Article topic: Brainstem Cavernoma
Author : Ali Ifraitekh
Editors: Rawan Hamamreh, Yasmeen Alabdallat
Scientific Editor: Adam M. Abdallah
keywords: Cavernous Hemangioma, Cavernoma, angioma, malformation, Brainstem, Vascular malformation
Overview
Cavernoma, Cavernous angioma, Cavernous hemangioma, Cavernous malformation, and cerebral cavernous malformations are all terms describing the same disease (2). A cavernoma usually presents in the CNS, particularly in the brain, they can also affect the spinal cord and other areas of the body. Cavernomas are quite common but rarely symptomatic, it is thought that they can affect 1 in 200 people but only about one in 10 will develop symptoms (3).
A symptomatic cavernoma can present with a wide variety of mainly neurological symptoms some of which include headaches, focal neurological deficits, seizures, and hemorrhage or it can even be discovered incidentally (that is, while looking for another anomaly). The most common finding was found to be seizures though (4). Cavernomas represent 15% of cerebrovascular malformations. Cavernomas are usually associated with other vascular malformations, most notably venous malformations.
The incidence rate of cavernomas was found to be 0.15-0.56 per 100 000 persons per year. The annual hemorrhage rate was found to be between 0.6% and 11% per patient per year (5).
Pathology
Cavernomas are abnormal vascular structures made up of bubble-like cavities termed Caverns. Venous blood flows through them. Their walls are thin and can leak blood. They range from being microscopic to being several inches in diameter. The cause is often unknown although up to 20% are familial in origin (6). Cavernomas are often described to look like a berry. The enlarged closely packed vessels of cavernomas have no interposition of the brain parenchyma and are usually surrounded by hemosiderin and gliosis. The cause of cavernomas is unknown although 20% of cases are familial in origin (6). The remaining 80% are sporadic. The inheritance pattern of familial cases is autosomal dominant with incomplete penetrance. Lesions in the brain are divided based on their location relative to the tentorium cerebelli into supra and infratentorial lesions. Brainstem cavernomas are infratentorial. Approximately 70% of cases are supratentorial and 30% are infratentorial, particularly in the brainstem (7).
Diagnosis
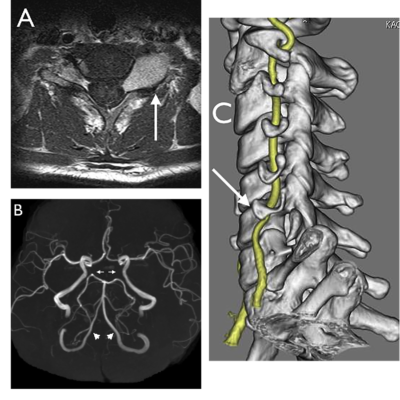
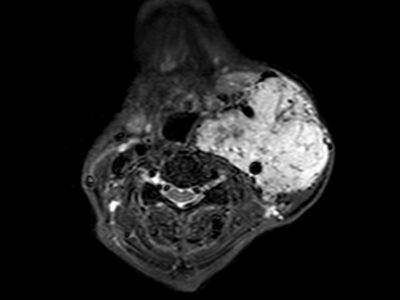
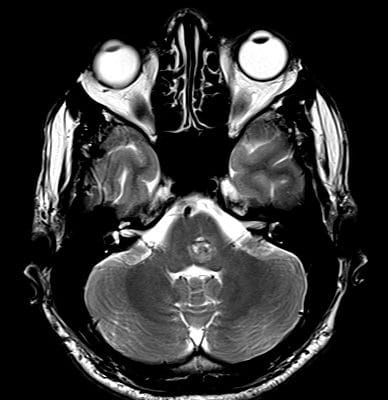
The diagnostic modality of choice is the MRI while the CT scan lacks specificity when compared to the MRI (8). On MRI cavernomas appear as well-circumscribed (it is demarcated by a layer of signal loss owing to it being surrounded by a layer of hemosiderin) popcorn-like lesions that have multiple foci with different signal intensities. The variation in signal intensity is due to them representing bleeding at different stages of evolution (9). Cavernomas are usually not associated with edema or mass effect. Figure (1)
Different MRI sequences used and the results they give:
- T1:
- Varied signal intensity depends on the age of the blood products, small fluid-fluid levels may be present. Figure (2)
- T2
- Hypointense rim is visible
- Varied signal intensity depending on the age of blood products
- If a recent bleed has occurred, edema surrounding the lesion may be present
- GRE T2*/SWI
- Shows prominent blooming
- Can be used for detecting smaller lesions that would otherwise be missed by conventional spin echo sequences, particularly in patients with familial or multiple cavernous malformations
- T1 C+ (Gd): using gadolinium contrast usually shows no enhancement
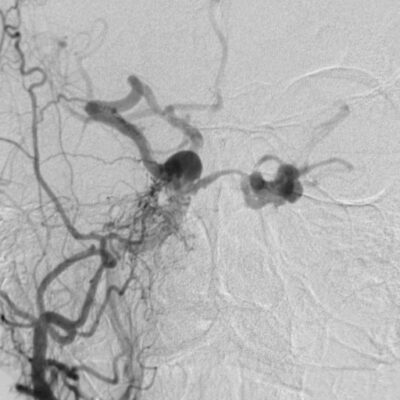
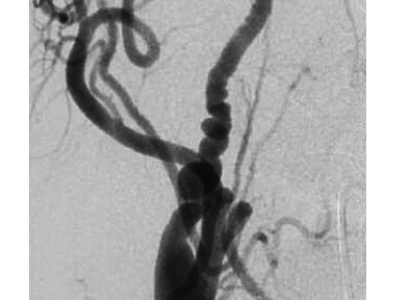
It is important to note that angiography is usually not the preferred method to diagnose cavernomas since they are angiographically occult due to the low speed at which blood flows through them (4). Angiography (digital subtraction angiography) does play a role however in differentiating between a cavernoma and an arteriovenous malformation (10).
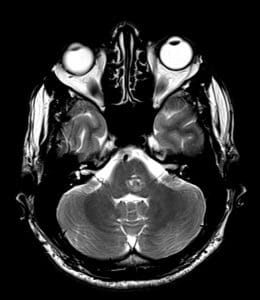
Figure (2): Axial T2, Evidence of well-demarcated rounded lesion at the pontomedullary junction, on the posterior medial aspect. (13)
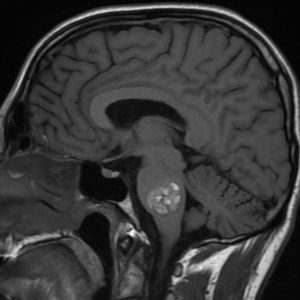
Figure (2): Sagittal T1, Large pontine cavernous malformation demonstrating fluid-fluid levels and surrounding edema in keeping with episodic hemorrhage. (14)
Treatment
In 1928 Walter Dandy was the first to operate on a pontine brain stem cavernoma. This was of course found after operating on the patient since diagnostic modalities weren’t advanced enough back then to diagnose such a lesion (1).
Treatment options include following the lesion up over time, and surgical removal which is an option reserved for lesions causing significant symptoms interfering with the patient’s life. Surgical removal is relatively simple due to the lesion being surrounded by a layer of gliosis which naturally demarcates it. The risk of bleeding is also lower due to the lower speeds at which blood flows through these lesions further simplifying their resection. Brainstem cavernomas however have an eloquent location owing to the vitality and importance of the brainstem which renders these lesions technically difficult to resect.
Indications for surgery include a single hemorrhage when it is not located in an eloquent area, intractable epilepsy, progressive neurological deficit, multiple hemorrhages when it is located in eloquent areas, severe symptoms such as cardiac or respiratory instability, and the presence of a cavernoma within 2 mm from the pial surface. The following situations might also be indications of surgery in brainstem cavernomas (8,11):
- Patients are treated with steroids to limit the edema.
- Progressive neurological deficits caused by recurrent bleeding
- In case developmental venous anomalies (DVA) associated with the cavernoma are present, resection is usually avoided due to the risk of venous infarction that is caused by resecting the DVA.
- Exsanguinated blood is seeping into brain tissue surrounding the angioma. This includes acute or subacute bleeding visible on MRI whether inside or outside the cavernoma and which is causing mass effect.
- The cavernous angioma is causing considerable compression of surrounding tissue (visible compression)
- The lesion is in contact with the brain stem surface
- Stereotactic radiosurgery can be considered in patients with surgically inaccessible lesions. However, studies have reported a high risk of complications such as recurrence of hemorrhage, permanent neurological deficits, and radiation-induced adverse effects.
- In cases where aborting further bleeding or the development of seizures is required, resection is warranted. Postoperative MRI within 72 hours of the operation to detect any rebleeding is needed.
- Coma, respiratory or cardiac instability as clinical presentations of cavernomas are not considered surgical contraindications due to the fact that emergent surgical evacuation might achieve satisfactory outcomes in relieving these grave symptoms.
- Stable lesions (not growing) that have not reached the brain stem surface causing minimum neurological manifestations ought not to be operated on but rather followed up conservatively.
Cavernomas in the brainstem is in an eloquent position, the slightest increase in size or bleeding (which increases size indirectly) can press on important nerves or nuclei and cause severe symptoms, this risk should be balanced by the risks associated with the intricate surgery that would be performed to remove such lesions. It is also worth noting that repeated hemorrhages worsen the neurological deficits which in turn affects the clinical picture of the patient, furthermore surgically removing the lesion after such repeated hemorrhage will also become technically more difficult (11).
Resecting brainstem cavernomas can be achieved by using one of the four standard skull-base approaches, and those are retrosigmoid suboccipital (with or without telovelar approach), supracerebellar infratentorial, orbitozygomatic, and far lateral (12).