Article topic: Non-Atherosclerotic Carotid Artery Lesions
Name of the author: Rand Al Kalbani
Key words: non-atherosclerotic, carotid lesion, dissection, fibromuscular dysplasia, carotid artery aneurysm
Scientific editor: Dr.Omar Jbara
Linguistic editor: Philip Sweidan
Overview
Non atherosclerotic carotid lesions are uncommon disorder that is more seen in young aged group, it includes various pathology such as fibromuscular dysplasia, spontaneous carotid artery dissection, extracranial carotid artery aneurysm and radiation stenosis. Recently the incidence started to increase due to better imaging methods including magnetic resonance angiography and computed tomography angiography. The aim of management whether medially, surgically or endovascular is to preserve efficacy and to decrease the morbidity and mortality rate.1
SPONTANEOUS CAROTID ARTERY DISSECTION
Etiology and pathogenesis
It is rare but life threatening condition, it accounts for 2% of total ischemic strokes, mainly in the age between 35 and 50 years old with no significant difference in gender. In general it is either caused by neck trauma or spontaneously associated with fibromuscular dysplasia , Marfan’s syndrome, cystic medial necrosis, or Ehlers-Danlos syndrome2, following a violent uncontrolled cough, exercise, or aggressive sudden movement of the head. Dissection arises from the tunica intima (the inner layer of the artery) allowing the blood to enter the wall of the artery under the influence of the arterial pressure, forming an intramural hematoma either toward the intima (inward) or toward the adventitia (outward) making a pseudo-aneurysm (1,2)
The etiology depends on environmental and genetic factors; some studies say that it is manifested with collagen type III deficiency. Other studies show that elevation in homocysteine increases the incidence of dissection. Also increase in level of proteases mainly matrix metalloproteinase 2 have shown some evidence of dissection. Some vasodilators abnormalities such as impairment in nitroglycerin may predispose the risk for dissection. Also it is found that respiratory tract infections are implicated as a trigger(3)
Clinical presentation and complications
The presence of two symptoms from the classical triad is enough to diagnose spontaneous carotid dissection, including ipsilateral pain in the face, head, and neck, transient ischemic attack or partial Horner’s syndrome. 83%of the patients also complain from headache in the frontal or periorbital, or even periauricular region. This pattern is due to the anatomical distribution of the sympathetic fibers of the carotid artery. The internal carotid artery travels with the sympathetic fibers of the eye, and the external carotid artery travels with the sympathetic fibers of the sweat glands of the face. Surprisingly neck pain was only found in 21% of the patients, however transient ischemic attack was found in 60% and Horner’s in 50%(1)
Doctors should asses for carotid bruits because they are found in 40% of the patients. An important follow through test is oculopneumoplethysmograhpy, accessing the retinal artery pressure.(1)
Workup and diagnosis
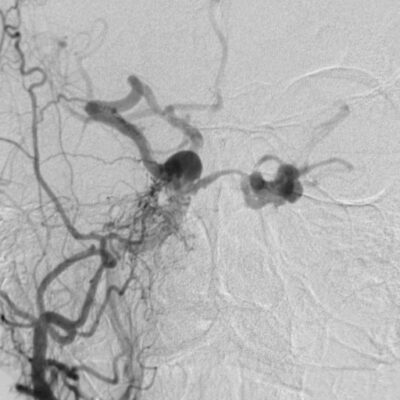
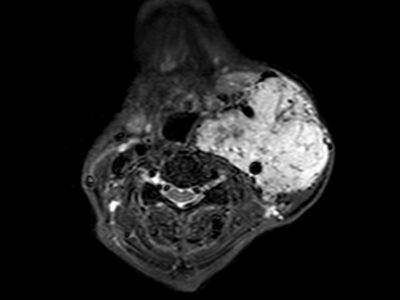
Carotid dissection is seen as a string sign on digital angiography, which is the gold standard image as shown in figure1. Usually with irregular stenosis, starting after 2 to 3 cm distal to the carotid bulb and extending but not further from the beginning of the petrous portion of the artery. In less than 10% of the cases we can find double lumen or intimal flap. These radiographical findings may worsen especially in the acute phase within a period of days or even hours.
The long term re-canalization in patients who had complete occlusion and was treated with anticoagulation is around 47%. Other noninvasive modalities such as magnetic resonance angiography or computed tomography angiography are used as screening methods.

FIGURE 1 : Digital angiography string sign of carotid dissection Case courtesy of Assoc Prof Frank Gaillard4
Treatment
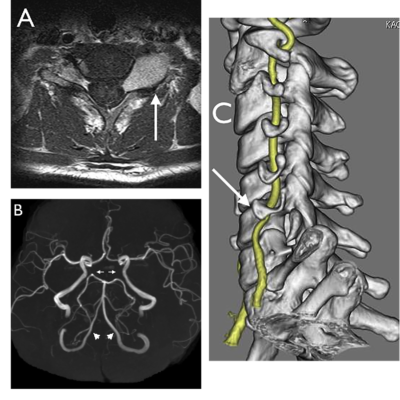
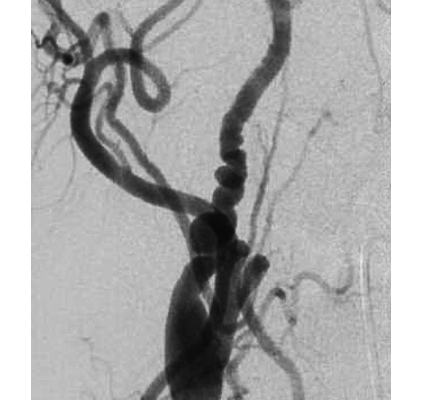
Antithrombotic therapy whether antiplatelet or anticoagulants are the mainstay for the management of carotid dissection. Angioplasty and stenting may be indicated for ischemic symptoms as shown in figure 2.
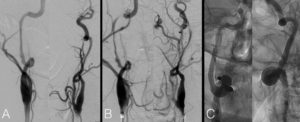
Figure 2 :right internal carotid artery digital angiography A) long cervical dissection with 360° loop B) worsened stenosis at the horizontal petrous segment with string sign C) the artery after reconstruction with 3 stents 5
In very rare severe cases, direct surgical repair is an option with patch graft or interposition graft, carotid ligation with or without artery bypass, a superficial temporal artery to middle cerebral artery bypass, or a high-low saphenous vein graft bypass, depending on the need for cerebral blood flow.1
Prognosis
The prognosis depends on the severity of the ischemic insult and the extension of the collateral circulation. The morbidity rate is less than 5%. In the first two to three months headache will resolve, 90% of the stenosis will resolve, aneurysms will decrease in size and occlusions will be re-canalized. The risk of recurrent dissection in the first month is 2% then decreases about 1% per year.2
In rare cases, persistent aneurysms may cause thromboembolic complications years after but they never rupture.2
EXTRACRANIAL CAROTID ARTERY ANEURYSMS
Etiology and pathogenesis
It is a rare condition with incidence less than 1% of total aneurysms, but it is significantly important due to the complications of having neurological thromboembolic events, cranial nerve compressions, or even aneurysm rupture. It is either caused by a trauma such as previous carotid surgery leading to a pseudo-aneurysms, atherosclerosis, fibromuscular dysplasia, or congenital. The most common location is at the bifurcation of the carotid artery followed by middle to distal internal carotid artery.6The prevalence of stroke in non-treated patients is 50% and mortality rate around 70% .7
Clinical presentation and complications
The patient’s presentation varies according to the size and the site of the aneurysm. Large aneurysms present as a pulsatile tender or non-tender mass. Symptomatic patients usually present with neck hematoma or epistaxis, other patients may present with transient ischemic attack due to thromboembolic events caused by the turbulent blood flow.
Workup and diagnosis
It is very essential to diagnose unruptured extracranial carotid artery aneurysm. Ultrasound is the first preferred test to a suspected aneurysm, followed by magnetic resonance angiography for further evaluation to determine the size, shape and location.8
Treatment
The management depends on the site, size, shape and cause of the aneurysm. Resection of the aneurysm in an open surgery and grafting is now replaced by endovascular stent grafting due to better outcomes, higher success rate and less morbidity and mortality rate.1
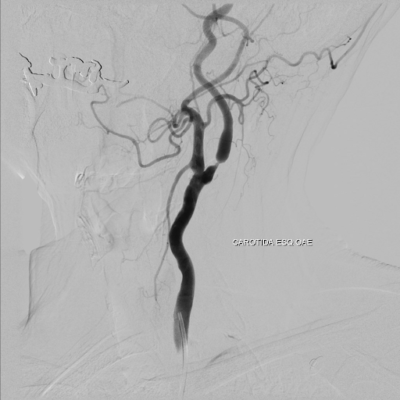
If the aneurysm is in the low to mid cervical region, or even fusiform aneurysms, it can be excised directly and then re-anastomosis of the proximal and distal artery as shown in Figure 4. If the primary re-anastomosis is not suitable, a Dacron or saphenous vein graft can be used to reconstruct the carotid artery. During the procedure, temporarily clipping of the carotid artery is done with electroencephalogram monitoring. 1
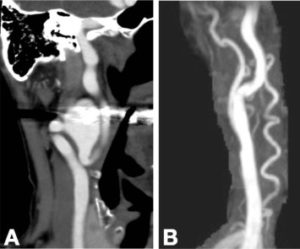
Figure 4 : CTA of the right external carotid artery aneurysm A)before surgery B) after resection and reanastomosis of the artery 10
Direct approach can’t be done if the aneurysm is in the high cervical region; instead high flow vein bypass is done. Moreover, aneurysms in that area can be caused by Para-pharyngeal infection, so it’s highly infectious and stenting in that area can cause chronic implant infection. That’s why a carotid occlusion is done to these patients if he passes a balloon test occlusion, if he fails, bypass occlusion with carotid occlusion is the preferred choice. If there is no infection, an endoluminal stent is done1.
FIBROMUSCULAR DYSPLASIA
Etiology and pathogenesis
It is a unifocal or multifocal, idiopathic, nonatherosclerotic, noninflammatory vascular disease that affects medium to large vessels mainly renal and internal carotid arteries. It is predominantly found in women with a ratio of 9:1, and any age group but mainly from 20 to 60 years old.1
Histologically fibromuscular dysplasia presents with three primary pathologies, intimal fibroplasia, medial fibroplasias, and sub-adventitial hyperplasia. Medial fibroplasias is limited to the outer media to the involvement of the entire media.1
The milder form of the disease is characterized by accumulation of collagen and ground substances separating in the disorganized smooth muscle cell, however, in the severe form, the media itself is profoundly disorganized with fibroblast and collagen replacing the smooth muscle1
The etiology of fibromuscular dysplasia is unknown, although various hormonal (progesterone and estrogen) and mechanical factors have been suggested.
Clinical presentation and complications
The majority of cases are asymptomatic, patients could also complain from headache, tinnitus, vertigo, lightheadedness and syncope. 2/3 of the patients have carotid bruit, and 18% to 56% have cerebrovascular symptoms due to stenosis or occlusion in the carotid arteries.1
Fibromuscular dysplasia can cause hypertension (renal artery fibromuscular dysplasia), spontaneous carotid artery dissection, aneurysm formation, carotid cavernous fistula, thromboembolism, subarachnoid hemorrhage, stroke or even mesenteric ischemia.(11,1)
Workup and diagnosis
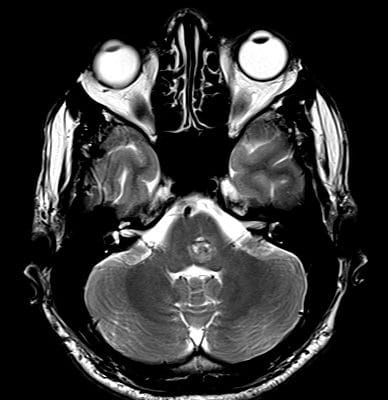
Fibromuscular dysplasia is usually found incidentally when angiography is done for other reasons. In 80% of patients, the string of beads is found on angiography. A multiple irregular spaced constriction with normal or ectatic intervening segments1 as shown in Figure 5
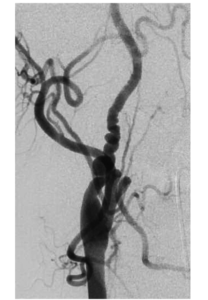
Figure 5: carotid angiogram showing the string of beads in FMD 1
The second presentation is smooth, concentric tubular stenosis. Other presentation called atypical fibromuscular dysplasia, involving one wall of the affected segment, creating smooth out pouching of the artery.1
Duplex ultrasound of the carotid arteries is less sensitive technique, it may demonstrate irregular pattern of stenosis. 1
Treatment
Management depends on the patient’s presentation. Medical or surgical treatment should be reserved for patients who have symptoms of cerebral ischemia. Antiplatelet, antithrombotic and antihypertensive drugs are the main treatment for carotid fibromuscular dysplasia. Vascular intervention is rarely performed since it is non athereosclerotic.12
RADIATION STENOSIS
Etiology and pathogenesis
Radiation is abundantly used to treat many vascular pathologies, such as arteriovenous malformation, arteriovenous fistulas, cavernous malformations, and vascular tumors. On the other hand, radiation to the normal vessel can induce variable side effects depending on the arterial size and radiation dose. It was observed that damaged endothelial cells by radiation do not function well as a barrier to plasma lipoprotein infiltration in the vessel wall. As a result, we will have lysosomal activation and cellular proliferation within the vessel wall, resulting in intimal plaque formation. With the continuous radiation in the treatment of neck and mediastinal malignancies, reports of radiation induced extracranial carotid stenosis became more prevalent. External carotid stenosis from radiation is more challenging due to the involvement of extensive segments of the carotid artery and because it is associated with fibrosis of the arterial wall and the normal tissue, which makes endarterectomy more difficult.1
Clinical evaluation
Imaging studies are done for patients who developed symptoms of cerebral ischemia or emboli after radiation to the head, neck, or mediastinum. Although radiation changes in large arteries look very similar to the atherosclerotic changes seen in the carotid bulb, the spectrum of radiation stenosis is more variable. For example, the arterial changes associated with radiation stenosis can occur in places that can’t be affected by atherosclerosis. Moreover, radiation stenosis can severely affect the surrounding tissue. Lastly, the damaged carotid arterial wall can make sever and more dangerous cardiac endarterectomy than the usual one. A carotid duplex scan gives information about most of the cervical carotid artery, but not a good choice for the evaluation of the proximal cervical carotid artery and the distal cervical internal carotid artery. For a complete view of the arterial origins of high cervical segments, magnetic resonance angiography is done but may not be obtainable in some patients. So cervical and cerebral angiography remains the “gold standard” for radiation stenosis.1
Treatment
As said before dissection of plaques caused by radiation stenosis is more difficult because of the adherence to the intima. So as a primary treatment for radiation stenosis is carotid angioplasty stenting. It is used due to association of stenosis with soft tissue fibrosis, operating through an area of a previous myocutaneous flap, and more proximal arterial involvement.1
External links: