Article topic: Ischemic Stroke
Author: Zain Sarhan Alsaddi
Keywords: Ischemic Stroke, Neurology, Neuromedicine, Cerebrovascular Diseases
OVERVIEW
A stroke results from a sudden cessation of sufficient blood supply to the brain. The disruption of blood supply is either due to a blockage of a main cerebral artery or a rupture in one causing it to bleed. This subsequently deprives the brain tissue of oxygen and nutrients and eventually leads to cell death within few minutes. 1
There are three main types of stroke. The most common type is the Ischemic stroke, which accounts for 87% of all strokes. It is the consequence of an occluded cerebral artery that clogged up by either a thrombus or an embolism. The second, less common yet more severe type is the hemorrhagic stroke, and this happens as a leaking or burst of a blood vessel. It is further subdivided into types which are intracerebral hemorrhage as well as subarachnoid hemorrhage. 7
The third type, sometimes called a “mini stroke”, or what is more commonly known as the transient ischemic attack (TIA), the definition of a TIA has changed from time-based to tissue-based. It is defined as a transient episode of neurologic dysfunction due to the focal brain, spinal cord or retinal ischemia without acute infarction. A TIA is a temporary disruption of blood flow that typically lasts a few minutes and does not cause lasting symptoms. It is important to know that a TIA is a warning sign of a future stroke and just like the other two major types of stroke, it requires emergency care. 8
Stroke is considered the third leading cause of death in the world and tends to lead to a long-term disability and cognitive impairment. Immediate or delayed vascular cognitive impairment (VCI) or vascular dementia (VaD) was detected in about 25–30% of ischemic stroke survivors. 1, 9
PATHOGENESIS AND ETIOLOGY
The exact mechanism for stroke injury is not fully understood despite considerable research efforts. However, it is established that cerebral ischemia induces a cascade of inflammatory and immune reactions that encircle molecular, cellular as well as genomic events. Furthermore, the body’s Immune response has been shown to play a major role in ischemic stroke progression. Neuronal damage’s extent seems to correlate with the degree of innate immune activity.
After the ischemic stroke event occurrence, Pathophysiological changes take place like ionic imbalance, neuro-inflammation, excitotoxicity, and activation of microglia which contribute to neuronal death. Moreover, Ischemia induces a significant increase in microvascular density, a sign of angiogenesis and its degree is positively correlated with the survival rate of stroke patients. In addition to that, an improvement in functional outcome after ischemic stroke was found to be associated with increased angiogenesis. However, in a clinical setting, neither neuroprotection nor angiogenesis strategies showed any therapeutic benefit.
Marcet et al. discussed the impacts of inflammation in ischemic stroke and traumatic brain injury indicating that although the initial trauma that led to brain damage is most likely unsalvageable, the secondary immunologic deterioration of neural tissue gives many opportunities for therapeutic strategists. 9, 10
RISK FACTORS
The risk factors for ischemic stroke greatly mirror the risk factors of atherosclerosis and primary prevention of stroke focuses on the identification and modification of risk factors. They are divided into non-modifiable and modifiable risk factors. 2, 11, 12
Non-modifiable risk factors
- Age: In general, stroke is known to be a disease of aging. Its incidence increases as the person grows older, with the incidence doubling after age 55 for each decade. 34
- Gender: The relationship of sex to stroke risk mainly depends on age. Previously the risk of stroke was thought to be higher in men, however recent studies and research suggest otherwise indicating that, at younger ages, women have a higher risk of stroke and this is related to pregnancy and the postpartum state that follows it as well as hormonal factors like the use of contraception. Furthermore, it is believed to be higher in women due to their longer lifespan when compared to men. 34 A study that was performed in 8 different European countries discovered that the risk of stroke increased in men and women yearly by 9% and 10% respectively. 35
- Race: when compared to their white counterparts, African Americans showed that they are at twice the risk of stroke incidence, and also have a higher mortality associated with stroke.36
- Family history
- Genetic risk factors33 :
-
- Single gene disorders that primarily cause stroke
- Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CADASIL)
- Cerebral Autosomal Recessive Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CARASIL)
- Familial amyloid angiopathy
- Collagen 4 (COL4A1) mutations
- Ehlers-Danlos Type 4
- Fabry Disease
- Marfan syndrome
- Mitochondrial encephalopathy with lactic acid and stroke- like episodes (MELAS)
- Sickle cell disease
- Smooth Muscle Alpha-Actin (ACTA2) mutation associated disorders
Modifiable risk factors
- Hypertension: It is considered to be the most important modifiable risk factor for stroke. With the increasing age, the risk of developing hypertension also increases regardless of the hypertension status. Alongside medical hypertension control, the hypertensive patients are also encouraged to engage in lifestyle behavioral modifications, such as dieting and increase physical activity. These two methods of hypertension remain the most effective strategies in reducing stroke risk. 37
- Diabetes mellitus is an independent risk factor that increases the risk for stroke by 2 folds. 38
- Dyslipidemia: Stroke incidence also increases with an increase in total cholesterol level and low LDL. It causes thick and hard plaque to build up in your arteries and thus clog them. Subsequently reducing the flow of blood and leading to an infarct.
- Cardiovascular issues like Atrial fibrillation (AF) for the longest, the relation between AF and stroke has been initially assumed to be due to blood stasis in the fibrillating left atrium that causes a thrombus to form and embolize to the brain. however recent data challenged this assumption stating that, First, around one-third of patients do not show evidence of AF until after a stroke despite being preceded by months of continuous monitoring of the heart-rhythm.39 Second, other types of arrhythmias like PSVT have also been linked to stroke risk. Finally, those with a genetic mutation that is associated with AF like the gene for Natriuretic Peptide Precursor A, can have a stroke even before the onset of AF.40
- Kidney Disease : The risk of stroke is high in patients with chronic kidney disease, especially in patients on dialysis
- Diet and Exercise: low Physical inactivity is linked with many health issues, stroke included. In those who are physically active, their risk of stroke is lesser than those who are not active. The relationship is explained with the fact that exercising decreases blood pressure, reduces excess body fat and subsequently diabetes. 41
- Smoking is also considered a major risk factor for stroke, which nearly doubles the stroke risk. 42
- Alcohol. heavy drinking associated with an increased risk of ischemic stroke. 43
- Substance abuse like cocaine, heroin, amphetamines, and ecstasy have shown to increase risk of both the ischemic and hemorrhagic stroke. 44
a continuously updated well known and widely used score that is used to estimate a 10-year stroke risk stratified by the gender is the The Framingham Stroke Risk Profile (FSRP). It combines the various predictors of stroke like age, systolic blood pressure, anti-hypertensive therapy, diabetes, cigarette smoking, left ventricular hypertrophy by electrocardiogram, and the presence of cardiovascular disease (coronary heart disease, peripheral vascular disease, congestive heart failure). 45 There are other scores, which were developed from different population samples, that determine the risk of stroke and include additional metrics like physical disabilities, depression, and marital status. 46
CLINICAL PRESENTATION AND COMPLICATIONS
Stroke typically presents with a sudden rapid onset of neurological deficits. The signs and symptoms that the patient presents vary depending on the area of the brain is involved and whether a main artery or its branches are affected. Thus, the clinical presentation is influenced by the size of the infarct.
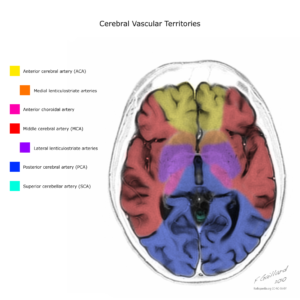
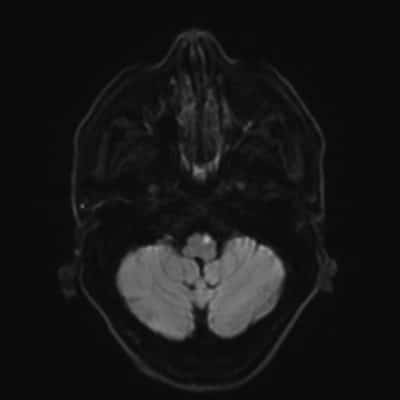
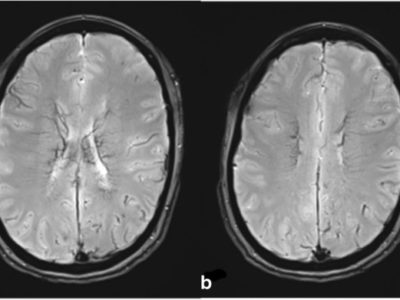
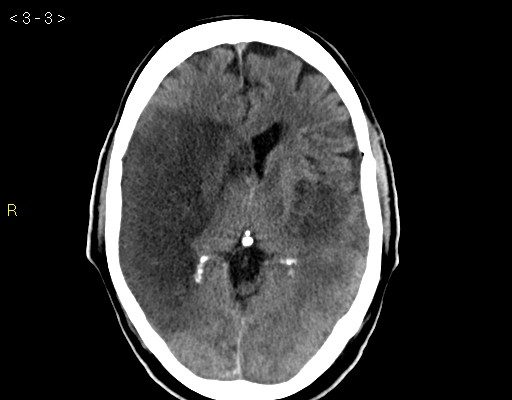
Figure 1. Case courtesy of Assoc Prof Frank Gaillard. |
Mainly, focal weakness and speech disturbance are the two most common physical findings of ischemic stroke. Other signs and symptoms of ischemic stroke that are also considered as most common are listed below: 13, 14, 15
Symptoms
- Subjective arm weakness
- Subjective leg weakness
- Self-reported speech disturbance
- Subjective facial weakness
- Arm paresthesia
- Leg paresthesia
- Headache
- Non-orthostatic dizziness
- Seizure
Signs
- Arm and/or leg paresis
- Aphasia
- Dysphasia or dysarthria
- Hemiparetic or ataxic gait
- Facial paresis
- Eye movement abnormality or diplopia
- Visual field defect
The person might be present with speech problems and will have a difficulty understanding what others are saying and may be confused. Face droopiness, which is the weakness of one side of the face, is another visible clinical finding. It is usually accompanied with vision problems in either one or both eyes. The person may have a blurred, blackened or a double vision. Moreover, he may develop a sudden weakness or feeling of numbness or the arm or leg. This often affects just one side of the body. To test this, ask the person to raise both arms over the head at the same time. If one arm begins to fall, it may be a sign that they are having a stroke. They may also have a problem with maintaining balance, so they will present with a troubled walking. Furthermore, a sudden, severe headache that is accompanied by vomiting, dizziness or altered consciousness, may indicate that they are having a stroke.
WORKUP AND DIAGNOSIS
History and physical examination are the initial steps to diagnosing stroke. The most important component to obtain from the history is when was the person last seen normal and with no symptoms. Stroke treatment is most effective when given as soon as possible as it has a narrow time window of effectiveness. Quick assessment of the person with suspected acute ischemic stroke is made to determine the most suitable intervention among the available options as well as further assess the eligibility for thrombolysis.16
Usually, The National Institutes of Health Stroke Scale (NIHSS) provides a quantitative measure of stroke-related neurologic deficit, its widely used as a clinical assessment tool to evaluate acuity of stroke patients, determine appropriate treatment, and predict patient outcome. The NIHSS is a 15-item neurologic examination stroke scale used to evaluate the effect of acute cerebral infarction on the levels of consciousness, language, neglect, visual-field loss, extraocular movement, motor strength, ataxia, dysarthria, and sensory loss. A trained observer rates the patent’s ability to answer questions and perform activities. Ratings for each item are scored on a 3- to 5-point scale, with 0 as normal, and there is an allowance for untestable items. Scores range from 0 to 42, with higher scores indicating greater severity.
Immediate Diagnostic Studies:
- Noncontrast brain CT or brain MRI
- Blood glucose
- Serum electrolytes and renal function tests
- Electrocardiograph
- Markers of cardiac ischemia
- Complete blood count, including platelet count
- Prothrombin time/international normalized ratio
- Activated partial thromboplastin time
- Oxygen saturation
For Selected patients, the following can be done:
- Hepatic function tests.
- Chest radiography if a lung disease is suspected.
- Lumbar puncture (if subarachnoid hemorrhage suspected and head CT
negative for blood). - Electroencephalogram, if seizure is suspected.
Despite the desire to know the results of these tests before giving the recombinant tissue plasminogen activator, thrombolytic therapy should not be delayed while awaiting the results unless a bleeding abnormality or thrombocytopenia is clinically suspected, or the patient has received heparin or warfarin used unknown anticoagulants.
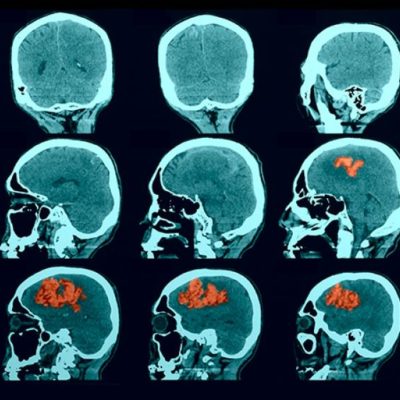
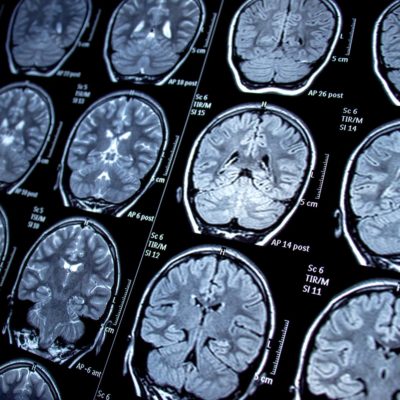
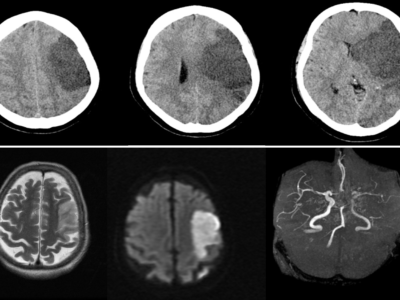
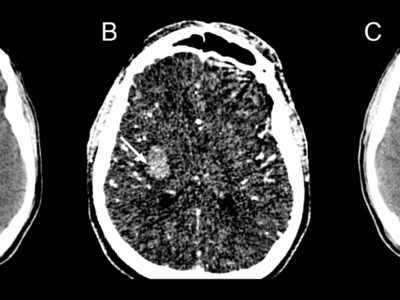
In order to be able to distinguish between ischemic stroke and hemorrhagic stroke as well as rule out other types of central nervous system lesions, neuro-images must be done. However, the choice of neuroimaging depends on its availability at the hospital, eligibility to be used for acute stroke intervention and if there are any patient contraindications present.
Clinically, the diagnosis of stroke is usually accurate but determining the pathological type of stroke is best achieved by conducting an early brain computed tomography (CT) scan or by performing an autopsy, for confirmation. A CT scan is not only needed to rule in the diagnosis of ischemic stroke, but also to exclude the presence of certain stroke mimics and detect hemorrhage. In other words, a normal CT scan does not rule out the diagnosis of ischemic stroke. 16
Although MRI scans have better resolution when compared to CT scans, they are less available and more expensive than CT scanners. Also, MRI scans cannot be performed on persons who have certain types of implanted devices (e.g., pacemakers) or in those who are claustrophobic. In addition, CT scans have a 95- 100% sensitivity of detecting subarachnoid blood in the first 12 hours; however, over time as the subarachnoid blood is cleared, its sensitivity greatly decreases to about 50% after one week and is not detectable by CT after a period of about two to three weeks, unlike ischemic stroke. 24, 27, 28
According to the guidelines, it is recommended that a MRI scan is ordered if it could be obtained as quickly as a CT scan and more importantly if the patient presented within the time window of acute stroke intervention. If not, then CT is the go-to test because when the history and physical is consistent for acute, its treatments should not wait for detailed imaging. 26
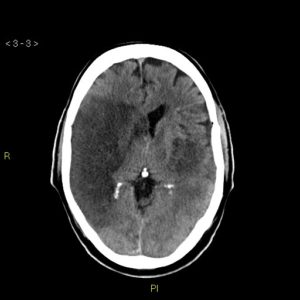
Figure 3. Middle Cerebral Artery (MCA) infarct 29 Case courtesy of Dr. Sajoscha Sorrentino.
Factors such as poor public awareness of symptoms, lack of quick detection by emergency medical services (EMS), poor coordination between EMS and the hospital emergency department or delay of diagnosis upon arrival at the emergency department are considered factors that contribute in the failure to provide prompt diagnosis and treatment of acute ischemic stroke.
STROKE MIMICS AND DIFFERENTIAL DIAGNOSIS
When evaluating a patient presenting with a suspected stroke, other possible conditions associated with the central nervous system must be ruled out as there is a large number of stroke- mimickers 18,20-23
- Seizures, status epilepticus in particular, can mimic a stroke
- Subdural hematomas (SDH), intracranial hemorrhages (ICH), or masses
- Demyelinating disorders like multiple sclerosis
- Toxic and metabolic differentials like Sepsis, uremia, hypo and hyperglycemia, hyponatremia, and hyperkalemia can all cause symptoms that resemble a stroke
- Complex migraines
- Systemic infections, the commonest source is the chest.
- Dementia.
- Psychiatric disorders like panic disorders.
- Could be associated with alcohol intoxication, an adverse effect to a secondhand medication or other encephalopathy
- References
- Gibson CL. Cerebral ischemic stroke: Is gender important? J Cereb Blood Flow Metab. 2013;33:1355–61.
- Tsivgoulis, Georgios et al. “Recent Advances in Primary and Secondary Prevention of Atherosclerotic Stroke.” Journal of stroke vol. 20,2 (2018): 145-166. doi:10.5853/jos.2018.00773
- Nogles TE, Galuska MA. Middle Cerebral Artery Stroke. [Updated 2020 Aug 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556132/
- Matos Casano HA, Tadi P, Ciofoaia GA. Anterior Cerebral Artery Stroke. [Updated 2020 Jul 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537333/
- Toyoda K. Anterior cerebral artery and Heubner’s artery territory infarction. Front Neurol Neurosci. 2012;30:120-2.
- . Case courtesy of Dr Henry Knipe, <ahref=”https://radiopaedia.org/”>Radiopaedia.org</a>. From the case <a href=”https://radiopaedia.org/cases/39328″>rID: 39328</a>
- Mozzafarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al., on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation 2016;133(4):e38–360.
- American Heart Association/American Stroke Association. TIA (Transient Ischemic Attack)external icon. Accessed October 6, 2016.
- Kalaria RN, Akinyemi R, Ihara M. Stroke injury, cognitive impairment and vascular dementia. Biochim Biophys Acta. 2016;1862(5):915-925. doi:10.1016/j.bbadis.2016.01.015
- Su H. Inflammation and genetic factors in stroke pathogenesis. Neuroimmunol Neuroinflamm. 2017;4:260-262. doi:10.20517/2347-8659.2017.22
- Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, Mensah GA, Norrving B, Shiue I, Ng M, Estep K, Cercy K, Murray CJL, Forouzanfar MH., Global Burden of Diseases, Injuries and Risk Factors Study 2013 and Stroke Experts Writing Group. Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016 Aug;15(9):913-924.
- O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, Rao-Melacini P, Zhang X, Pais P, Agapay S, Lopez-Jaramillo P, Damasceno A, Langhorne P, McQueen MJ, Rosengren A, Dehghan M, Hankey GJ, Dans AL, Elsayed A, Avezum A, Mondo C, Diener HC, Ryglewicz D, Czlonkowska A, Pogosova N, Weimar C, Iqbal R, Diaz R, Yusoff K, Yusufali A, Oguz A, Wang X, Penaherrera E, Lanas F, Ogah OS, Ogunniyi A, Iversen HK, Malaga G, Rumboldt Z, Oveisgharan S, Al Hussain F, Magazi D, Nilanont Y, Ferguson J, Pare G, Yusuf S., INTERSTROKE investigators. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016 Aug 20;388(10046):761-75.
- Interobserver agreement for the bedside clinical assessment of suspected stroke.Hand PJ, Haisma JA, Kwan J, Lindley RI, Lamont B, Dennis MS, Wardlaw JM Stroke. 2006 Mar; 37(3):776-80
- The Recognition of Stroke in the Emergency Room (ROSIER) scale: development and validation of a stroke recognition instrument. Nor AM, Davis J, Sen B, Shipsey D, Louw SJ, Dyker AG, Davis M, Ford GA Lancet Neurol. 2005 Nov; 4(11):727-34.
- Is this patient having a stroke? Goldstein LB, Simel DL JAMA. 2005 May 18; 293(19):2391-402.
- Yew, Kenneth S, and Eric Cheng. “Acute stroke diagnosis.” American family physician vol. 80,1 (2009): 33-40.
- Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354(4):387–396. Medline.
- Hand PJ, Kwan J, Lindley RI, Dennis MS, Wardlaw JM. Distinguishing between stroke and mimic at the bedside: the brain attack study. Stroke. 2006;37(3):769–775. Medline.
- Albers GW, Caplan LR, Easton JD, et al. Transient ischemic attack–proposal for a new definition. N Engl J Med. 2002;347(21):1713–1716. Medline.
- Libman RB, Wirkowski E, Alvir J, Rao TH. Conditions that mimic stroke in the emergency department. Implications for acute stroke trials. Arch Neurol. 1995;52(11):1119–1122. Medline
- Hemmen TM, Meyer BC, McClean TL, Lyden PD. Identification of nonischemic stroke mimics among 411 code strokes at the University of California, San Diego, Stroke Center. J Stroke Cerebrovasc Dis. 2008;17(1):23–25. Medline.
- Hosseininezhad M, Sohrabnejad R. Stroke mimics in patients with clinical signs of stroke. Caspian J Intern Med. 2017 Summer;8(3):213-216.
- Vilela P. Acute stroke differential diagnosis: Stroke mimics. Eur J Radiol. 2017 Nov;96:133-144. doi: 10.1016/j.ejrad.2017.05.008. Epub 2017 May 5. PMID: 28551302.
- Kidwell CS, Chalela JA, Saver JL, et al. Comparison of MRI and CT for detection of acute intracerebral hemorrhage. JAMA. 2004;292(15):1823–1830. Medline.
- Fiebach JB, Schellinger PD, Gass A, et al. Stroke magnetic resonance imaging is accurate in hyperacute intracerebral hemorrhage: a multicenter study on the validity of stroke imaging. Stroke. 2004;35(2):502–506. Medline. [PubMed] [Google Scholar]
- Adams HP, Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists [published corrections appear in Stroke. 2007;38(6):e38, and Stroke. 2007;38(9):e96] Stroke. 2007;38(5):1655–1711. Medline.
- Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354(4):387–396. Medline.
- Masdeu JC, Irimia P, Asenbaum S, et al. EFNS guideline on neuroimaging in acute stroke. Report of an EFNS task force. Eur J Neurol. 2006;13(12):1271–1283. Medline.
- Case courtesy of Dr Sajoscha Sorrentino, <a href=”https://radiopaedia.org/”>Radiopaedia.org</a>. From the case <a href=”https://radiopaedia.org/cases/14777″>rID: 14777</a>
- Merwick Á, Werring D. Posterior circulation ischaemic stroke. BMJ. 2014;348 (may19 33): g3175. doi:10.1136/bmj.g3175
- Searls DE, Pazdera L, Korbel E et-al. Symptoms and signs of posterior circulation ischemia in the new England medical center posterior circulation registry. (2012) Archives of neurology. 69 (3): 346-51. doi:10.1001/archneurol.2011.2083
- Navarro-Orozco D, Sánchez-Manso JC. Neuroanatomy, Middle Cerebral Artery. [Updated 2020 Aug 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526002/
- Boehme AK, Esenwa C, Elkind MS. Stroke Risk Factors, Genetics, and Prevention. Circ Res. 2017;120(3):472-495. doi:10.1161/CIRCRESAHA.116.308398
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Executive summary: Heart disease and stroke statistics–2012 update: A report from the american heart association. Circulation. 2012;125:188–197
- Asplund K, Karvanen J, Giampaoli S, Jousilahti P, Niemela M, Broda G, et al. Relative risks for stroke by age, sex, and population based on follow-up of 18 european populations in the morgam project. Stroke. 2009;40:2319–2326.
- Cruz-Flores S, Rabinstein A, Biller J, Elkind MS, Griffith P, Gorelick PB, et al. Racial-ethnic disparities in stroke care: The american experience: A statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42:2091–2116.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The jnc 7 report. JAMA. 2003;289:2560–2572.
- Banerjee C, Moon YP, Paik MC, Rundek T, Mora-McLaughlin C, Vieira JR, et al. Duration of diabetes and risk of ischemic stroke: The northern manhattan study. Stroke; a journal of cerebral circulation. 2012;43:1212–1217.
- Brambatti M, Connolly SJ, Gold MR, Morillo CA, Capucci A, Muto C, et al. Temporal relationship between subclinical atrial fibrillation and embolic events. Circulation. 2014;129:2094–2099.
- Disertori M, Quintarelli S, Grasso M, Pilotto A, Narula N, Favalli V, et al. Autosomal recessive atrial dilated cardiomyopathy with standstill evolution associated with mutation of natriuretic peptide precursor a. Circulation. Cardiovascular genetics. 2013;6:27–36.
- . Manson JE, Colditz GA, Stampfer MJ, Willett WC, Krolewski AS, Rosner B, et al. A prospective study of maturity-onset diabetes mellitus and risk of coronary heart disease and stroke in women. Arch Intern Med. 1991;151:1141–1147.
- Bhat VM, Cole JW, Sorkin JD, Wozniak MA, Malarcher AM, Giles WH, et al. Dose-response relationship between cigarette smoking and risk of ischemic stroke in young women. Stroke. 2008;39:2439–2443.
- Hillbom M, Numminen H, Juvela S. Recent heavy drinking of alcohol and embolic stroke. Stroke. 1999;30:2307–2312.
- Brust JC. Neurological aspects of substance abuse. Butterworth-Heinemann; Philadelphia, Pa: 2004.
- Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: A risk profile from the framingham study. Stroke. 1991;22:312–318.
- Boehme AK, Esenwa C, Elkid MS. Stroke Risk Factors, Genetics, and Prevention. Circ Res. 2017;120(3):472-495. doi:10.1161/CIRCRESAHA.116.308398