Article topic: Dystonia
Author: Amr Atef Hassan
Editor: Ahmad Abuaisheh, Rahmeh Abdullah
Reviewer: Ethar Hazaimeh
Keywords: Dystonia, Etiology, Wilson’s disease, Botulinum toxin
Abstract
Dystonia is a neurological disorder that manifests as abnormal, involuntary movements or positions due to ongoing or intermittent muscle contractions. In a recent consensus, dystonia is now classified into two axes to define its clinical features and underlying causes. This classification system enables accurate recognition of both isolated and combined forms of dystonia while still incorporating the descriptions of generalized and focal dystonia, which prove valuable in planning investigations and treatment strategies. This article explores the characterization of dystonia for improved identification and provides a concise overview of its management. Treatment options for dystonia encompass medications, botulinum toxin, and deep brain stimulation.
Overview
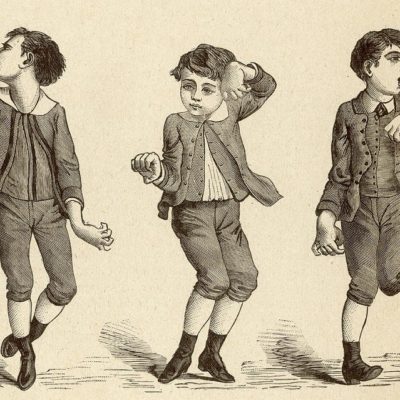
Dystonia is recognized as the third most prevalent movement disorder, following Parkinson’s disease and essential tremor (1). A definition for dystonia was established by a committee of the Dystonia Medical Research Foundation’s Scientific Advisory Board in February 1984, which remained valid until 2013 when an international committee developed a new concept (2). This neurological disorder is characterized by abnormal and involuntary muscle contractions, leading to sustained abnormal postures, twisting, or both, as well as repetitive movements of body parts (3).
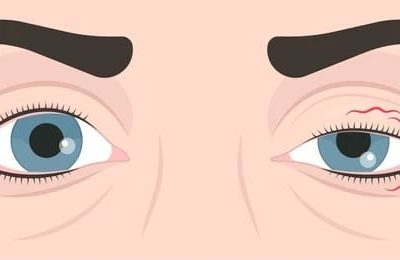
Dystonia can be a significant or presenting feature in many neurodegenerative diseases (4). In most cases, dystonia is a combination of abnormal movements and postures. However, some types, such as blepharospasm and laryngeal dystonia, are not associated with postures but instead involve focal involuntary contractions that interfere with the physiological opening or closing of the eyelids or larynx (5). Dystonia may occur alone or in combination with other clinical issues (6).
The prevalence of dystonia has been reported to be around 164 per million, with focal cervical dystonia [CD] being the most common type (7). Prevalence estimates also depend on age, with early-onset dystonia (<20 years) estimated to be between 0.3 and 5 cases per 100,000, while adult-onset (>20 years) dystonia is between 0.3 and 732 cases per 100,000 (8). The aim of this article is to shed light on dystonia, with a focus on its definition, etiology, clinical classification, and management.
Etiology
Over the years, the genetics of dystonia have been extensively studied, resulting in the identification of a multitude of genes that can cause this movement disorder (9). Despite the advancements in our understanding of dystonia’s etiology, the underlying cause of most forms remains unclear (table 1). As new clinical, genetic, and basic science information emerges, the classification of dystonia based on etiology will need to be continually updated (1).
| Nervous system pathology | Inherited | Acquired | Unknown |
| Nervous system pathology with degeneration (or heredodegenerative) |
Autosomal dominant
|
Perinatal brain injury
|
Sporadic |
| Neurodegeneration with brain iron accumulation |
Autosomal recessive
|
Infection/ inflammation
|
Familial |
| Wilson’s disease
|
X-linked Recessive Exposure to a neurotoxic agent
|
Toxic | |
| Mitochondrial | Drug | ||
| Vascular | |||
| Brain injury | |||
| Neoplastic | |||
| Functional |
Table (1): The etiology of dystonia (1,10)
Inherited dystonia
Inherited forms of dystonia are confirmed to have a genetic basis and can be further divided into multiple subgroups based on their pattern of inheritance (1):
Autosomal dominant dystonia encompasses several forms, including DYT-TOR1A, DYT/PARK-GCH1, DYT-THAP1, DYT-SGCE, and DYT/PARK-ATP1A3.
Autosomal recessive dystonia includes several forms, such as DYT-ATP7B (also known as Wilson disease), NBIA/DYT-PANK2 (pantothenate kinase-associated neurodegeneration), NBIA/DYT/PARKa-PLA2G6 (PLA2G6-associated neurodegeneration), and multiple metabolic disorders.
X-linked recessive dystonia consists of disorders such as DYT/PARK-TAF1, DYT/CHOR-HPRT (Lesch-Nyhan syndrome), and DYT-TIMM8A (Mohr-Tranebjaerg syndrome).
Mitochondrial dystonia is caused by mutations in the mitochondrial genome and includes forms such as Leigh syndrome or DYT-mt-ND6 (Leber optic atrophy and dystonia). It is worth noting that a significant number of recessive forms (autosomal and X-linked) and mitochondrial forms are classified as complex dystonia forms, while all isolated dystonias with a known genetic cause are inherited in an autosomal dominant fashion.
Nervous system pathology
Dystonia can be caused by various inherited degenerative diseases, including autosomal-dominant and autosomal-recessive conditions, X-linked dominant and recessive conditions, and mitochondrial defects. The neurodegenerative process can manifest in additional symptoms and signs, and dystonia may be observed.
Wilson’s disease is a common cause of dystonia and can present as generalized, segmental, or multifocal dystonia, with cranial involvement being characteristic. Other common signs include the “sardonic” smile, wing-beating tremor, dysarthria, dysphagia, drooling, ataxia, and dementia. The disease can affect the brain, liver (cirrhosis, acute hepatitis), eyes (Keyser-Fleischer rings), heart, kidneys, bones, joints, glands, and muscles. As the condition is potentially treatable, it should be considered when observing any patient with movement disorders (10).
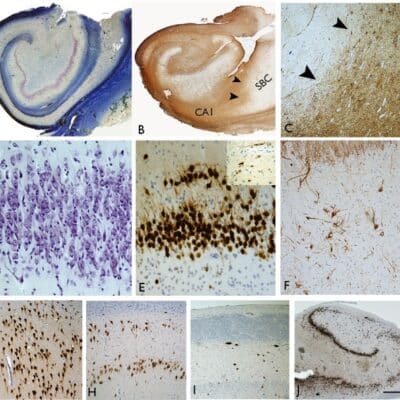
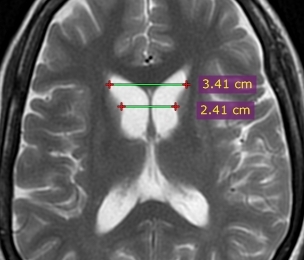
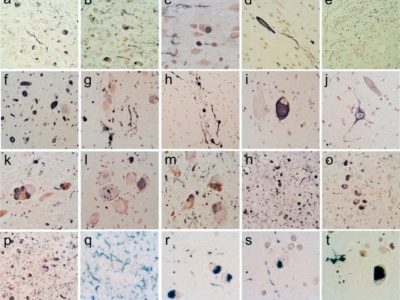
The pathologic changes in Wilson’s disease are typically observed in central gray matter nuclei and white matter tracts in the brainstem, with the underlying cause of the high susceptibility of these brain regions to copper toxicity unknown (11,12). Most severe abnormalities are present in the putamen, which is typically shrunken, soft, and brown-yellowish discolored. In severe cases, putaminal necrosis with iron-laden macrophages surrounding the necrotic cavity may occur (13), and cavitation can be rarely found in the thalamus, dentate nucleus, or white matter (14,15).
Cellular alterations have been identified in specific forms of dystonia, such as neuronal inclusions in brainstem nuclei in patients with DYT-TOR1A, indicating abnormalities on the cellular level. These findings require further replication and extension, as is true for another line of research linking dystonia to cerebellar dysfunction based on Purkinje cell loss and axonal swelling in the cerebellum of patients suffering from cervical dystonia (1).
Acquired dystonia
Acquired dystonia can occur secondary to a precipitating event. About half of the children with dystonia have an acquired cause for their condition, which can include hypoxic brain injury at birth, preterm delivery, and kernicterus. The timing of dystonia onset can vary after a causal event. For example, in drug-induced dystonia, acute reactions can be seen hours after the administration of antidopaminergic medications (e.g., metoclopramide, and prochlorperazine). One of the most common presentations is an oculogyric crisis, where the patient has an upward, conjugate, tonic deviation of the eye (16). Other causes of acquired dystonia can include perinatal injury, stroke, head trauma or peripheral trauma, brain tumor, exposure to neurotoxic agents, Japanese B encephalitis, encephalitis lethargica, brain abscesses (mostly involving the basal ganglia), cerebellum, and thalamus (10).
Functional dystonia should be considered in patients with dystonia who display atypical patterns of muscle movement, fixed dystonia, or experience a reduction in symptoms when distracted. This condition is often understood through a biopsychosocial framework that takes into account factors that contribute to abnormal brain processing of sensory and motor signaling. Identifying functional dystonia and providing a mechanistic explanation for the patient’s symptoms can lead to significant improvement in their condition. It is important to note that functional dystonia should not be excluded as a diagnosis, and should be actively considered alongside other possible causes of dystonia.
Unknown dystonia
Dystonia can be categorized as either sporadic or familial, with the latter indicating a possible genetic contribution. The identification of new dystonia-related genes, including GNAL, ANO3, KCTD17, and KMT2B, has allowed these subtypes to be classified as inherited forms of dystonia (1).
Classification of dystonia
Once a movement disorder is identified as dystonic in nature, it should be further characterized according to the current classification system, which was established by the Movement Disorder Society in 2013 (17).
This classification system includes Axis I Clinical Characteristics and Axis II Etiology. Clinical characteristics of dystonia include age of onset, body distribution, and temporal pattern, as shown in Table (2). Associated features include whether the dystonia is isolated or combined with another movement disorder and any accompanying neurological or systemic symptoms(18).
| Age at onset | Body distribution | Temporal pattern |
Associated features
|
| Infancy
(birth to 2 years)
|
Focal | Disease course: – Static
– Progressive
|
Isolated (no other
feature)
|
| Childhood (3-12 years) | Multifocal | Variability :
1- Persistent 2- Paroxysmal 3- Diurnal 4- Action- specific |
Combined (+ Another
movement disorder)
|
| Adolescence (13-20 years)
|
Segmental | Complex (+ other manifestation,
may include non-neurological)
|
|
| Early adulthood
(21-40 years) |
Generalized
+/- leg involvement |
||
| Late adulthood
(>40 years) |
Hemidystonia |
Table (2): Clinical characteristics of dystonia. (1)
Age at onset
According to research, dystonia that begins in childhood is more likely to have an identifiable acquired cause and may progress from focal to generalized, while typical adult-onset focal dystonia is more likely to be a subtype of isolated dystonia and usually does not spread (19). This classification follows established neurological disorder classifications and informs prognosis and diagnosis (17).
Childhood dystonia is a heterogeneous condition in terms of its clinical presentation and genetics. Emerging evidence indicates that mutations in genes associated with neurodevelopmental disorders may play a role in the development of dystonia that appears early in life (20).
Body distribution
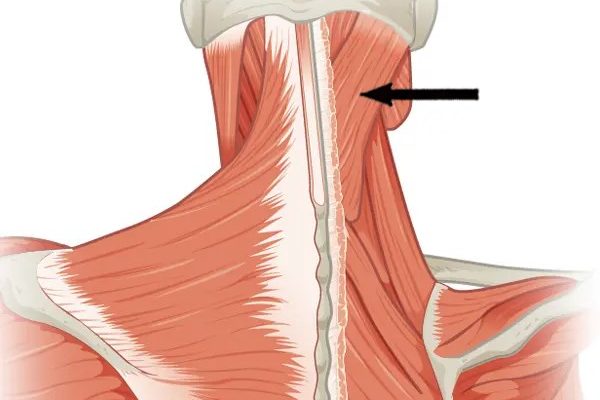
Dystonic signs can occur in any part of the body, but commonly affect the cranial and cervical regions, larynx, trunk, and limbs, either individually or in combination (1). Dystonia can be categorized based on how it affects different parts of the body, including:
- Focal dystonia, which affects only one specific region of the body.
- Segmental dystonia, which affects two or more adjacent regions of the body.
- Multifocal dystonia, which affects two or more non-adjacent regions of the body.
- Hemidystonia, which affects one-half of the body.
- Generalized dystonia, which affects the trunk and at least three other areas of the body.
Temporal pattern
The time course of the disease is a crucial clinical feature that aids in diagnosis and treatment decisions. The disease course distinguishes static forms from progressive forms and is an essential temporal characteristic (5). This terminology is commonly used by pediatric neurologists, but it is also applicable to adult cases.
Diurnal variability is used to differentiate dystonia that consistently occurs under the same conditions from variable forms, including task-specific, action-specific, and spontaneous dystonia.
Paroxysmal dystonia is distinct from dystonia which is always triggered by the same action or activity (task-specific dystonia). In paroxysmal dystonia, the same trigger may or may not cause an attack, while in action dystonia, the same motor activity will predictably induce dystonia (5).
Paroxysmal dystonia typically lasts after the trigger has ended, whereas action (or task-specific) dystonia is only present during the inducing action.
Dystonia variability can have four different patterns:
- Persistent dystonia, which persists to approximately the same extent throughout the day.
- Diurnal fluctuations, where dystonia varies during the day and has recognizable circadian variations in occurrence, severity, and phenomenology.
- Paroxysmal dystonia, a sudden self-limited episode of dystonia typically induced by a trigger with a return to the pre-existing neurological condition.
- Action-specific dystonia, which only occurs during a particular activity or task.
Associated features
Associated features are divided into:
- Isolated dystonia
- Combined dystonia
- Complex dystonia
According to research (1), various syndromes may arise from dystonia, including isolated dystonia or dystonia combined with myoclonus, parkinsonism, or other movement disorders. The term “primary” was coined to describe syndromes in which dystonia is the only phenotypic manifestation (with or without dystonic tremor).
Primary dystonia is characterized by dystonia being the sole clinical sign, and typically, there are no identifiable secondary causes or consistently associated brain pathology. Dystonia can emerge at any age, and age at onset is an important variable that affects clinical presentation and prognosis. Some cases of isolated dystonia have a genetic basis, with three genes currently known to cause the condition: TOR1A, THAP1, and GNAL. Additionally, three other genes (CIZ1, ANO3, and TUBB4) have recently been implicated and require further confirmation (22).
Combined dystonia, on the other hand, refers to cases in which dystonia is combined with other movement disorders, such as myoclonus or parkinsonism (5).
Diagnosis of dystonia
Currently, the diagnosis of dystonia is primarily based on physical examination and pattern recognition by an experienced clinician. This can be challenging due to the wide range of dystonia phenotypes and etiologies, as well as dystonia mimics like functional dystonia. Dystonia can present with different characteristics, including as the only symptom or part of a mixed neurological or systemic disorder. Childhood-onset dystonias can be particularly difficult to classify both etiologically and clinically (23).
Patients with isolated dystonia may require a laboratory workup depending on their age at onset, body distribution, and the presence of affected family members. Adults with focal or segmental dystonia may not require any diagnostic tests as they are often unrevealing. However, in adults with hemidystonia or generalized dystonia, neuroimaging may be useful as there is a higher likelihood of finding a structural cause.
Genetic testing may not be cost-effective for sporadic adult-onset isolated dystonias unless other family members are affected. Younger individuals with isolated dystonia require a different diagnostic approach as there is a higher likelihood of finding a cause. Neuroimaging is important for all early-onset cases, and genetic testing should target specific genes for early-onset isolated dystonias (6).
For patients with combined dystonia, an additional workup is warranted regardless of age at onset or body distribution, depending on the nature of associated features. Neuroimaging is useful in virtually all combined dystonias, as it can provide important diagnostic clues. Genetic testing for DYT1 and DYT6 dystonia is not useful in combined dystonia syndromes, but laboratory testing is driven by the syndromic pattern. For example, dystonia combined with Parkinsonism may lead to a relatively small list of disorders for more targeted diagnostic testing (6).
Management of dystonia
Patients with suspected dystonia should be referred to a specialist in movement disorders for further evaluation and access to appropriate treatment. Blood tests, including a full blood count, urea and electrolytes, liver function tests, and caeruloplasmin, can be conducted at this stage. Brain imaging is often reserved for neurological review since imaging protocols are tailored to the patient’s clinical features. Treatment for dystonia depends on the underlying cause. In general, botulinum toxin injections are the first-line treatment for focal dystonia, while oral medications and surgery are used to treat generalized dystonia (20).
Treatment of dystonia
There are several treatment options available for dystonia, including counseling and education, oral medications, botulinum neurotoxin injections, physical and occupational therapy, and neurosurgical interventions (6).
Pharmacological treatments may involve dopaminergic, antidopaminergic, and anticholinergic therapies, baclofen, benzodiazepines, muscle relaxants, dopamine depleters, and other medications (24). Unfortunately, many patients require a combination of treatments, and a significant number of patients may not respond to medical treatment due to poor tolerability or lack of benefit, especially with high doses of anticholinergic drugs in adults (25).
Anticholinergic Medications
The class of drugs known as anticholinergics is often used to treat dystonia. The most commonly prescribed medication of this class is trihexyphenidyl, but other drugs like benztropine, ethopropazine, procyclidine, and biperiden have also been used. A small trial has even shown that diphenhydramine, which is a histamine H1 antagonist with anticholinergic properties, can be effective in treating dystonia. These drugs are believed to work by reducing the hyperactivity of cholinergic interneurons in the striatum. The choice of which drug to prescribe may depend on factors such as the patient’s individual symptoms and medical history (26).
Botulinum toxin (BoNT) is a commonly used first-line therapy for many dystonic syndromes, with a long track record of safety and efficacy (27). It is particularly effective in reducing hypertonia, but it does not improve strength or directly improve function (28). BoNT works by blocking the release of acetylcholine into the neuromuscular junction, causing local temporary chemodenervation and muscle paralysis (28). It is important to note that BoNT must be used carefully and in combination with an active program of other rehabilitation techniques, as it only improves function in cases where a few muscles are the major cause of disability (28). Large safety studies have shown that BoNT is safe and effective for clinical use, and its uses have expanded greatly over the past three decades. Dr. Alan Scott, an ophthalmologist, first described the effect of BoNT on extraocular movements in monkeys affected by strabismus in 1981 (27).
Benzodiazepines, such as clonazepam, are often used in dystonia, although their efficacy has not been evaluated in large, controlled studies. Open and retrospective studies have shown efficacy in treating generalized and focal dystonias, particularly in blepharospasm and cervical dystonia with predominant head tremors (29).
Deep brain stimulation (DBS) has become a major therapy option for movement disorders, including dystonia (30). GPi and subthalamic nucleus (STN) are the two main targets for DBS in dystonia treatment (31). Certain types of genetic dystonia, such as TOR1A, KMT2B, TAF1, and SGCE, typically have better responses to DBS than others, such as THAP1, ATP1A3, and GNAL (31).
Posteroventral pallidal deep brain stimulation (DBS) is a highly effective treatment for severe, medication-resistant generalized and segmental dystonias, as well as certain forms of focal dystonia. Studies have demonstrated long-term improvement in motor symptoms and activities of daily living, with average improvement rates ranging from 50 to 60% depending on various factors. However, as is the case with DBS for Parkinson’s disease and essential tremors, while symptoms are often significantly improved, they are rarely eliminated, highlighting the need for continued improvements in the technique (26).
Conclusion
Although dystonia is a common symptom, the number of neuropathologically studied cases of human dystonia remains limited. This can be attributed to several factors, including the rarity of dystonia being the direct cause of death, and cultural barriers in certain populations such as Ashkenazi and Amish peoples, who have a higher incidence of genetic dystonias like DYT1. However, advances in data collection on dystonia patients have allowed for large cross-sectional studies that can identify factors influencing the prevalence and clinical characteristics of dystonia, including tremors.
References:
References...