Article topic: Dural arteriovenous fistula.
Author: Bshara Jreisat.
Editors: Haneen A. Banihani, Rahmeh Adel.
Reviewer: Adam Abdullah.
keywords: arteriovenous, fistula, inferior vena cava, endovascular treatment.
Abbreviations:
dAVFs: Dural arteriovenous fistulas, AVMs: Arteriovenous malformation, CVD: Cortical vein drainage, LFM DAVFs: lateral foramen magnum Dural arteriovenous fistula, IVVP: inferior vena cava pressure, EVT: Endovascular treatment.
Overview
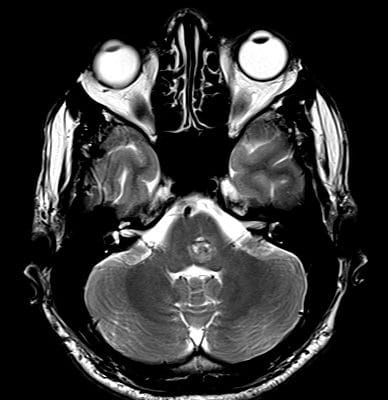
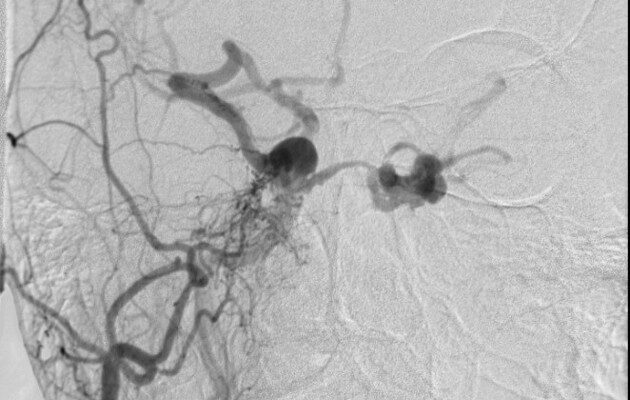
Dural arteriovenous fistulas (dAVFs), in some cases, called Dural arteriovenous malformation (AVMs), are anomalous and abnormal connections between the arterial and venous systems within the protective dural layer of the brain [Figure 1]. The exact cause of dAVFs is usually not known, but they are believed to develop
as a result of factors like trauma, surgical interventions, venous narrowing, or blood clot formation in the brain’s venous sinuses. These abnormal vascular connections are most frequently found near the dural venous sinuses in the cranial area1.
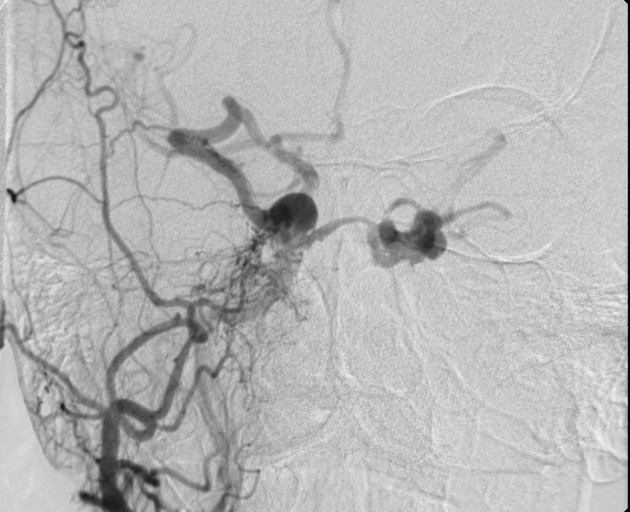
Figure 1: Dural arteriovenous fistula, (yap, 2019) (2)
Pathogenesis and Etiology
Even though we don’t fully understand the underlying mechanisms of these lesions, it appears that Dural Arteriovenous Fistulas (dAVFs) in adults are primarily acquired conditions. They involve multiple blood vessels originating from specific areas of the meninges and are supplied by arteries such as the external/internal carotid and vertebral arteries. Previous factors such as craniotomy, injuries, blood clot formation, and underlying thrombotic disorders like protein C/S deficiency and Factor V Leiden have been suggested as potential contributing factors3.
It is believed that the development of dAVFs may be linked to the gradual narrowing of the dural venous sinuses; clot formation in the dural venous sinuses which could trigger the formation of new blood vessels (neoangiogenesis) as part of the disease’s pathogenesis; and previously thrombosed dural venous sinus.
The primary anomaly seen in dural arteriovenous fistulas (dAVFs) is the formation of connections between dural arteries and veins within the walls of venous sinuses, typically through small vessels averaging around 30 micrometers in diameter. In cases where there is an identifiable triggering event, the development of new blood vessels (neovascularization) is often initiated by a previously thrombosed dural venous sinus, with the transverse sinus being a common site4.
For patients with idiopathic fistulas, the condition is usually associated with prior asymptomatic blood clot formation within a dural venous sinus. This clot formation is often a result of inherited conditions that increase the risk of blood clot formation, such as anti-thrombin, protein C deficiency, and protein S deficiency, or due to systemic illnesses and conditions that promote a Pro-thrombotic state4.
Classification
We have two types of Classification5:
1. Borden classification of (dAVFs):
| Type | Venous drainage site | CVD |
| “Benign” | ||
| Type I | Dural sinus | No |
| “Aggressive” | ||
| Type II | Dural sinus | Yes |
| Type III | Cortical vein | Yes |
2. Cognard classification of (dAVFs):
| Type | Venous drainage site | CVD | Flow pattern |
| “Benign” | |||
| Type I | Dural sinus | No | Antegrade |
| Type IIa | Dural sinus | No | Retrograde |
| “Aggressive” | |||
| Type IIb | Dural sinus | yes | Antegrade |
| Type II (a+b) | Dural sinus | yes | Retrograde |
| Type III | Cortical vein | yes | Retrograde |
| Type IV | Cortical vein | yes | – |
| Type V | Cortical vein | yes | – |
Clinical Presentation and Complication
Clinical presentation of dural Arteriovenous Fistula (dAVF) includes Pulsatile tinnitus, which might be the main characteristic when the dAVF is very close to the petrous bone; Intracranial hemorrhage in the lateral foramen magnum Dural arteriovenous fistulas (FM DAVFs) is not uncommon and is often linked to the drainage of the brainstem venous system. Myelopathy: In cases of lateral foramen magnum Dural arteriovenous fistulas (FM DAVFs) where venous reflux flows into the inferior portion of the intracranial vertebral venous plexus (IVVP system), it is most likely that symptoms of spinal venous congestion, such as quadriparesis, will manifest. Cranial nerve palsy: Cranial nerve palsy is rare and mainly presents as hypoglossal nerve palsy and there are two possibilities for this condition: the first is ischemic neuropathy of the vasa nervorum of the cranial nerve and the second is neuropathy secondary to venous congestion (6).
Workup and Diagnosis
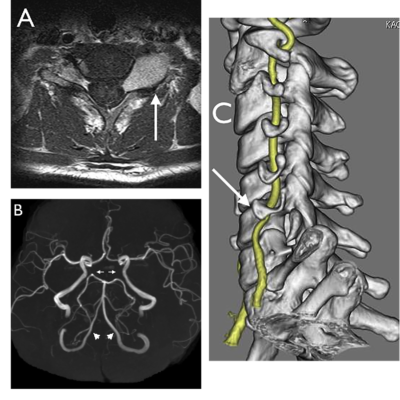
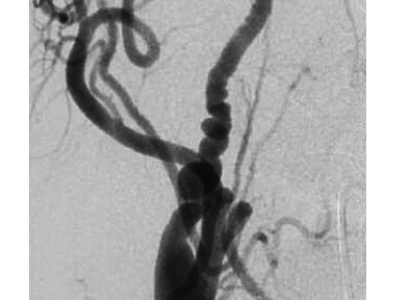
The diagnosis of foramen magnum dural arteriovenous fistulas (FM DAVFs) is challenging because of the intricate vascular network in this area, including small and winding feeder vessels. Presently, various imaging techniques such as head computed tomography (CT), CT angiography (CTA), magnetic resonance imaging (MRI), magnetic resonance angiography (MRA), and digital subtraction angiography (DSA) are valuable tools for establishing a diagnosis of FM DAVFs6.
Treatment
The treatment of a Dural arteriovenous fistula (DAVF) typically depends on the specific characteristics of the DAVF, its location, and the patient’s overall health.
Treatment options for DAVFs include Observation, particularly if the DAVF is small, asymptomatic, and considered low risk, a medical team may choose to closely monitor the condition without immediate intervention. Endovascular Embolization; is a minimally invasive procedure that involves threading a catheter through the arteries to the site of the DAVF and injecting a substance to block the abnormal connection, thereby stopping the abnormal blood flow.
Surgical removal of the DAVF may be necessary in cases where endovascular embolization is not feasible or has not been successful. Surgical options include craniotomy, where the DAVF is accessed through an opening in the skull or transarterial or transvenous approaches. Radiosurgery; Stereotactic radiosurgery, such as gamma knife or CyberKnife, may be used for smaller DAVFs that are deep or difficult to access through surgery. It involves delivering highly focused radiation to the DAVF to close off the abnormal blood flow over time. Combined Approaches in Complex Cases; a combination of treatments, such as endovascular embolization followed by surgery or radiosurgery, may be employed to achieve the best outcome 1,5,7.
The choice of treatment depends on factors like the location and size of the DAVF, the patient’s overall health, and the risks associated with each approach. It is crucial to consult with a medical specialist, typically an interventional neuroradiologist or neurosurgeon, to determine the most appropriate treatment strategy for an individual DAVF case. Left untreated, some DAVFs can lead to serious neurological problems, so prompt evaluation and treatment are essential.
Prevention
It is crucial to take preventive measures to avoid complications like venous infarction and cerebral hemorrhage. One method to achieve this is by employing a remodeling balloon in the primary draining vein. This balloon can be temporarily inflated to block the forward flow of blood in the vein during the Onyx embolization of the fistulous venous pouch1.
References
Read more
- Baharvahdat, Humain, et al. “Updates in the Management of Cranial Dural
Arteriovenous Fistula.” Stroke and Vascular Neurology, vol. 5, no. 1, Nov. 2019, pp. 50–58, https://doi.org/10.1136/svn-2019-000269. Accessed 15 Feb. 2022. - yap, Joshua. (2022, October 22). Radiology Quiz 4554 | Radiopaedia.org. Radiopaedia.https://radiopaedia.org/cases/4554/studies/6675lang=us&source_of=https%3A%2F%2Fradiopaedia.org%2Farticles%2Fdural-arteriovenous-fistula%3Flang%3Dus.
- Chen, Patrick M., et al. “Cranial Dural Arteriovenous Fistula.” Stroke, vol. 49, no. 12,Dec. 2018, https://doi.org/10.1161/strokeaha.118.022508. Accessed 3 Mar. 2021.
- Zyck S, De Jesus O, Gould GC. Dural Arteriovenous Fistula. 2023 Aug 14. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 30335307.
- Gandhi, D., et al. “Intracranial Dural Arteriovenous Fistulas: Classification, Imaging Findings, and Treatment.” American Journal of Neuroradiology, vol. 33, no. 6, Jan.2012, pp. 1007–13, https://doi.org/10.3174/ajnr.a2798. Accessed 24 Dec. 2019.
- Li, Chao, et al. “Dural Arteriovenous Fistula of the Lateral Foramen Magnum Review.” Interv Neuroradiol, vol. 24, no. 4, May 2018, pp. 425–34,
https://doi.org/10.1177/1591019918770768. Accessed 15 May 2023. - Hou, Kun, et al. “Endovascular Treatment of the Cavernous Sinus Dural Arteriovenous Fistula: Current Status and Considerations.” International Journal of Medical Sciences,vol. 17, no. 8, 2020, pp. 1121–30, https://doi.org/10.7150/ijms.45210. Accessed 21 Jan.2023
[/read]