Article Title: Schizotypal Personality Disorder
Author Name: Pesan Sabatieen
Editor: Sama Abd-Alkareem, Yara Alswaiti.
Reviewer: Ethar Hazaimeh
Keywords: Eccentric behavior, Cognitive Distortions, Social anxiety, Paranoia.
Introduction
Schizotypal personality disorder is a rare condition characterized by impaired social and interpersonal skills, eccentric behavior, and cognitive or perceptual anomalies. [1] It was not included in the DSM-III until 1980, and was previously used to describe a wider variety of illnesses, known as “nonpsychotic schizophrenia-type illness.” The rarity of schizotypal personality disorder remains unclear [2].
This problem has a significant influence on day-to-day functioning and other mental disorders. Individuals with SPD may also experience frequent dissociative episodes, further exacerbating their difficulties. [3]. People who suffer from schizotypal personality disorder may experience dissociative episodes on a regular basis, which make the problem worse. indicating that this illness requires further attention. [4]
To individuals with high levels of schizotypy may have difficulty in understanding the emotions of others when encountering complicated everyday social scenarios, which may further lead to negative experiences in social interactions and impede their day‐to‐day interpersonal communication [5]
Abstract
(SPD) is a persistent personality disorder expressed as a less severe manifestation of schizophrenia-spectrum psychopathology disorder [6]. SPD is often misdiagnosed due to its resemblance to other psychiatric disorders, making accurate diagnosis challenging [7]. The disorder being linked to schizophrenia can give us a better understanding of any genetic overlap, the pathogenesis of the disorder, and treating any related mental illnesses [8].
Keywords: Eccentric behavior, Cognitive Distortions, Social anxiety, Paranoia.
Epidemiology and Risk Factors
The prevalence of SPD is not considered high, estimated to be only 4% in the US, with a slightly higher percentage for men (4.2%) than women (3.7%) [8].
The likelihood increases if the person has the following risk factors :
- Went through divorce, separation, widowhood, or developed a low income . [7]
- Associated with several mental illnesses such as BPD, PTSD, and bipolar I and II disorders [8].
- Peer victimization is considered a risk factor among adults who were victimized between the ages of 8 to 16 years in the forms of verbal and physical harassment. Social manipulation and attacks were associated with SPD, directly linked to social anxiety and the lack of close friends [9], Additionally, regardless of the diagnosis of psychotic disease, exposure to childhood trauma is linked to an increase in schizotypal traits (particularly paranoid ideation) and sophisticated social cognitive abilities[10].
- A major risk factor is genetics. There is a correlation between the p250GAP gene and SPD; the genetic variation in this specific gene increases susceptibility to SPD [11]. Another gene, CACNA1C, responsible for memory and brain functioning, has the variation rs1006737, which is directly associated with the risk of SPD, affecting brain activity, psychosis, and emotional processing [12].
Clinical Features
Patients with SPD exhibit more disordered speech and ideas than those with other personality disorders, along with a decreased sense of reality [13]One classification for SPD is schizophrenia spectrum disorder [13]. Suicidal ideation (SI) and behavior have also been linked to SPD [14].
Digital environments may also contribute to the development of schizotypal immersion, a personality trait that influences how individuals with SPD engage in virtual and online spaces. [14]. A study involving 717 college students found that focusing abilities are linked to self-coherence and problematic internet usage, affecting SPD patients more than others [15].
Suicidal Acts and Linked Behaviors
A study in the US found that a diagnosis of depression in SPD patients predicts lifetime suicide attempts [16]. Schizotypal characteristics in adolescence can also predict suicide attempts between 18 and 38 [17].
Joiner and Rudd (2002) found that symptoms of SPD were linked to suicidality in a large cohort of young adults referred to a high-risk suicide treatment program. The study examined the association between personality traits and suicidal behavior in 87 Japanese patients with schizophrenia and 322 controls. Results showed that all SPQ (schizotypal personality questionnaire) indices were significantly higher in patients with schizophrenia (SA + nSA groups) than in controls, highlighting the importance of understanding schizotypal personality traits in determining suicidal behavior [18]
Numerous research have connected SPD and schizotypal traits to suicidal thinking and conduct. The reason for this is :
Because SPD is challenging to treat, misdiagnosis happens frequently. Lack of established protocols for suicide screening or therapies for individuals with SPD impedes efforts to prevent suicide.
Suicide prevention for those with SPD involves three steps :
- Identifying SPD.
- Treating SPD appropriately.
- Offering suicide prevention and screening [19].
DSM Classification
In order to diagnose illnesses like schizophrenia and depression, medical experts use the DSM-5, a diagnostic guideline for mental health disorders that includes personality disorders.
The DSM-5 lists schizotypal personality disorder (SPD) as a Cluster A personality disorder. Cluster A personality disorders are characterized by peculiar or quirky circumstances. Because protective factors mitigate subcortical DA hyperactivity, people with SPD are also less likely to experience psychosis.
As a schizophrenia spectrum disorder, SPD is included in both the personality disorder and psychosis sections of the DSM-5 due to its demonstrated close link to other schizophrenic disorders [20].
The Five-Factor Model
The Big Five, often known as the Five-Factor Model (FFM), represent five broad categories of normal personality traits: neuroticism, agreeableness, extraversion, conscientiousness, and openness. It is employed to comprehend general personality.
The study on the five-factor personality dimensions in individuals with schizotypal personality disorder (SPD) found inconsistent results, particularly in terms of openness. Results showed that individuals with SPD had higher levels of neuroticism and lower levels of extraversion, agreeableness, and conscientiousness. Female SPD subjects exhibited higher openness levels than healthy individuals, suggesting gender-associated differences in openness. This underscores the need for future studies to examine gender effects in SPD [21].
The Best Approach to Deal with SPD
Identifying SPD through common factors such as trauma or maltreatment history, particularly childhood neglect, is crucial, as these individuals often exhibit higher levels of schizotypal personality disorder symptoms, along with other factors like depression and dissociation [7].
Recognition of SPD allows us to offer suitable therapeutic methods, such as providing suicide prevention and screening services. Interventions aimed at reducing depressive symptoms, enhancing self-worth, and developing social skills may be effective in lowering the risk of suicide in people with SPD. [22]
Research on suicidality in individuals with SPD is necessary and could become a significant area of study in suicide prevention. Future research on the pathophysiology of suicidality in SPD is expected to contribute to the development of techniques for suicide prevention treatments and screening in these individuals. [22]
Clinical studies revealed findings that are unique in the research, omega-3 fatty acids may help lessen schizotypal personality in kids who live in the community. If confirmed and expanded, these findings may have epidemiological implications for early avoidance of more substantial schizotypal traits that emerge later in adolescence [23].
Eriksonian stage
Young adulthood is a common time for the development of personality disorders. Using development theory concepts like Eriksonian phases might help us better grasp the patient’s difficulties. A person would be going through the Eriksonian stage of “identity versus confusion” during adolescence; the formation of a complex inner world with several identities would support the patient’s sense of self in spite of social difficulties [24].
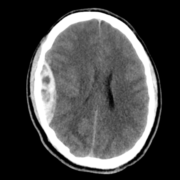
Neuroimaging Findings
Neuroimaging studies have found that individuals with SPD exhibit reduced gray matter volume in the left superior temporal gyrus (STG) and greater parahippocampal asymmetry compared to controls. While SPD and schizophrenia share some similarities in STG structure, individuals with schizophrenia show additional reductions in hippocampal and amygdala volumes, particularly in the left hemisphere. These findings suggest potential neural distinctions between SPD and schizophrenia.
Conclusion
Finally, this article has shed light on schizotypal personality disorder, elucidating its definition, presentation, diagnosis methodology, and course of treatment. By outlining the DSM-5’s diagnostic criteria, medical professionals can more accurately diagnose and distinguish schizotypal personality disorder from other personality disorders. Efficient approaches to management, such as behavioral therapies and medication-assisted treatment for underlying causes, are essential in lessening the burden of this condition on everyday life. In order to improve outcomes for persons impacted by SPD, we anticipate that research will continue to expand and that cooperative efforts will be made to create focused treatments and better diagnostic methods.