Title of article: Narcolepsy
Author: Manar Al-Titi
Editors: Lubna Al-Rawabdeh, Samah Al-Ajjawe
Reviewer: Ethar Hazaimeh
Keywords: Multiple Sleep Latency Test (MSLT), Polysomnography (PSG), Sleep Onset REM Periods (SOREMPs)
Introduction
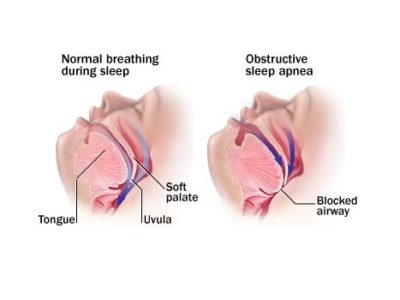
Narcolepsy is a chronic neurological disorder characterized by excessive and overwhelming drowsiness, cataplexy (episodes of muscle weakness at times of intense emotion), hypnagogic hallucinations (vivid dreams at the onset of sleep), and sleep paralysis (temporary inability to move the body as a unit). before falling asleep or upon waking). This is one of the most common reasons for preventing daytime sleepiness after obstructive sleep apnea. [1,2]
Narcolepsy occurs in two forms in both children and adults, depending on whether cataplexy is present [3]. Type 1 narcolepsy, formerly known as narcolepsy with cataplexy, includes cataplexy as one of the first symptoms and is associated with low levels of orexin (also called hypocretin) in the cerebrospinal fluid (CSF). Narcolepsy type 2, or narcolepsy without cataplexy, has all the features of narcolepsy type 1 except cataplexy and low CSF orexin levels.
Epidemiology
Type 1 narcolepsy (narcolepsy with cataplexy) is estimated to have a prevalence of 27 to 50 per 100,000 people and an incidence of 0.75 per 100,000 person-years [4-5]. It is equally common in men and women [6-7]. Narcolepsy usually begins in the teens and early 20s but occasionally occurs as early as the age of five or after 40 years of age. The prevalence of type 2 narcolepsy (narcolepsy without cataplexy) is undetermined because it is understudied and more difficult to diagnose, but it has been estimated at 21 to 36 per 100,000 people.
Etiologies
Loss of orexin (hypocretin) signaling, genetic factors, and, more rarely, brain lesions can cause narcolepsy.
Orexin/Hypocretin: Narcolepsy results from the loss of the neuropeptides orexin-A and orexin-B (also known as hypocretin-1 and hypocretin-2) [8,9]. These neurotransmitters are products of the pre-pro-orexin gene and are produced by neurons in the lateral hypothalamus [10,11]. Orexins A and B have excitatory effects when bound to OX1 and OX2 receptors on postsynaptic neurons.
Orexins are released during wakefulness and increase the activity of many brain regions involved in promoting wakefulness, including the locus coeruleus, raphe nuclei, and tubercle mammillary nucleus [12]. By increasing the activity of these wakefulness-promoting monoaminergic neurons, orexins stabilize wakefulness, prevent inappropriate transitions to rapid eye movement (REM) or non-REM sleep, and inhibit REM sleep. The loss of orexins also allows REM-related phenomena (eg, cataplexy, hypnagogic hallucinations, and sleep paralysis) to invade the waking state.
Animal models first identified the importance of orexins in narcolepsy. Dogs with OX2 receptor mutations were found to exhibit drowsiness and cataplexy very similar to human narcolepsy [13]. Mice lacking orexin peptides or orexin-producing neurons also had severe narcolepsy [14]. Very similar behavior was observed in mice lacking both orexin receptors.
People with narcolepsy are usually classified as having either type 1 narcolepsy (narcolepsy with cataplexy) or type 2 narcolepsy (narcolepsy without cataplexy). It was later shown that people with type 1 narcolepsy are also deficient in orexin. individuals with type 1 narcolepsy had an approximately 91% decrease in the number of hypothalamic orexin-producing neurons with little or no detectable orexin-A in their cerebrospinal fluid [15-17]. The neuronal loss appears to be selective because adjacent neurons containing the melanin-concentrating hormone are conserved.
In the brains of patients with type 1 narcolepsy, an increase in the number of
histamine-producing neurons and a decrease in the number of corticotropin-releasing hormone-producing neurons have been observed [18-19]. These are most likely compensatory responses to the loss of excitatory stimuli from orexin neurons, and their physiological significance remains unclear.
The cause of narcolepsy type two is unknown, and these sufferers generally have normal cerebrospinal fluid (CSF) orexin-A levels. It has been hypothesized that this disorder may result from much less widespread loss of the orexin neurons [20], impaired orexin receptor signaling, or a totally separate mechanism. About 24 percent of sufferers who have narcolepsy type 2 have low CSF orexin-A levels, and about 1/2 of these people can also later strengthen cataplexy, suggesting the progression of the disorder [21].
Genetic factors — Narcolepsy generally happens sporadically, but genetic factors play an important role. The DQB1*0602 haplotype (a subtype of DQ1) is present in 94 percent of sufferers with cataplexy and in 95 percent of those with orexin deficiency [22]. Some additional human leukocyte antigen (HLA) haplotypes may further expand the hazard of narcolepsy, whilst others show up protecting. [23]. Though these and other genetic factors may predispose some humans to boost narcolepsy, environmental factors appear to be extra important, as only about 25 percent of affected monozygotic twins are concordant for narcolepsy [24].
Autoimmune speculation — Researchers hypothesize that the orexin neurons are selectively killed by an autoimmune process, since narcolepsy is strongly associated with a certain HLA haplotype, DQB1*0602 [25]. The onset of narcolepsy appears best in the spring, suggesting that it may also be brought on with the aid of a wintry weather infection [26]. One viable set is streptococcal pharyngitis because anti-streptolysin O (ASO) and anti-DNase B titers are time to time elevated, especially in the first year after the onset of narcolepsy [27].
A T cell-mediated process is feasible due to the fact narcolepsy is linked to a polymorphism in the T cell receptor alpha gene [28]. Supporting this idea, quite a few research have shown that patients with narcolepsy regularly have T cells that target a couple of epitopes of the pre-pro-orexin protein [29]. A humoral mechanism may additionally also contribute, as antibodies against tribbles homolog 2, a protein expressed in neurons, is expanded in some patients quickly after the onset of narcolepsy. The number of astrocytes might also be relatively expanded in the orexin neuron region, which is regular with an inflammatory or neurodegenerative process.
Individuals in countless countries in Europe developed narcolepsy type 1 quickly after receiving Pandemrix, an AS03-adjuvanted 2009 H1N1 influenza vaccine. Pandemrix used to be used in some European countries during the course of the 2009-2010 H1N1 influenza pandemic, but it used to be no longer used in the United States. One proposed mechanism is cross-reactivity between the human orexin two receptor and influenza nucleoprotein A, a protein found in higher concentrations in Pandemrix compared with different H1N1 vaccines.
It appears probable that the orexin neurons are killed by using an autoimmune mechanism, however, the method has to be accurate. Neuroimaging studies have discovered no consistent abnormalities [30], and CSF of sufferers shut to narcolepsy onset lacks improved protein or oligoclonal bands [31-32].
Secondary narcolepsy — In rare cases, posterior hypothalamus and midbrain lesions can cause narcolepsy. Tumors, vascular malformations, strokes, and inflammatory approaches such as neurosarcoidosis have all been suggested to cause secondary narcolepsy, most likely due to direct damage to the orexin neurons or their projections [33]. Narcolepsy can additionally appear with genetic syndromes such as Prader-Willi syndrome or Niemann-Pick disease type C, and sleepiness and cataplexy-like activities are seen in some patients with Prader-Willi syndrome [34].
DSM-5 Diagnostic Criteria
A. Recurrent durations of an irrepressible need to sleep, lapsing into sleep or napping going on within the same day. These need to have been going on at least three times per week over the previous 3 months.
B. The presence of at least one of the following:
- Episodes of cataplexy, described as either (a) or (b), going on at least a few times per month:
a. In humans with long-standing disease, quick (seconds to minutes) episodes of sudden bilateral loss of muscle tone with maintained attention are precipitated through laughter or joking.
b. In children or in persons within 6 months of onset, spontaneous grimaces or jaw-opening episodes with tongue thrusting or global hypotonia, besides any obvious emotional triggers.
2. Hypocretin deficiency as measured by cerebrospinal fluid (CSF) hypocretin-1 immunoreactivity values (less than or equal to one-third of the values determined in healthy subjects tested with the same assay, or less than or equal to one). hundred percent hundred). ten pg/ml). Low CSF hypocretin-1 levels should not be observed in the context of acute brain injury, inflammation, or infection.
3. Nocturnal sleep polysomnography displaying fast eye movement (REM) sleep latency less than or equal to 15 minutes, or a multiple sleep latency check to display an implied sleep latency less than or equal to 8 minutes and two or extra sleep-onset REM periods.
Specify whether:
G47.411 Narcolepsy with cataplexy or hypocretin deficiency (type 1): Criterion B1 (episodes of cataplexy) or Criterion B2 (low CSF hypocretin-1 levels) is met.
G47.419 Narcolepsy besides cataplexy and either except hypocretin deficiency or hypocretin unmeasured (type 2): Criterion B3 (positive polysomnography/multiple sleep latency test) is met, however, Criterion B1 is now not met (i.e., no cataplexy is present) and Criterion B2 is now not met (i.e., CSF hypocretin-1 stages are not low or have now not been measured).
G47.421 Narcolepsy with cataplexy or hypocretin deficiency due to a clinical condition.
G47.429 Narcolepsy without cataplexy and besides hypocretin deficiency due to a medical situation Coding note: For the subtype narcolepsy with cataplexy or hypocretin deficiency due to a clinical circumstance and the subtype narcolepsy besides cataplexy and barring hypocretin deficiency due to a scientific condition, code first the underlying clinical situation (e.g., G71.11 myotonic dystrophy; G47.429 narcolepsy barring cataplexy and besides hypocretin deficiency due to myotonic dystrophy).
Specify present-day severity:
Mild: Need for naps solely once or twice per day. Sleep disturbances, if present, are mild. Cataplexy, if present, is rare (occurs less than once a week).
Moderate: Need for more than one nap daily. Sleep may additionally be moderately disturbed. Cataplexy, when present, occurs daily or every few days.
Severe: Nearly regular sleepiness and, often, fantastically disturbed nocturnal sleep (which may additionally include immoderate body motion and vivid dreams). Cataplexy, when present, is drug-resistant, with a couple of attacks daily.
Diagnosis
All sufferers with chronic daylight hours sleepiness have to have a thorough history, sleep history, physical exam, and neurologic examination searching for proof of cataplexy, hypnagogic or hypnopompic hallucinations, or sleep paralysis. Questions that are useful in detecting viable narcolepsy consist of the following:
- Are you sleepy most of the day?
- Do you feel rested on waking in the morning?
- Are your naps refreshing?
- Do you ever see, feel, or hear things that you know aren’t there as you are falling asleep?
- Are you ever unable to move when you first awake or as you are falling asleep?
- Do you have muscle weakness when you laugh or tell a joke?
- Over the last two weeks, how often have you fallen asleep when you did not intend to?
| Question | Implication |
| Are you sleepy most of the day? | Sleepiness is present but could be caused by a variety of conditions |
| Do you feel rested upon waking in the morning? Are your naps refreshing? | Sleepiness is probably not caused by poor quality sleep (eg, sleep apnea, etc) |
| Do you have vivid dreams during daytime naps? | Possible REM sleep during naps |
| Do you ever have muscle weakness when you tell a joke or laugh? | Cataplexy |
| Do you ever see, hear, or feel things that you know aren’t there as you are falling asleep? | Hypnagogic hallucinations |
| Are you ever unable to move when you first awake or just before falling asleep? | Sleep paralysis |
| Over the last two weeks, how often have you fallen asleep when you did not intend to? | Functional impact of daytime sleepiness; complements the Epworth Sleepiness Score |
If the answer to any of these questions is yes, then narcolepsy should be considered and each should have a polysomnogram and more than one sleep latency test performed.
Sleep research — The purpose of the polysomnogram is to exclude alternative and coexisting causes of persistent daytime sleepiness, which might also warrant specific therapy [35]. The motive behind more than one sleep latency take a look at multiple sleep latency test (MSLT) is to measure the mean sleep latency and pick out sleep onset speedy eye motion periods (SOREMPs). Stimulants and other psychoactive medications ought to be stopped one week earlier than testing, and antidepressants have to be stopped at least three weeks earlier than trying out (four weeks for fluoxetine) to keep away from speedy eye motion (REM) sleep rebound effects. The patient should additionally have actigraphy or an entire sleep log for one to two weeks prior to the MSLT to document adequate quantities and timing of sleep.
Polysomnography (PSG) evaluates sleep architecture, sleep quality, and different physiological parameters. Patients who have narcolepsy commonly reveal spontaneous awakenings, mildly decreased sleep efficiency, and increased light non-REM sleep. Patients with narcolepsy kind 1 and occasionally those with narcolepsy type two may show REM sleep within 15 minutes of the onset of sleep [36]. In contrast, wholesome individuals enter REM sleep 80 to hundred minutes after the onset of sleep. Polysomnographic characteristics of alternative issues are described separately.
The MSLT starts in the morning, 1.5 to 3 hours after the PSG. The patient is placed in sleep-inducing surroundings (ie, dark, quiet room) and prompted to try to sleep. Monitoring includes electroencephalography (EEG), electrooculography, intellectual or submental electromyography, and electrocardiography (ECG). Each nap session continues for 15 minutes after sleep onset to realize REM sleep. The sleep latency is documented for every nap session. If the patient no longer falls asleep, the nap session is terminated after 20 minutes and the sleep latency is documented as being 20 minutes. This is repeated at two-hour intervals till the patient has had four or 5 possibilities to nap [37].
On average, wholesome subjects fall asleep in about 10 to 15 minutes, whereas human beings with narcolepsy fall asleep in much less than 8 minutes, offering objective proof of their sleep propensity [38]. The naps of sufferers with narcolepsy often include REM sleep, and the presence of two or greater naps containing REM sleep (known as SOREMPs) is a crucial characteristic of narcolepsy [39-40].
The MSLT has a number of barriers in the diagnostic evaluation of narcolepsy that must be considered:
- An MSLT is valid only if the PSG validated at least six hours of sleep at some stage in the preceding night. Greater quantities of sleep may additionally be wished to be considered adequate in youth and adults with longer sleep times.
- The MSLT has terrible test-retest reliability and can be falsely poor or nice 20 to 30 percent of the time, especially in narcolepsy sufferers who lack cataplexy. For poor studies, the test needs to be repeated if the records are strongly suggestive of narcolepsy.
- The MSLT may additionally be less sensitive for the prognosis of narcolepsy in older adults because sleep latency increases and SOREMPs grow to be less universal with age.
- More than two SOREMPs are not specific for analysis of narcolepsy. SOREMPs are common in shift workers and can show up with other disorders that extend REM sleep pressure, such as inadequate sleep, untreated sleep apnea, or circadian phase delay. In fact, 5-10% of the typical population may even have two or more SOREMPs and up to 20% have a recommended sleep onset latency of ≤ 8 minutes. SOREMPs that immediately comply with stage N1 sleep may be extra unique for narcolepsy than those that follow stage N2 or N3 sleep [41].
- REM sleep-suppressing medicines (eg, antidepressants, stimulants) can forestall the appearance of SOREMPs, and withdrawal from these capsules can produce SOREMPs, for up to a number of weeks after discontinuation.
Other laboratory assessments — Measurement of orexin-A (hypocretin-1) in cerebrospinal fluid (CSF) is useful in sure medical conditions [42]. Examples include when the multiple sleep latency check is hard to interpret due to both bad midnight sleep (eg, insomnia, sleep apnea, circadian rhythm sleep disorders); the incapacity to discontinue antidepressants or other sleep-modulating medications prior to testing; when the affected person is a young child (the MSLT has no longer been standardized in younger young people and, thus, is difficult to interpret or when the patient has ordinary cataplexy (90 percent of sufferers with real cataplexy have low orexin levels). A commercially reachable assay for CSF orexin-A is handy in the United States via Mayo Clinic Laboratories.
HLA checking out is now not hobbies for diagnosing narcolepsy. Most humans with narcolepsy are DQB1*0602 positive, however, this discovery is now not specific because this haplotype additionally occurs in 12 to 40 percent of healthful Americans, and more than 98 percent of DQB1*0602 superb folks do not have narcolepsy. Still, some clinicians discover HLA trying out beneficial in people with cataplexy, as over 89 percent of patients with narcolepsy with cataplexy elevate DQB1*0602 [43]. Conversely, in patients with extraordinary cataplexy, lack of DQB1*0602 affords help in opposition to a prognosis of narcolepsy with cataplexy.
Differential Diagnosis
When narcolepsy is suspected, various surrogate conditions must be considered, especially when cataplexy is no longer present. The correct differential analysis depends on which symptom or sign gave rise to suspicion of narcolepsy:
- Chronic daytime sleepiness: Many conditions can cause daytime sleepiness by interfering with sleep duration or quality. These include inadequate sleep, obstructive sleep apnea, central sleep apnea, periodic limb movements, sleep and waking rhythm disorders (eg, rotating shift work), mood disorders, and hypersomnia. It is common for more than one of these circumstances to exist.
Sleep recording and actigraphy are useful when the circadian disease is suspected or to provide evidence of chronic sleep deprivation. In patients with delayed sleep phase disorder, a two-time sleep latency test (MSLT) can show multiple numbers of sleep-onset REM periods (SOREMPs) even after five hours of sleep the night before, when normal sleep duration extends to the end of the night. late tomorrow. Similarly, uncorrected sleep deprivation may result in an expanded variety of SOREMPs in -MSLT that are now not unique to a diagnosis of narcolepsy.
- Cataplexy: sudden muscle weakness that occurs while a person is awake. Intense Thoughts Trigger Cataplexy [44] The cause of cataplexy is still under investigation, most people with cataplexy have a loss of certain brain cells that produce the hormone orexin (also called hypocretin). Orexin plays an essential role in the sleep-wake cycle.
Much of what we know about the relationship between cataplexy and orexin (hypocretin) comes from research on narcolepsy type 1. This research suggests that a number of factors may also play a role in orexin loss in people with narcolepsy type 1.
- Hypnagogic hallucinations and sleep paralysis: These symptoms are common in narcolepsy but can also occur as isolated phenomena, often triggered by inadequate sleep, obstructive sleep apnea, circadian rhythm sleep disorders, and anxiety. They can also occur as a rebound phenomenon in patients who stop taking substances that suppress REM sleep (e.g. alcohol, amphetamines, antidepressants) [45,46]. About 21 percent of healthy people may experience infrequent hypnagogic hallucinations or sleep paralysis (eg, 2 or 3 times a year), but many people with narcolepsy experience these symptoms more frequently (eg, 3 or 4 times a month). In contrast to the hallucinations of schizophrenia and other psychotic disorders, patients with narcolepsy often distinguish hypnagogic hallucinations as dream phenomena.
Treatment
Narcolepsy has no cure, but medication and lifestyle adjustments can help manage symptoms.
Drugs for narcolepsy include:
- sodium oxybate (Xyrem) and oxybate salts (Xywav). These drugs work well to relieve cataplexy. They help improve nighttime sleep, which is often poor in narcolepsy.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs) or selective serotonin reuptake inhibitors (SSRIs).
- Tricyclic antidepressants. These ancient antidepressants can treat cataplexy. But they can cause side effects like dry mouth and dizziness.
Researchers are studying possible unique treatments for narcolepsy. Drugs under study include those that target hypocretin chemistry. Researchers are also studying immunotherapy. More research is needed before these pills are available.