Article topic: Bow Hunter Syndrome
Author: Hashem Bani Ata, Omar Alqudah
Editor: Sadeen Eid
Reviewer: Ethar Hazaimeh
Keywords: vertebrobasilar, compression, head rotation, doppler, dizziness, osteophytes, cervical, decompression.
Introduction
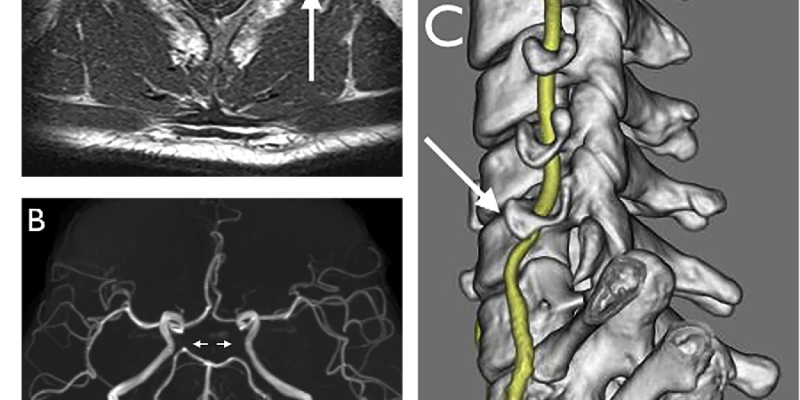
Bow hunter syndrome is a rare condition of transient vertebrobasilar symptoms as a result of reversible vertebrobasilar insufficiency caused by mechanical compression of the vertebral artery triggered by head rotation1. Symptoms include dizziness, visual abnormalities, vertigo, and syncope that improve when the head comes back1. Osteophytic compression is thought to be the most common etiology2. Diagnosis is made by doppler sonography, CTA, and MRA. Treatment could be conservative, or surgical such as; cervical decompression, cervical spine fusion, and stent placement3. The name Bow Hunter’s Syndrome came from the the position of bow hunter’s head when they aim their bow4.In 1978, the first scientific literature was established about bow hunter syndrome by Sorensen5.
Epidemiology
Bow hunter syndrome is more common in males than females, typically in (5-7) the decade of life with a mean age of 53 years old, but it can present in any age group. Also, many comorbidities increase the risk of bow hunter syndromes such as diabetes, hyperlipidemia, hypertension, and coronary artery disease, as noticed in many case reports that a patient has two or more from the previous comorbidities6.
Etiologies and Pathogenesis
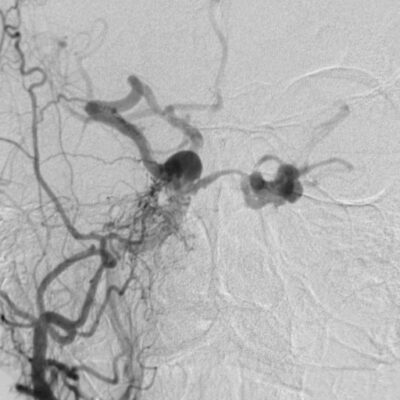
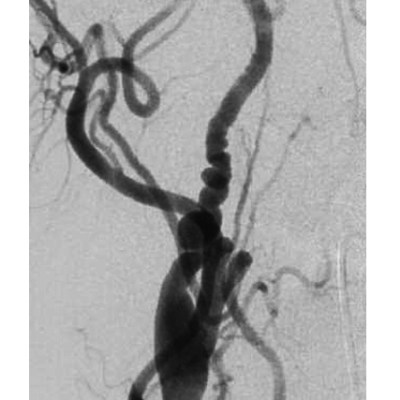
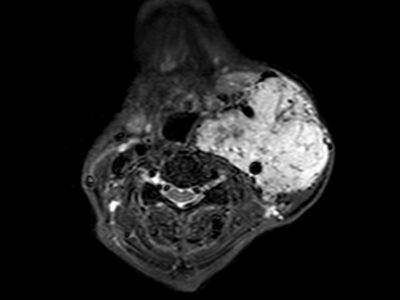
Many etiologies for bow hunter syndrome are recorded in many case reports however, every cause compresses the vertebral artery by certain mechanisms, compressive agents could be bone, ligament, disc7, and muscle8. The most common etiology is osteophyte9. Spondylosis causes vertebral compression by overgrowth10. Also, hypertrophy of neck muscles8, ligament disc7, atlantoaxial hypermobility4, and, thyroid cartilage impingement5. Rare causes for bow hunter syndrome could be vascular, such as aneurysm, vertebral artery hypoplasia, vertebral artery dissection, atherosclerosis, or embolism5.
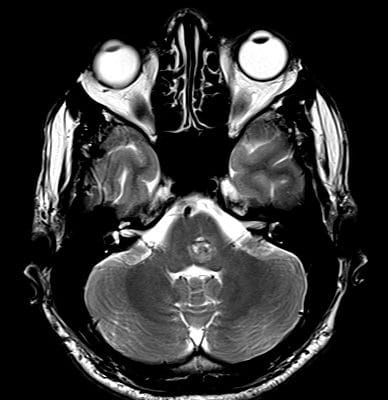
Pathogenesis of bow hunter syndrome is depending on the compression of the vertebral artery, and the most common locations of compression are C1-2 and C5-C7 because of the hypermobility for these locations. Narrowing of the vertebral artery during head rotation is physiologic due to stretching, what happens in bow hunter syndrome is there is an offending agent such as osteophyte that exacerbates narrowing and stretching7.
Clinical features
Bow hunter syndrome manifests with transient symptoms that are relieved when the head return to the neutral position and the angles at which symptoms are provoked are 30,45,60,80 and 90. The classic presentation of bow hunter is vertigo, dizziness, and nausea, but it can manifest with posterior circulation stroke6. These symptoms are illustrated with their prevalence in the table below3:
| Symptom | Prevalence |
| Vertigo | 28% |
| Syncope | 26% |
| Lightheadedness
Dizziness |
11% |
| Nausea/vomiting | 10% |
| Visual symptoms | 8% |
| Tinnitus | 7% |
| Focal neurological deficits | 5% |
| Other symptoms | 5% |
Diagnosis
Comprehensive history and physical examination are the first step in the diagnosis of bow hunter syndrome and need high suspicion because of its rarity, after that, Imaging confirms the diagnosis11. Regardless of the technique employed to diagnose bow hunter syndrome, two positions are needed; one when the head is neutral to show the patent artery, and one when the head is rotated to show the compressed or stenotic artery. The diagnosis may involve a variety of techniques. The gold standard modality is digital subtraction angiography (DSA). Other techniques like computed tomography and angiography, magnetic resonance imaging, and angiography, are also option.6.DSA overweight CTA and MRA by its accuracy and quickness during the evaluation of the flow through the vertebral artery as the symptoms develop after seconds of head rotation. Also, the risk of posterior circulation infarction is increase with CTA and MRA. In contrast, CTA provides details about an offending agent and its effect on vascularity6.
Other modalities are used such as transcranial Doppler (TSD) sonography; which confirms lesion the effectiveness of treatment and is used widely because it is considered safe and non-invasive at a lower cost. Cerebral blood flow scintigraphy, single-photon emission CT scanning, and Electrophysiological examinations are also used6.
The accuracy of all modalities above in the diagnosis of bow hunter syndrome is recorded in table below11:
| Modality | Accuracy |
| Dynamic angiography | 100% |
| Ultrasound | 36.4% |
| CTA | 18.2% |
| MRA | 18.2% |
Treatment
There is no ideal management for bow hunter syndrome, and multiple management is available; conservative, surgery, and endovascular intervention. Depending on the desire of the patient and complications for each procedure, the decision will be5,6.
Conservative therapy
This option includes explaining to the patient how to prevent eliciting symptoms by avoiding head rotation using a neck collar and also using antiplatelet and anticoagulant drugs such as aspirin and warfarin. According to that this therapy avoids patient invasive procedures with variable complications, it can be considered a first-line treatment. The effectiveness of this therapy is variable from patient to patient, so some patients don’t improve with this treatment and need another management5,6.
Surgical treatment
Surgical decompression and cervical spine fusion are two possible surgical techniques, each one has its indication depending on the advantages and disadvantages, offending agent, and patient conditions. Sometimes a surgery called decompression with effusion combines two operations5,6.
Surgical decompression involves the removal of bone elements such as the transverse process that surround the vertebral artery. So, decompression doesn’t affect on motion range of the head, and that makes it overweighs fusion which restricts head movements. The disadvantages of decompression are represented by the fact of removing the protective agent of the vertebral artery from adhesion with surrounding structures which increases the risk of restenosis; because in this procedure, some bony structures such as the transverse process and groove of the atlas are removed, which prevent adhesions.
Although decompression makes patients return to their daily living activities, they are at risk of recurrence, and some patients develop postoperative posterior circulation infarction, so some patients need fusion later. Depending on where the disease is, there are two ways to accomplish surgical decompression: an anterior approach and a posterior approach. The anterior approach is performed for lower cervical spine pathology and the posterior approach is for upper cervical spine5,6.
Cervical spine fusion is adopting restricted neck motion to prevent vascular compression. Movement restriction is performed by bone graft fixed between the lamina of the axis and the posterior arch of the atlas. The risk of restenosis in this procedure is less than vascular decompression, but the problem is in head motion restriction and its reflect in daily living activities5,6.
Endovascular procedure
In this procedure, a coil or stent is used in cases of atherosclerosis, aneurysms, or malformations. The effectiveness of this procedure isn’t known until now6.