average annual risk of recurrence recorded in studies with short follow-up compared to those of more extended follow-up periods. The risk of recurrence following primary intracerebral hemorrhage is similar to that following cerebral infarction.7
Strokes pose a significant conflict for survivors due to the risk of recurrence, which may be the final insult to regaining independence. 8,9 Recurrence in the immediate post-stroke period prolongs hospital stay and significantly increases neurological disability and the chance of death. 10
Epidemiology
Stroke is the second leading cause of death globally11. It has a global burden that is increasing dramatically. Current data indicate that 16.9 million people suffer a stroke every year, representing a global incidence of 258/100,000/year, with men having an incidence that is 1.5 times higher than women.12
Cultural and environmental mechanisms play a role in racial-ethnic stroke disparities, including socioeconomic class, access to care, discrimination, and cultural variations in risk factors. It is observed that blacks in the U.S. have higher stroke incidence and higher death rates for all stroke subtypes compared to other racial groups. 13
Generally, trends in stroke incidence and mortality rates have decreased in the recent decades in high-income countries, and this reflects reasonable control of risk factors, as well as an improvement in life expectancy. The opposite has been reported in low-to-middle-income countries 14
Etiology and Pathogenesis
Strokes can be subdivided into ischemic and hemorrhagic, with ischemic strokes being more prevalent than hemorrhagic, making up approximately 80% of all strokes. 15
Ischemic stroke is when a vessel is occluded and can be broadly subdivided into thrombotic and embolic strokes. Damaged areas of an atherosclerotic plaque can cause a blood clot to form, blocking the blood vessel hence a thrombotic stroke. Embolic strokes are blood clots or debris from elsewhere in the body that blocks a cerebral artery, typically from the heart valves.
Further sub-classifications are
- Large artery disease; atherosclerosis of large vessels.
- Small vessel disease: these changes happen due to chronic diseases, such as diabetes, hypertension, hyperlipidemia, and smoking.
- Embolic stroke: which could be due to atrial fibrillation
- Strokes of determined and undetermined etiologies.
In ischemic strokes, a volume of functionally impaired but structurally intact tissue surrounds the ischemic region; this tissue is known as the ischemic penumbra. 16 Also, in the core, where blood flow is most severely restricted, excitotoxic and necrotic cell death occurs within minutes.
As for the periphery of the ischemic area (the penumbra), where collateral blood flow is present, buffering of the full effect of stroke can be seen; hence the degree of ischemia and outcome of individual cells is dependent on the timing of reperfusion.17 The penumbra is the site for therapeutic interventions as it hosts a cascade of neurochemical events disrupting ion homeostasis.16
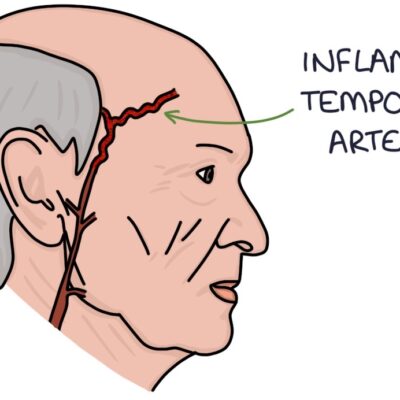
As for the second type of stroke, the hemorrhagic (intracerebral) stroke mostly happens due to pre-existing or newly diagnosed hypertension or could be due to intracranial vascular malformations like cavernous angiomas.
Pathogenesis of ischemic stroke
Variable pathological changes occur to the affected tissue to eventually reach apoptosis, Initially, excitotoxicity, excitotoxicity, and ionic imbalance:
The brain requires large amounts of oxygen to generate sufficient ATP by oxidative phosphorylation to maintain and restore ionic gradients, e.g., Na/K ATPase. This ion pump maintains the high intracellular K+ concentration and the low intracellular Na+ concentration, which are essential for the propagation of action potentials.
When ischemia happens, the mitochondria are incapable of generating ATP due to oxygen depletion; hence when neuronal depolarization happens, the neuron is incapable of restoring resting potential, usually done through the Na+/K+ ATPase. 18 Alongside the Na intracellular increase, Ca++ increases as well since plasma membrane Ca++ ATPase fails to maintain a normal low Ca++ concentration intracellularly.17
Membrane depolarization also releases neurotransmitters like glutamate, which plays a crucial role in ischemic pathology. The sodium-dependent glutamate transmembrane porters of presynaptic and postsynaptic membranes maintain a large concentration gradient. Membrane depolarization and sodium accumulation inside the cells during ischemia causes the reversal of glutamate transporters allowing glutamate to exit the cell along its concentration gradient. 17
This increased synaptic glutamate concentration leads to the activation of N-Methyl-D-aspartate (NMDA) and alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors. NMDA receptors are calcium-permeable, further exacerbating intracellular calcium overload (excitotoxicity). 19
Another factor that further exacerbates calcium overload is acidosis, one of the consequences of anaerobic metabolism of ischemia; hyperglycemia increases lactate in the ischemic environment, further depressing PH. 17
Peri-infarct depolarization
In the affected brain tissue’s core region, cells undergo anoxic depolarization and never repolarize. Cells in the penumbral region can repolarize, but at the expense of further energy consumption, they depolarize once again in response to the increase of glutamate or K+ levels, or both, which accumulate in the extracellular space. This cycle leads to repetitive depolarizations, also called ‘peri-infarct depolarizations.’ 20
Oxidative and nitrative stress
High levels of intracellular Ca++, Na+, and ADP cause the mitochondria to produce high levels of reactive oxygen species, which the brain is especially vulnerable to due to the low endogenous antioxidant levels in neurons. 21
The abundant oxygen radicals destroy cellular macromolecules signaling cells to undergo apoptotic cell death. 22
Workup and diagnosis
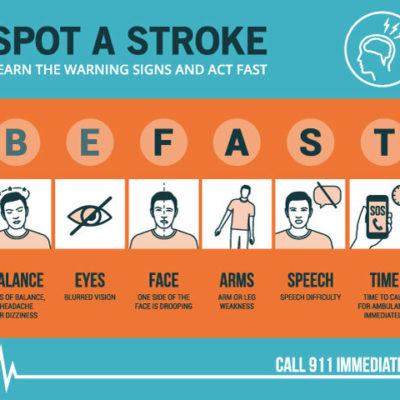
When comparing ischemic stroke to intracerebral hemorrhage, it is found that the most common feature is its acute onset compared to intracerebral hemorrhage, which gradually worsens. 25
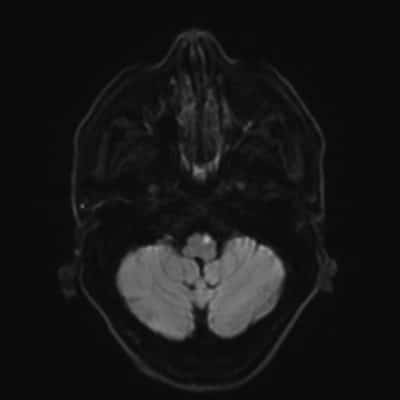
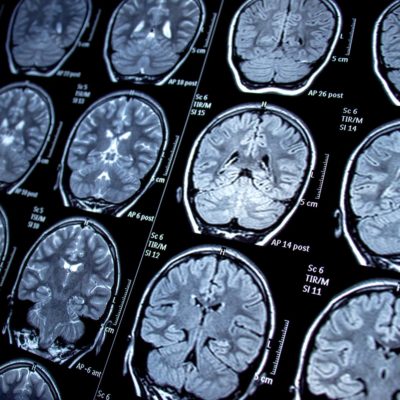
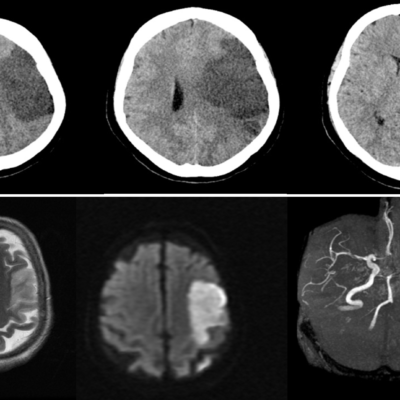
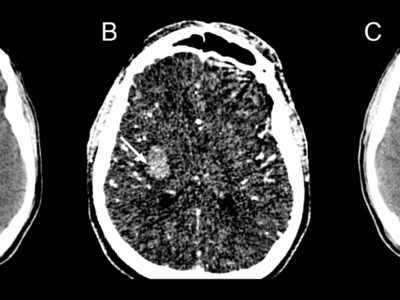
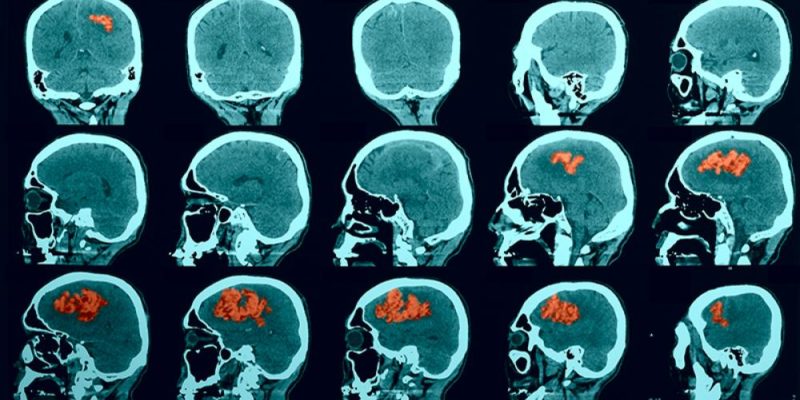
All patients with stroke symptoms should undergo urgent neuroimaging with non-contrast computed tomography (CT) or MRI.26 To distinguish between intracerebral hemorrhage and ischemic stroke, patients should undergo neuroimaging since both entities are characterized by “acute onset of focal symptoms.” 25
MRI scans have a better resolution than CT scans; however, they are less available, more expensive, and can’t be used in patients with implanted devices, e.g., pacemakers and metallic stents. 25
MRIs are recommended if the patient is within the time window of acute stroke intervention and if they can be obtained as fast as a CT scan. If not, then CT scans are the recommended modality because acute stroke treatments should not be delayed for detailed imaging when both, the history and physical presentation, are consistent with acute stroke. 27
It is worth mentioning that strokes can sometimes be confused with stroke mimics and are considered a differential diagnosis. The duration of the symptoms mainly distinguishes strokes from Transient ischemic attacks (TIA), a focal ischemic neurologic event resolving within 24 hours. 29

FIGURE (1): AXIAL NON-CONTRAST CT SCAN OF RIGHT FRONTOPARIETAL HEMORRHAGE WITH SURROUNDING EDEMA Case courtesy of Dr. Derek Smith rID: 34366.
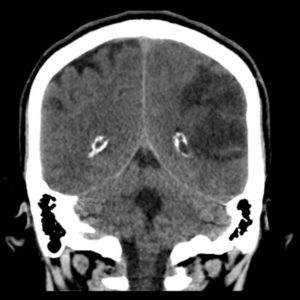
FIGURE (2): CT SCAN SHOWING TWO REGIONS OF ISCHEMIC STROKE IN THE TERRITORY OF THE LEFT MIDDLE CEREBRAL ARTERY. Case courtesy of Dr. David Cuete rID: 26882
Prevention of stroke
One of the best ways to primarily prevent Strokes is by making healthy lifestyle choices:
- Choosing a healthy diet.
- Bearing a healthy weight.
- Maintaining physical activity.
- Avoiding smoking.
- Limiting alcohol.
Secondary prevention of stroke
-
Antithrombotic therapy:
Aspirin: 50-325 mg daily is the recommended initial therapy to prevent the recurrence of an ischemic stroke. The major adverse effect of using aspirin is gastrointestinal bleeding, its prevalence increases when the dose increases 39. If the patient has recurrent strokes during aspirin therapy, increasing the aspirin dose won’t cause a difference as there is no evidence that this increase will decrease the risk of another event 40. Note that Aspirin is the most cost-effective therapy option.
Clopidogrel: monotherapy of 75 mg daily is recommended and can also be used in patients allergic to aspirin 40. Clopidogrel is as safe as Aspirin, with fewer bleeding episodes41. Effectiveness may be decreased with the use of proton pump inhibitors because of the possible cytochrome p450 2C19 interactions. Hence, patients are recommended to use histamine H2 blocker or pantoprazole because of its decreased effects on CYP2C19. 42
Dipyridamole: Dipyridamole is a ‘mild’ antiplatelet agent compared with the more ‘aggressive’ antiplatelet agent clopidogrel. The more modest platelet inhibition provided by Dipyridamole is better suited for secondary prevention in stroke/TIA patient populations and is less likely to cause adverse bleeding complications. 43. Dipyridamole exerts antithrombotic effects, at least partially, through the vessel wall 36. It also has antioxidant 44, anti-inflammatory 45, and anti-proliferative properties46. However, Dipyridamole is associated with a headache that may cause the patient to discontinue the medication 47. Dose titration by initiating therapy with once-daily dosing may help to overcome that headache48.
Aspirin Plus Clopidogrel:
- The CHANCE trial (Clopidogrel in High-Risk Patients with Acute Nondisabling Cerebrovascular Events) was a clinical trial that aimed to evaluate the effectiveness of clopidogrel alone in preventing recurrent stroke in high-risk Chinese patients who have had a minor ischemic stroke or high-risk TIA 49. The trial was conducted in China and enrolled over 5,000 patients. The results of the trial showed that the use of clopidogrel for 21 days reduced the risk of recurrent stroke by 25% compared to placebo. The trial supports the use of clopidogrel for 21 days in this population to reduce the risk of recurrent stroke, without increasing the risk of major bleeding.
- The POINT trial (Platelet-Oriented Inhibition in New TIA and Minor Ischemic Stroke) was a clinical trial that aimed to evaluate the effectiveness of combining two antiplatelet drugs, clopidogrel and aspirin, in preventing recurrent stroke in patients who have had a minor ischemic stroke or high-risk TIA. The trial was conducted internationally and enrolled over 20,000 patients. The results of the trial showed that the combination of clopidogrel and aspirin reduced the risk of recurrent stroke by 21% compared to aspirin alone. Additionally, the combination therapy was found to be safe, with no increase in major bleeding events. The POINT trial provided strong evidence for the use of combination antiplatelet therapy in patients with minor ischemic stroke or high-risk TIA, to reduce the risk of recurrent stroke.
However, due to the increased risk of bleeding, this combination is not recommended for long-term use (more than 2 or 3 years) 40 Use of each drug alone did not improve recurrent stroke or TIA rates, and the combination increased bleeding. 50
Aspirin/Dipyridamole: 25 mg/200 mg twice daily is indicated as initial therapy for prevention of ischemic stroke recurrence and after TIA40. This combination, although not as well tolerated as aspirin monotherapy, was as effective as Aspirin alone for secondary stroke prevention40.
The selection of appropriate therapy depends not only on efficacy but also on the side-effect profile of antiplatelet agents, affordability, and the patient’s preference51.
Secondary stroke prevention mechanisms in specific underlying pathologies:
In cardioembolism, where embolism from the heart accounts for around 25% of ischemic stroke cases, these occur in atrial fibrillation, cardiomyopathy, myocardial infarction, left ventricular thrombus, valve prostheses, and patent foramen ovale.
- Atrial fibrillation: it accounts for 10% to 12% of all ischemic strokes. 52 Occult atrial fibrillation may be the underlying mechanism for up to one-third of cryptogenic strokes 53. For patients with non-valvular atrial fibrillation and adequate renal function, DOACs are indicated. 54 As for patients with valvular atrial fibrillation or impaired renal function, warfarin is to be used.55
- MI and left ventricular thrombus: VKA anticoagulation for three months is indicated for secondary prevention after stroke due to LV thrombus.
- Cardiomyopathy: Patients with dilated cardiomyopathy are at increased stroke risk due to turbulent blood flow, stagnation, and occult thrombus formation. Anticoagulation with warfarin is a way for secondary prevention. Atrial cardiopathy is an emerging mechanism for cardioembolic stroke and is under investigation.52
- Prosthetic heart valve: Vitamin K antagonists are recommended for secondary prevention. The ideal International Normalized Ratio (INR) range depends on valve position and history of prior embolism.52
- Patent Foramen Ovale (PFO): PFO alone is associated with cryptogenic stroke, especially in younger patients (<55) with a substantial right to left-sided shunting and atrial septal aneurysm. PFO closure may be considered for long-term secondary stroke prevention.52
- Hypercholesterolemia: Low-density lipoprotein cholesterol (LDL-C) is a risk marker for ischemic stroke.56 It has been shown that statin therapy reduces the risk of stroke recurrence.57 First-line statins like atorvastatin or rosuvastatin, are indicated for patients following ischemic strokes regardless of their cholesterol level 58, as it has been reported that statins improve all-cause mortality, functional outcome, and the risk of stroke regardless of type. 59
- Carotid artery stenosis and reperfusion interventions: Two therapeutic procedures are available: carotid endarterectomy (CEA) and carotid artery angioplasty and stenting (CAS). CEA is a surgical intervention in which atherosclerotic plaque is removed from the internal carotid artery. CAS is a percutaneous, minimally invasive approach in treating carotid artery stenosis.57 In older patients, CAS is associated with a higher risk of death and stroke. 60
- Stroke due to coagulation disorders: If a patient is found to have abnormal findings on coagulation testing after primary ischemic stroke or TIA if anticoagulation therapy is not administered, Antiplatelet therapy is recommended.40
- Blood Pressure Management: The targeted blood pressure should be less than 140 mmHg systolic.58 After a stroke, ACE inhibitors, calcium channel blockers, and thiazide diuretics are first-line options for blood pressure control,61 with beta blockers inferior to other anti-hypertensive drugs. 62
Risk factors of stroke recurrence:
Unmodifiable risk factors:
- Age
- Previous history of a cerebrovascular event, especially among older stroke patients compared to younger ones. 63
- Stroke subtype; ischemic stroke subtypes are significant independent predictors of stroke recurrence.64
Modifiable risk factors:
- Hypertension65
- Atherogenic dyslipidemia (AD) and hyperlipidemia65
- Diabetes mellitus65
- Atrial Fibrillation.66
Prognosis:
Stroke severity is one of the most critical determinants of the prognosis of the outcome. Stroke severity is correlated with diastolic blood pressure and the serum cholesterol level in a way in a direct way. Hence, measurement and control of these prognostic factors help assess stroke outcomes and improve stroke rehabilitation.67
Prognosis is worse for those with intracerebral and subarachnoid hemorrhage because the 1-month mortality is especially high, approaching around 50%. The primary cause of early mortality is neurological deterioration, but later deaths are more commonly associated with cardiac disease or stroke complications.68
Recent Findings:
A global study into the causes of stroke found that one in 11 survivors experienced a period of extreme emotions in the hour leading up to the stroke. In a research analysis of behavioral patterns in patients who suffered an ischemic stroke, the most common behavioral patterns were anger and emotional upset and were linked to an approximately 30% increase in the risk of stroke one hour after an episode. 69
Neurons do not regenerate, though the brain can sometimes remap its neural pathways to restore some visual function after a stroke, the process is slow and inefficient and never happens for some patients. Stem cell therapy can help by reprogramming the local glial cells into neurons without the need to implant new cells, which means there is no immunogenic rejection.70
References...