Article topic: Causes of Ischemic Stroke
Author: Fadi Haddad
Editors: Yaman Oudat, Ethar Hazaimeh
Keywords: Stroke, Classifications, Atherosclerosis, Cardioembolism
Introduction
Stroke can be defined as an acute episode of focal neurological deficit (brain, retina, or spinal cord) lasting longer than 24 h, or of any duration if radiological or pathological evidence of infarction or hemorrhage relevant to the symptoms, involving a defined cerebral vascular territory.1 In the US, the number of adults who ever had a stroke is 7.8 million and the percent of adults who ever had a stroke is 3.1%, and it is ranked as the 5th leading cause of death.2 It is important to establishing the most likely cause of an ischemic stroke as it influences both short-term and long-term prognoses and it affects treatment decisions.3 Throughout history, many classifications of strokes have been defined such as; The Trial of Org 10172 in Acute Stroke Treatment (TOAST) Classification, The Spanish Classification system (GEECV/SEN), and The SPARKLE classification.4-6 TOAST classification shows a logical and clinically oriented system and supports other independent assessments.4 TOAST classification became the most widely used system to identify the etiology of strokes.7
TOAST Classification
TOAST classification has subdivided ischemic stroke into 5 categories: Large-artery atherosclerosis (embolus/thrombosis), Cardioembolism (high-risk/medium-risk), Small-vessel occlusion (lacune), Stroke of other determined etiology, Stroke of undetermined etiology (Two or more causes identified, Negative evaluation or Incomplete evaluation). It is based on specific clinical, radiological, and laboratory investigations (Table 1), which will help in guiding proper management.
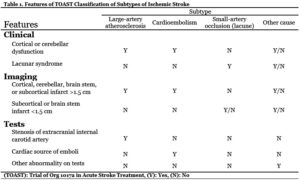
Table 1. Features of TOAST classification of subtypes of Ischemic stroke
- Large Artery Atherosclerosis:
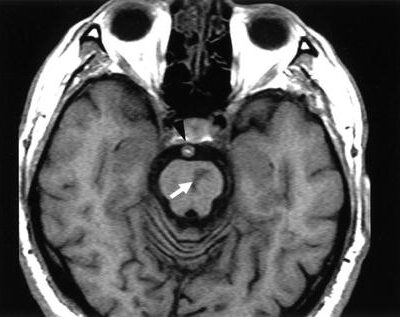
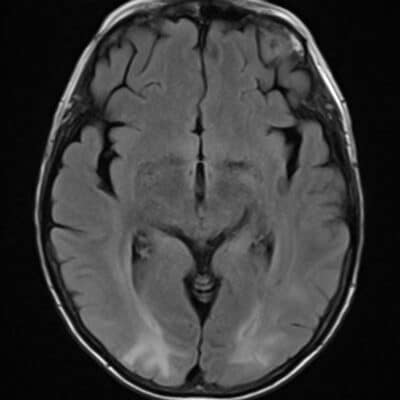
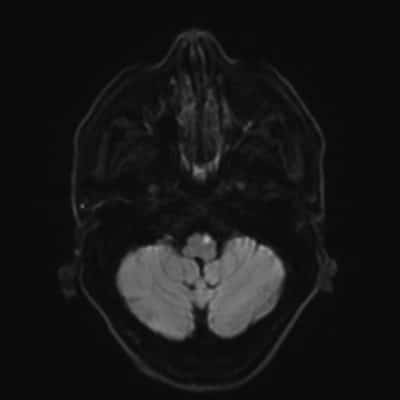
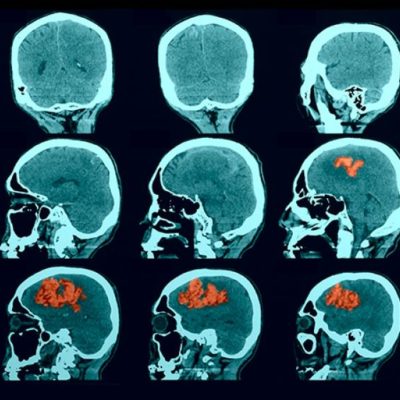
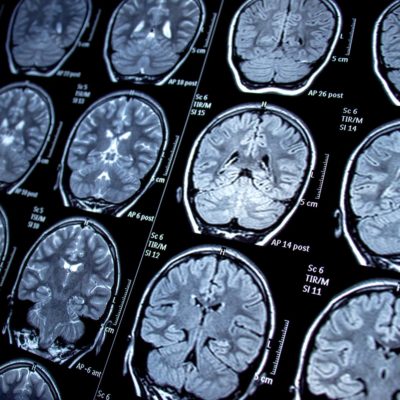
Is defined as the presence of well-notable stenosis or occlusion (>50%) due to atherosclerosis of the major arteries of the brain (e.g., Internal carotid artery, and the basilar artery) or a Branch vessel (e.g. Anterior, posterior, and middle cerebral arteries) accompanied by an infarction larger than 15mm in diameter on Computed Tomography (CT) scanning or Magnetic Resonance Imaging (MRI), with clinical findings of cortical, cerebellar or brain stem damage depending on the occulted artery.8-11 Large Artery Atherosclerosis is the most common cause of stroke forming (37.3%) of cases and in which, the most common territory affected is the territory of the middle cerebral artery (49.6%).12 The arterial circulation of the brain can be divided into anterior and posterior circulations; regarding the anterior circulation, Middle Cerebral Artery (MCA) is most frequently involved and covers parts of the parietal lobe, the frontal lobe, and the temporal lobe (Figure 1).13 Anterior Cerebral Artery infarction is a rare entity as it represents 0.5–3% of all ischemic strokes. It occurs most frequently on the left side of the brain, with contralateral hemiparesis or monoparesis as the most common presentation (Figure 2).14-16 The posterior circulation covers the occipital lobe, cerebellum, and brain stem. The symptoms of which occur according to the involved location (Figure 3).17
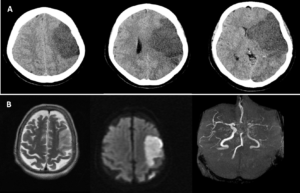
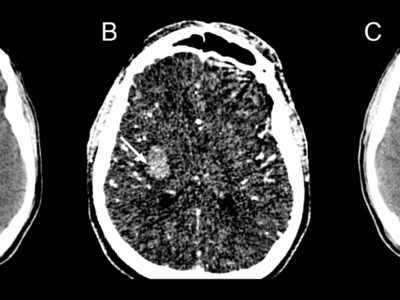
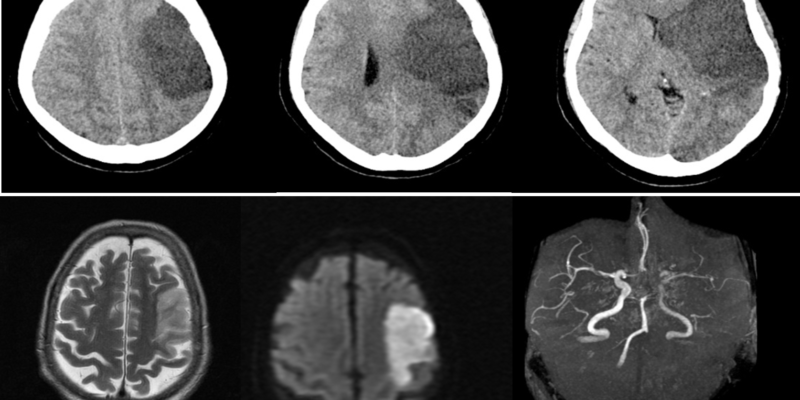
Figure 1. (A) Axial CT scan without contrast of the brain for a 60-years-old female patient presented with acute right-sided weakness showing a progression of MCA territory infarct with marked midline shift.18 (B) Axial T2 and DWI weighted MRI of the brain, and an MRA showing a well-defined area of high T2 signal with diffusion restriction in the left MCA territory. Loss of signal in the left MCA and its branches on the MRA.19
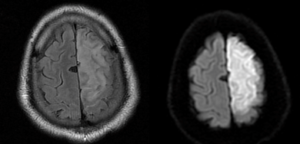
Figure 2. Axial Flair and DWI weighted MRI of the brain for a 50-years-old male presented with acute onset right lower limb weakness, showing DW imaging confirms acute infarction – territorial to left ACA.20
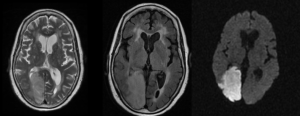
Figure 3. Axial T2. FLAIR and DWI MRI of the brain of an 85-years-old female presented with right-sided weakness and decreased vision showing right-sided PCA territory infarct showing hyperintense T2/FLAIR signals and diffusion restriction. Confluent high signal foci in T2 and FLAIR sequences at subcortical, centrum semiovale, and periventricular white matter of both cerebral hemispheres (Fazekas grade III) depict microvascular ischemic events.21
- Cardioembolism
The findings of Cardioembolism strokes are similar to those of large artery atherosclerosis but differ as they are originated from the heart. They are mostly associated with a variety of conditions including mechanical prosthetic valves, atrial fibrillation or flutter, recent myocardial infarction (<4 wk), dilated cardiomyopathy, infective endocarditis Regional left ventricular akinesis, or rheumatic heart disease (Figure 4). It accounts for 20-30% of ischemic strokes.22,23
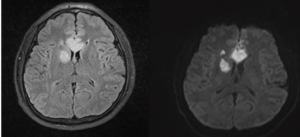
Figure 4. Axial DWI and FLAIR MRI for a 40-years-old male presented with an altered conscious level showing Extensive restricted diffusion in the rostrum, genu, and body of the corpus callosum. Further foci of restricted diffusion of variable size in the right internal capsule, corpus striatum, centrum semiovale, and insula. All consistent with acute infarcts.24
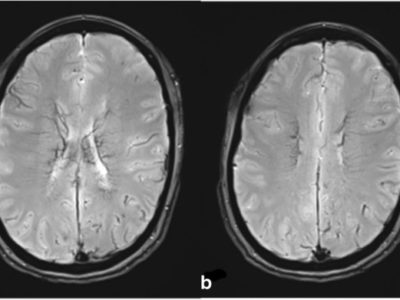
- Small-vessel occlusion
Also known as Lacunar Strokes (LS); are defined as small infarctions occurring in the terminal branches of large cortical arteries. The main branches involved are derived from PCA territory. This can be due to a numerous number of causes; hypertension, dyslipidemia, and Diabetes Mellitus (DM). Moreover, it accounts for 20-30% of ischemic strokes.25-28 They are clinically significant when infarcts are between 5 mm to 15 mm in diameter and involving the deep gray and subcortical white matter (Figure 5).27
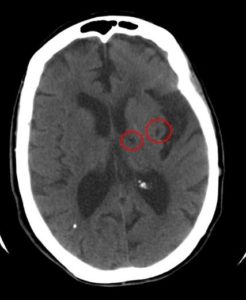
Figure 5. Axial CT without contrast of the brain showing two small hypoattenuating areas on left thalamic and insular region.29
- Strokes of other determined etiology
This kind of stroke accounts for 2-11% of ischemic strokes.30 It can be due to a variety of causes such as vasculopathy (the most common cause) and is mostly associated with cytomegalovirus (CMV), human immunodeficiency virus (HIV) and Varicella zoster virus (VZV)31, and hypercoagulable states (e.g. antithrombin III, protein S, and protein C deficiencies) 32,33, hematological disorders representing 1.3% of the causes of all acute strokes34, right to left vascular shunts35, and arterial dissections.36
- Strokes of undetermined etiology
Despite intensive investigation, 25% of ischemic strokes do not any have identified etiologies.37 This kind of stroke can be due to emboli of undetermined sources because they are not usually detected by conventional imaging techniques. Those causes might be patent foramen ovale38, paroxysmal atrial fibrillation39, aortic arch atherosclerosis40,3or non-stenosing atherosclerosis of the carotid arteries.41