Article Title: Rumination Disorder
Author: Lujain Al Badareen
Editor: Ihda Mahmoud Bani Khalaf, Sadeen Eid.
Reviewer: Ethar Hazaimeh
Keywords: rumination syndrome, eating disorder, Gastric regurgitation, Functional gastrointestinal disorder.
Overview
The term rumination, which refers to both humans and animals, is derived from the Latin ruminor, meaning “to take out of the throat” or “to chew out”(1) it is a normal process in animals known as ruminants, such as cows and goats. (2) Rumination syndrome is a purposeful gastrointestinal sickness characterized by the aid of using repetitive handy regurgitation of lately ingested meals into the mouth, accompanied by the aid of using a brand new episode of chewing and then swallowing or expelling the bolus, which typically does not taste acidic or bitter because it occurs a few minutes after eating. (3)
Rumination syndrome could have an impact on every child and adult and is classified via Rome IV as functional gastrointestinal disorder criteria and as an eating disorder according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-V). (4) It can result in significant impairments, including medical complications (eg, tooth damage, weight loss, electrolyte imbalance) and psychosocial complications (eg, avoidance of work or social meals). (5,6)
The diagnosis includes important and common features such as The episode tends to recur until the belching material becomes acidic, and the taste of the regurgitated material is usually pleasant to the patient. (2) Doctors frequently misdiagnose it as refractory gastroesophageal reflux disease or recurrent vomiting, often resulting in a prolonged diagnostic delay. (7)
Epidemiology
The exact prevalence and incidence of rumination disorder are uncertain as different diagnostic criteria are used to diagnose depending on the clinical setting,(8) as well as patients take years to be accurately diagnosed and tend to see numerous physicians leading to sparse inaccurate data. (2) Even though it’s considered a rare disorder, its true prevalence is most likely underestimated, given the lack of recognition of said pathology by both clinicians and patients. (3)
Using the Rome II criteria, the authors of the Canadian study reported a prevalence of 0.8% (95% confidence interval 0.3%-1.3%) in the general population using the questionnaires. (9) The global prevalence of functional gastrointestinal pathologies, according to the Rome IV criteria, was established in a recently published multicenter study, describing a prevalence of rumination syndrome of 2.8% (3.1% women, 2.5% men) through an online survey and a prevalence of 1.1% (1.4% women, 0.8% men) through personal interviews. (10) The prevalence of rumination syndrome is higher in patients with fibromyalgia or eating disorders and might reach 7-8%. (11)
In a study on a pediatric population from 4 provinces of Sri Lanka, 2,160 children and adolescents, between the ages of 10 and 16 years, were surveyed, utilizing the Rome III criteria, prevalence obtained by questionnaire was 5.1% and was similar in boys and girls (5.1% and 5%, respectively). (3) Rumination syndrome is suspected of playing a more significant role in the treatment-refractory gastrointestinal reflux disease, nausea, and vomiting. (12)
Etiology
The etiology of rumination disorder is probably multifactorial; However, the proper motives are rarely known. (8) Several risk factors have been associated with the condition, which include all the following:(13)
- Emotional neglect (infants). (8)
- Emotional stresses. (14)
- Presence of mental health diagnoses such as obsessive-compulsive disorder, anxiety, depression, adjustment disorder, post-traumatic stress disorder, and attention deficit-hyperactivity disorder (ADHD). (15)
- Developmental delay. (8)
- Fibromyalgia.(11)
- Rectal evacuation disorder. (7)
Pathophysiology
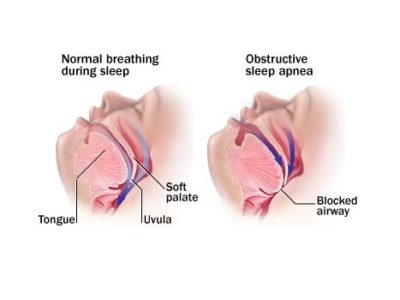
The pathophysiology of rumination syndrome is not fully understood and involves several overlapping mechanisms,(8) the primary mechanism and key event include an often unperceived increase in the stimulation of all abdominothoracic muscles during eating or the postprandial period, increasing the intra-abdominal pressure and negative intrathoracic pressure. (8)
Gastroduodenal manometry and more recently the high-resolution esophageal impedance manometry technique have demonstrated this retrograde gastric flow content that reaches the buccal cavity in patients presenting with rumination is produced due to the simultaneous combination of elevated intra-abdominal pressure and negative intrathoracic pressure, resulting in an esophagogastric gradient in the direction of the oral cavity. (3)
In high-resolution postprandial esophageal impedance manometry, gastric pressure follows the ruminative phenomenon, which in most cases is typically greater than 30 mmHg of proximal reflux episodes,(16) which is associated with upper and lower esophageal sphincter relaxation at the time of gastric pressurization. (3) Those observations reveal that the increase of intra-abdominal pressure, alone, cannot explain the rumination phenomenon and that upper and lower esophageal sphincter relaxation most likely plays a major role in that process. (17,18)
In the comparison of rumination patients with controls, utilizing the gastric barostat test, the patients with rumination syndrome presented with more nausea and abdominal bloating sensation than the controls. (3) At 4 and 8 mmHg of gastric distension pressure, the lower esophageal sphincter tone was more reduced in those patients than in the controls, suggesting greater gastric sensitivity as well as lower esophageal sphincter relaxation during the gastric distension maneuver. (3) Nonetheless, accommodation and gastric emptying were within normal ranges in the majority of patients with rumination syndrome. (19)
Electromyographic studies of the abdominal muscles have shown that gastric insufficiency is due to the maneuver of sudden contraction of the intercostal muscles, together with the contraction of the anterior abdominal muscles. (20) The simultaneous activation of all abdominothoracic muscles in those patients can be appreciated as a characteristic “R” or retrograde wave on electromyography. (8)
In a group of 5 patients with rumination syndrome, diagnosed by the Rome III criteria, and monitored with high-resolution esophageal impedance manometry and videofluoroscopic recording to evaluate the barrier of the gastroesophageal junction in rumination episodes, the ascension of the gastroesophageal junction was observed from the abdominal cavity to the thoracic cavity, generating a “pseudo-hernia” with gastric content and air. (3) However, the importance of that observation is still being disputed, especially because it has also been described in healthy persons during physical activity. (21) Prevalence of sliding hiatal hernia was observed in 50% of the cohort of both a rumination syndrome group and a gastroesophageal reflux disease group. (16)
According to patterns observed in high-resolution esophageal impedance manometry, there are 3 rumination variants have been described:(16) Primary rumination: characterized by an increase in intra-abdominal pressure that precedes retrograde flow from the stomach into the esophagus. (3) Secondary rumination: similar to the primary but the increase in abdominal pressure follows an event of gastroesophageal reflux. (3)
Rumination associated with supra gastric belching: produced by a mechanism similar to that of a supra gastric belch, in which the aboral movement of the diaphragm creates subatmospheric pressure in the esophageal body and the upper esophageal sphincter relaxes, the air then enters the esophageal body, which can be seen as increasing in impedance toward the oral cavity, after which the air is rapidly (in less than a second) expelled from the esophageal body and is manifested as a return to baseline impedance. (3)
The increase in intra-abdominal pressure is caused by the expulsion of air and precedes the reverse flow of gastric contents. (3) The maintenance of rumination syndrome is often associated with psychosocial diseases. (8) Several smaller studies suggest that many patients with rumination syndrome have a higher burden of underlying somatic disorders, depression, or even anxiety. (2,22) Rumination might be maintained because it provides (pain) relief or aid in weight control. (23) A pathophysiologically distinguished subtype of rumination syndrome is infantile rumination, which is related to emotional neglect. (24,25)
Diagnosis
Histopathology
Duodenal biopsies were analyzed by Halland et al. (26) from 22 patients diagnosed with rumination and compared with 10 controls. Histological analysis showed that patients with rumination syndrome had mild eosinophilia and an increased number of intraepithelial lymphocytes compared to controls. (8)
The authors speculate that the muscle mechanisms leading to rumination could be in the context of low-grade inflammation, but further research is needed to confirm what the hypothesis said. (27)
evaluation
According to the ROME-IV criteria for rumination, the diagnosis can be made based on clinical findings without invasive testing. (8) In contrast, the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) criteria require that repeated regurgitation shouldn’t be due to a medical condition which most often requires some form of testing for exclusion. (8)
Moreover, as many patients commonly wait years to be accurately diagnosed, some patients are disappointed about the diagnosis of the functional gastrointestinal disorder and objective tests help patients better understand the diagnosis of rumination. (28,29)
The recommended evaluation of patients suspected of having rumination disorder includes:(8)
- Assessment of potential underlying eating disorders. (8)
- Endoscopy and-or CT enterography to exclude mechanical obstruction. (8)
- High-resolution esophageal manometry (HRIM) with impedance testing (children and adults). (8)
- Electromyography [EMG] of the abdominothoracic muscles:(8) will show a characteristic spiking of activity during episodes of rumination. (30)
- Gastric emptying studies and pH studies are not necessary for diagnosis but are recommended if clinical symptoms are atypical. (8)
Diagnostic and Statistical Manual of Mental Disorders (DSM-V) Criteria for Rumination Syndrome
- Repeated belching for at least a month is a hallmark. (8)
- The repeated regurgitation is not due to an underlying general medical condition (e.g., GERD, pyloric stenosis, etc.). (8)
- The behavior does not occur exclusively in the course of anorexia nervosa, bulimia nervosa, binge-eating disorder (BED), or avoidant/restrictive food intake disorder. (8)
- If occurring in the presence of another mental disorder (e.g., intellectual developmental disorder) or general medical condition (including pregnancy), it is severe enough to warrant additional clinical attention. (8)
Clinical characteristics
When doctors suspect a patient of having rumination syndrome, the predominant symptom is the rapid 0nset of effortless postprandial regurgitation, typically within 10 minutes of finishing a meal. (31,32) Regurgitation can be produced, even if the patient only ingested liquids, which favors the regurgitation of previously ingested solid foods. (33) Episodes tend to persist for 1 or 2 hours after the meal, and even when they occur within that period, the regurgitated material consists of partially digested foods that are recognizable by their flavor. (3) Regurgitation is often triggered by a sensation of abdominal discomfort. (3)
To distinguish rumination from vomiting, regurgitation episodes in rumination syndrome are usually not preceded by nausea and when a patient vomits, it is difficult to keep the content in the mouth due to the intensity of the impulse, rapidly expelling it. (3)
Some individuals with rumination syndrome have reported postprandial dyspeptic symptoms such as bloating or heartburn(34) and early satiety was reported in 3/4 of patients. (27) Other symptoms, such as heartburn, abdominal pain, diarrhea, and/or constipation, are less frequent but don’t rule out the diagnosis. (3) On the other hand, nocturnal regurgitation, dysphagia, or symptoms that aren’t close to meals make the diagnosis less likely. (33)
In some patients, doctors have described a provocative event before the diagnosis of rumination, such as Illness or psychosocial stress related to divorce, death in the family, or problems at school or work. (35)
Complications
Rumination syndrome is considered a mild disease(15,36) but can cause mental and physical problems that affect the patient’s quality of life. (35) Frequent regurgitations can also result in significant weight loss (especially in adolescents) and can lead to the diagnosis of an eating disorder in the form of rumination syndrome. (37)
Among the complications associated with this syndrome, dental erosions have been detected in up to 77% of children(38) and halitosis has been described as a reason for referral. (15) Research has found that patients with rumination syndrome often have accompanying anxiety, depression, and somatization necessitating long-term cognitive behavioral therapy to help with symptoms. (8)
Treatment
The therapeutic strategy begins with an adequate explanation to the patients about the nature of the pathology, commenting to them that it corresponds to a benign functional disorder, describing the underlying mechanisms that produce it so that the patients take an active role in the management of the condition. (3)
The available therapies focus on increasing pressure in the lower esophageal sphincter or decreasing gastric pressure produced by the contraction of the striated musculature of the abdominal wall. (3) Diaphragmatic breathing is the first-line treatment. (8) Diaphragmatic breathing reduces the postprandial intragastric pressure and increases the pressure of the gastroesophageal juncture zone, so restoring the pressure gradient to that level. (17) It works by beginning a mechanism that competes with the acquired and unperceived contractions of the abdominothoracic muscles. (8) The patients are instructed to place one hand on the abdomen and the other on the chest. They are then told to inhale slowly through their nose, only raising the hand on their stomach and keeping the hand on their chest still as they inhale. (3) The patient then exhales slowly through the mouth. (3) Each inhalation and exhalation should be slow and complete, to carry out 6 to 8 respirations per minute. (3) This technique can be taught to patients in either a supine or seated position, “as patients normally eat”. (39) The patients are typically instructed to do the diaphragmatic breathing exercises immediately after a meal and continue them for ten to fifteen min or more until the regurgitative sensation is resolved. (3)
Pharmacological treatment for rumination syndrome should be reserved for patients whose initial behavioral therapy has failed. (8) Pauwelle et al. indicated in a small cross-over study that baclofen 10 mg three times a day reduces flow events and improves patient-reported symptoms in rumination syndrome. (40,41) Baclofen is a gamma-aminobutyric acid type B (GABAB) that is capable of reducing the transitory relaxations of the lower esophageal sphincter and increasing the pressure of the lower esophageal sphincter in healthy individuals and patients with gastroesophageal reflux disease. (42,43) Baclofen crosses the blood-brain barrier (BBB) and has a variety of side effects related to the central nervous system, including confusion, dizziness, lightheadedness, sleepiness, weakness, and tremors. (3) In general, a 5 to 10 mg initial dose at bedtime is recommended and can be increased to 10 mg, three times a day, with careful monitoring in relation to secondary effects. (3)
Patients with rumination syndrome have also used Tricyclic antidepressants (TCAs) together with diaphragmatic breathing for at least 3 months. (3) The most widely used tricyclic antidepressant was nortriptyline, starting at a dose of 10 mg at night, with a weekly increase of 10 mg, until achieving symptom improvement, with a minimum of adverse effects. (35) Tack et al. indicated in a cross-over study for functional dyspepsia that buspirone has positive gastric fundus relaxation properties, which might benefit patients with rumination disorder. (25)
Chewing gum use is associated with fewer rumination episodes, but no randomized trials are demonstrating the effectiveness of this intervention. (44,45)
Conclusion
Rumination syndrome is a clinically recognized entity, with lots of clinical criteria included in the Rome IV criteria,(3) but often, patients with rumination syndrome go undetected and untreated. (24) Diagnosis can often be delayed because of a lack of clinician knowledge to assess for rumination syndrome, and patients can experience protracted symptoms without appropriate treatment. (24) Treatment is based on a detailed explanation of the condition to the patient and a solid doctor-patient relationship, encouraging adherence to diaphragmatic breathing exercises with or without biofeedback in referral centers, and using baclofen in second-line treatment. (3)
References...