Article topic: Carotid Body Tumors
Author: Layan Abuqayyas
Scientific editor: Dr.Omar Jbara
Linguistic editor: Philip Sweidan
Overview
The carotid body is a small organ, measuring 2-6mm, located in the dorsal aspect at the bifurcation of the Carotid Artery bilaterally(1). Carotid artery tumors are a type of neuroendocrine tumors (NET) that arise from the paraganglionic neurons derived from embryonic neuronal tissue. Carotid Body tumors are the most common head and neck paraganglioma (2).
Etiology and Pathogenesis
The carotid bodies are composed of non-chromaffin cells from which tumors descend. They are divided into functional and non-functional. The vast majority of tumors are non-functional and the rare cases of functional non-chromaffin cell tumors release catecholamines like norepinephrine and epinephrine.
Due to the close proximity of the carotid body to major blood vessels, tumors are highly vascular and certain growth factors are implicated in their angiogenic physiology: Vascular Endothelial Growth Factor (VEGF) and Platelet Derived Endothelial Cell Growth Factor (PD-ECGF). Moreover, the prevalence in females is higher than males (2:1) and more at higher altitudes (2000m above sea level) due to tumors expressing estrogen receptors and hypoxia acting as an environmental trigger to the genetics. (3)
CBT can occur in sporadic and familial forms, and various oncogenes are culprits in both forms of occurrences. Sporadic tumors are unilateral in 95% of cases. Gardner and colleagues performed seminal genetic studies and found an increased expression of (c-myc, bcl-2, and c-jun) in the tumors. Further confirmation on the role of oncogenes was proven by Wang and colleagues, where the oncoprotein (bcl-2) was studied and found to have a tendency to deregulate cell death, therefore, playing a vital role in the formation of the carotid body tumors.
The succinate dehydrogenase (SDH) mutation is linked to an earlier age of onset, multiple paragangliomas, and a positive family history. This mutation is present in both forms with increased incidence in familial cases (83%) than in sporadic (11%).(4)
Clinical presentation
CBTs are mostly benign tumors which present as an asymptomatic anterior neck mass, but if they grew large enough they may have a mass effect that present with signs and symptoms of fullness, dysphagia, odynophagia, tongue weakness or atrophy. This is attributed to the close proximity of the carotid body to the Vagus and Hypoglossal nerves (seen in 10%).(1)
The functional variant of CBT is relatively rare (4%)(3), and the release of catecholamines causes a presentation with symptoms of headache, flushing, palpitations, or increased blood pressure and heart rate.(1)
Workup and Diagnosis
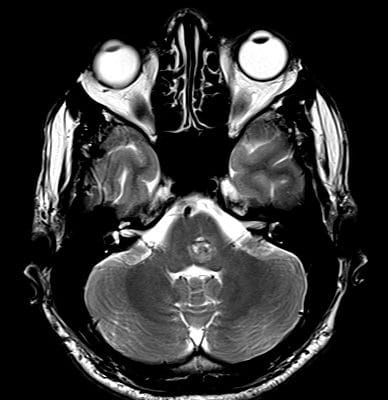
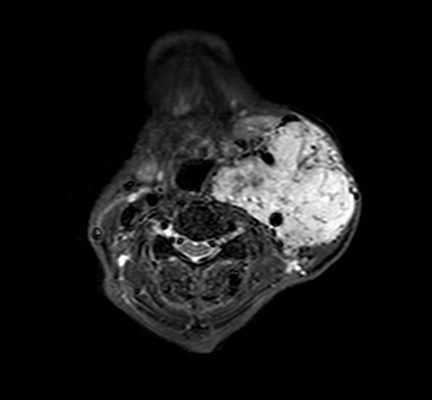
CBTs are identified after clinical examination or found incidentally on imaging. The differential diagnoses for masses in the high cervical area include: carcinoma, lymphadenopathy, leiomyomas and branchial cleft cysts. Thus, a cervical MRI with and without contrast can help differentiate CBT(3) (Fig.1). Color flow carotid duplex has become the ideal screening test for CBTs, where a well-circumscribed hypoechoic mass is seen splaying the carotid bifurcation. Other radiographic modalities that can be used to support the diagnosis: CT with or without contrast, and ultrasound.(1)
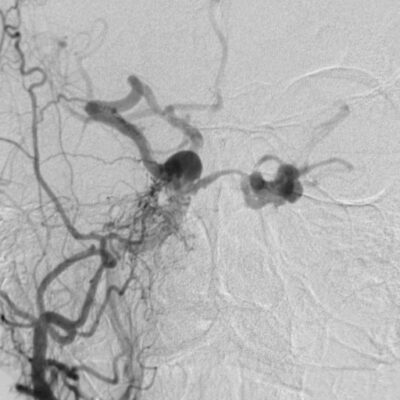
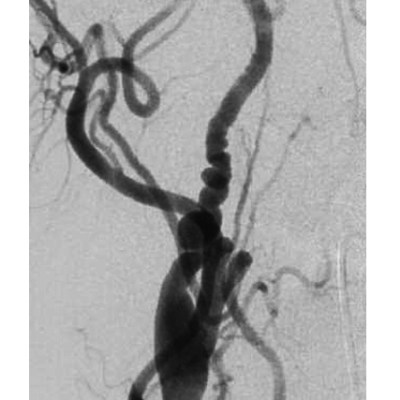
The highly vascular nature of the tumor is problematic if surgical resection is done without angiography (Fig.2), as it is needed to delineate the exact blood supply for the tumor. The ascending pharyngeal artery is the biggest contributor in most cases, and the superior thyroid artery plays a minor role. Variations in the vascularity should be assessed carefully.(3)
Once the mass is confirmed to be a CBT, endocrine workup is prompted, especially in patients with high blood pressure or palpitations. (3)
Classification:
Shamblin and associates created a three-group system for CBT according to the location and important landmarks. Group I tumors are at the bifurcation between the ICA and ECA with no vessels or nerves traversing the tumor, they are easily dissectible. Grade II is partially associated with the ECA and ICA, they invade the adventitia, but do not completely enclose the arteries. Grade III tumors completely enclose the ICA and may invade the adventitia all the way to the muscularis. Grade III is the hardest to resect due to the superior laryngeal and hypoglossal nerves traversing the tumor, and the need for ICA reconstruction.(3)
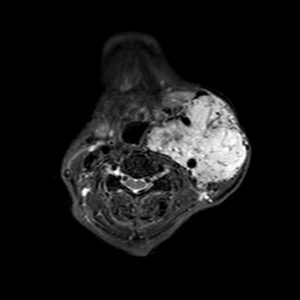
Fig.1: Axial MRI T1 showing a large enhancing vascular conglomerate soft tissue mass splaying the external and internal carotid arteries sitting between them, representing a carotid body tumor. Case courtesy of Dr. HanniMakky.(5)
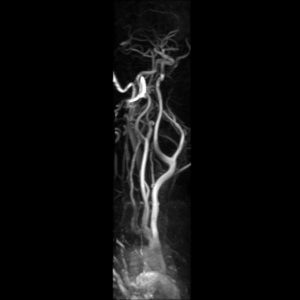
Fig.2: Angiography showing a large enhancing vascular conglomerate soft tissue mass splaying the external and internal carotid arteries sitting between them, representing a carotid body tumor. Case courtesy of Dr. HanniMakky.(5)
Treatment:
Preoperative planning is crucial to assess endocrine abnormalities due to catecholamine release. These patients should be given alpha-blockade two weeks prior to surgery and further beta-blockade to control heart rate and arrhythmias. Diagnostic cerebral angiography is done to assess for collateral cerebral blood flow. (3)
Evaluation of tumor extent horizontally and vertically, neural involvement, and infiltration of the ICA and other blood vessels is warranted to reduce morbidity and mortality.(4)
Smaller tumors (2-3cm) are resected easily, while bigger ones may require embolization to decrease the risk of blood loss.(3) Embolization is indicated for larger tumors, Shamblin group III and tumors with cranial extension(6). Superselective catherization is done after angiography to embolize the smaller vessels supplying the tumor without disrupting blood flow through the major vessels. Surgery is done no later than 48 hours after embolization to decrease soft tissue inflammation(3). Embolizaton carries the risk of transient ischemic attacks and stroke(6).
Tumors of grade III that encase the ICA may not be good candidates for surgical resection. Therefore, balloon occlusion testing is done to assess the possibility of resection and its effect on the ICA. The cerebral blood flow is assessed continuously intraoperatively using Compressed Spectral Array Electroencephalography (CSA-EEG) and a decrease in the cerebral blood flow may cue the surgeon to perform intraoperative shunting. (3)
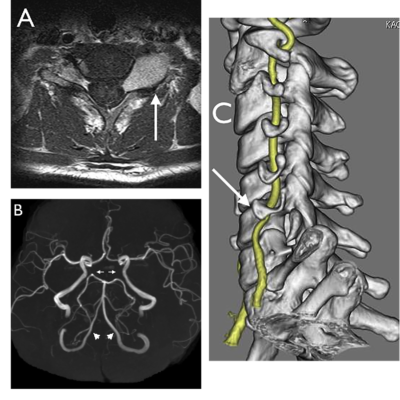
The incision will depend on the group. Group I and II may be resected with a curvilinear incision along the middle portion of the tumor, or a straight incision along the sternocleidomastoid. For Group III, a radial neck T incision is advised to properly view the tumor. (Fig.3). Bilateral tumors are operated separately, with removal of the largest one first. (1)
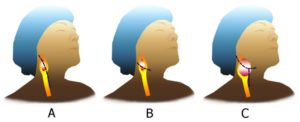
Fig.3: A and B for grade I and II, C for grade III. (7)
Upon exposure, identifying the vagus and hypoglossal nerves is important as the hypoglossal nerve may be superior and posterior to the tumor. In group III, the nerves traversing the tumor may be damaged and surgery will be difficult and associated with irreversible damages. In larger tumors extending higher in the neck, or patients with shorter necks, exposure higher up the extracranial ICA is necessary.
Superiorly, the oblique incision is continued anterior to the tragus up to the root of zygoma. Mobilization of the parotid gland is done to ensure the safety of the lower division of the facial nerve, followed by tracking of the hypoglossal nerve along its course between the ECA and ICA and mobilization of it. Inferiorly, the stylohyoid and digastric muscles along with the stylomandibular ligament are divided to expose the distal ICA. (3)
Radiotherapy is considered for patients at higher risk to undergo surgical resection due to extensive involvement, anesthetic risks, and multiple tumors. It helps reduce the tumor size and stops the growth.(1)
Prognosis
The benign etiology of most CBTs make their prognosis related to the local invasion of vascular and nervous structures. Prognosis depends on the preoperative measures done; to decrease mortality and morbidity, along with surgical complications.(3)
Some CBTs are malignant (5-10%) and distant metastasis may occur in rare cases to lymph nodes, bone, lung, liver, pancreas, thyroid, renal, brain, and breast. The treatment modality in local malignant CBT is surgical. However, in distant metastasis, it is yet to be identified.(2)
External Resources:
- Carotid Body Tumor Excision (CharudattaBavare, MD, M. MujeebZubair MD) – YouTube
- CAROTID BODY TUMOR – RESECTION WITHOUT EMBOLIZATION – YouTube
- Resection of a Carotid Body Tumor – YouTube