Topic: Psychomotor Agitation
Author: Heba Mrouj
Editor: Ihda Mahmoud Bani Khalaf, Sadeen Eid.
Reviewer: Ethar Hazaimeh
Keywords: Psychomotor agitation, Agitated, Restlessness, DSM-5, Verbal de-escalation
Overview
Psychomotor agitation (PMA) is a clinical term used to describe a set of symptoms characterized by restlessness, excessive physical activity, irritability, and changes in cognitive functions. It is associated with various psychiatric and medical conditions and represents a crucial issue in psychiatry.[1]
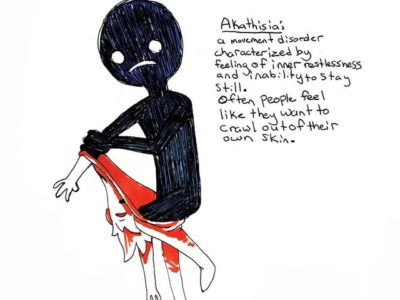
The latest version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines agitation as “an excessive motor activity associated with a feeling of inner tension”.[2]
PMA can manifest in several ways, such as restlessness or an inability to sit still; aimlessly darting around, pacing, incessant finger tapping, and sudden starts/stops in tasks. [6] They may also exhibit rapid speech, engage in purposeless object manipulation, and fidget with their clothing.
In severe cases, PMA may lead to self-inflicted harm, including actions like biting lips until they bleed, pulling at the skin around the nails, or chewing the inside of the cheek. [6] These symptoms often hinder an individual’s ability to focus, maintain calm, or engage in routine activities.
PMA is a complex and multifaceted clinical phenomenon, so understanding its underlying causes and early assessment is essential to improve the well-being and quality of life of individuals affected by this condition, ensure the safety of the healthcare staff, and ease future management. [2]
Epidemiology
While PMA carries significant clinical importance and is generally acknowledged as a prevalent phenomenon in medical practice, there is a lack of robust data concerning its epidemiology as an independent clinical entity. Most of the available information has been derived from patient encounters in psychiatric emergency settings, primarily addressing agitation in the context of psychiatric conditions, with a specific emphasis on aggressive and violent manifestations. [3]
The reported prevalence of agitation in psychiatric emergency services falls within the spectrum of 4% to 10%. [2]
PMA is notably widespread, especially among patients with schizophrenia and bipolar disorder (BD). [4] In a study conducted in Spain, it was found that about 25% of individuals diagnosed with schizophrenia and 15% of those with BD were estimated to encounter at least one episode of PMA annually, with an average of two episodes per patient each year. [4]
Causes and risk factors
Psychomotor Agitation is a multifactorial syndrome that is linked to numerous medical conditions, including:
- Psychiatric disorders (e.g. Bipolar disorder, schizophrenia, major depressive disorder, and anxiety disorder).
- Substance intoxication/withdrawal such as (Amphetamine/ cocaine abuse and alcohol/benzodiazepine withdrawal).
- General medical conditions like (Delirium, Neurodegenerative diseases, or even infections). Therefore, understanding the underlying cause of PMA is crucial for accurate diagnosis and effective treatment.
Moreover, certain risk factors found to be related to PMA can be classified into three main domains:[5]
- Demographic factors: such as being male, aged below 40, single, having a family history of alcoholism or aggressive tendencies as well as possessing a limited educational background, and belonging to a low socioeconomic stratum.
- Psychological factors: like recent exposure to highly stressful life events, or experiences of extended hospital admissions.
- Clinical factors: which encompass a family history of prior episodes involving agitation, anxiety, substance misuse, a lack of cooperation with treatment, limited self-awareness of one’s illness as well as Co-occurrence with conditions such as mental retardation, dementia, epilepsy, and personality disorders.
Sings and symptoms
Signs and symptoms of PMA can vary in intensity from mild to severe, which encompasses alterations in physical mobility, cognitive processes, and the functioning of the body. The table below outlines these signs/symptoms which can assist in identifying PMA:
Table 1: Signs and symptoms of psychomotor agitation [4]
| Type | Signs and Symptoms |
| Changes in behavior | • Combative attitude • Inappropriate behavior without a clear purpose • Hyperreactivity to stimuli • Inability to remain quiet, seated, or calm • Exaggerated gesticulation • Facial tension and angry expression • Defiant and/or prolonged visual contact • Raised tone of voice, silence, or refusal to communicate • Altered emotional state with the appearance of anxiety, irritability, or hostility • Verbal and/or physical aggression against self or others or objects |
| Cognitive changes | • Fluctuations in the levels of consciousness • Temporo-spatial disorientations • Tendency to frustration • Difficulty in anticipating consequences • Delusional ideas and/or hallucinations |
| Change in physical parameters | • Fever • Tachycardia • Tachypnoea • Sweating • Tremor • Neurological signs such as difficulty walking |
Diagnosis
The process of diagnosing PMA involves several crucial steps. First and foremost, ensuring the safety of the individual suspected of having PMA is paramount, as the condition can potentially lead to self-harm or suicidal tendencies.[7] Subsequently, a healthcare provider conducts a comprehensive assessment that includes a detailed patient interview and a physical examination. During the interview, the doctor can ask the patient questions about the onset of symptoms, exacerbating and alleviating factors as well as history of substance abuse. While during physical examination they can detect the signs of agitation. [6]
Various rating scales have been developed to aid in determining the presence of PMA. These scales involve observational assessments conducted over varying timeframes, ranging from minutes to hours or even days. [7] The checklists used in these scales typically focus on Identifying the symptoms that are currently present, assessing the intensity of these symptoms, as well as considering any additional symptoms that may not be directly related but might provide valuable clues in pinpointing an underlying cause. [2]
The rating scales utilized in diagnosing PMA include: [7]
- Agitation severity scale (ASS)
- Aggressive Behavior Scale (ABS)
- Agitated behavior scale
- Brief agitation measure (BAM)
- Brief agitation rating scale (BARS)
- Broset Violence Checklist (BVC)
- Clinical global impression scale for aggression (CGI-A)
- Cohen-Mansfield agitation inventory (CMAI)
- Historical, clinical, and risk management -20 violence risk assessment scheme (HCR-20)
- Neurobehavioral rating scale-revised (NRS-R)
- Overt agitation severity scale (OASS)
- Positive and negative syndrome scale-excited component (PANSS-EC)
- McNeil-Binder Violence Screening Checklist (VSC)
- Pittsburgh agitation scale (PAS)
- Ryden aggression scale
- State-trait anger expression inventory (STAXI)
- Staff Observation Scale (SOAS)
The process of diagnosing PMA is protracted because it can be linked to many different health disorders. Accurate diagnosis is crucial for proper treatment, as each underlying condition may require unique therapeutic approaches. While treatment can alleviate symptoms, the persistence and management of PMA may vary based on its cause, requiring ongoing and specific therapies. [7]
Management and Treatment
Depending on the severity of agitation episodes, they can progress unexpectedly, leading to aggressive behavior. This necessitates the implementation of non-coercive methods, which may begin with verbal de-escalation and/or oral medication, and in more advanced stages, it may require the application of more coercive or restraint measures. [8] Thus, the severity of PMA can determine the approach to treatment and management. [7]
The initial step for the management of PMA involves alleviating the individual’s anxiety and decreasing the risk of escalation into aggression or violence towards themselves or others. [6]
Treatment of PMA may involve:
-
Verbal De-escalation
Dealing with an agitated patient should commence by adjusting the environment and using verbal de-escalation techniques to offer physical comfort and reduce external stimuli. [2]
In every case of PMA, we should systematically use De-escalation techniques to prevent symptoms from getting worse, ultimately avoiding the need for physical restraint (which are methods that aim to immobilize the patient) [10]
Furthermore, De-escalation involves creating a safe environment as well as having a well-trained healthcare staff. It emphasizes the significance of respecting personal space, reassuring the patient, and maintaining non-provocative attitudes. Verbal contact is established with a designated person responsible for de-escalation. Active listening is encouraged to better understand the patient’s feelings, desires, and needs. [10]
-
Medication
Pharmacological approaches for addressing agitation have historically relied on three categories of medications: first-generation antipsychotics (FGAs), second-generation antipsychotics (SGAs), and benzodiazepines (BZDs). [9]
-
Identifying the underlying illness
Long-term treatment of PMA mainly depends on treating the underlying cause of symptoms, whether it is psychiatric, medical, or even substance abuse. These causes should be first treated to clear up the symptoms of agitation. [2,7]
Conclusion
Psychomotor agitation is a common condition linked to various psychiatric and medical disorders. It presents along a spectrum, ranging from mild agitation to the most intense and violent episodes. [3] Hence it is considered a serious health emergency, treated as a severe mental disorder. [5] It necessitates immediate professional care and neglecting it may significantly compromise the safety of the patient. [5]
Furthermore, inadequate treatment of PMA may result in rapid progress to its most severe level. So, it is crucial to initiate treatment at the earliest opportunity and pinpoint patients in the early stages of their condition. [3]