Article topic: Premenstrual Dysphoric Disorder (PMDD)
Authors: Mohammad Kamal Daradkeh, Ahed Fahmi Mohammad Daoud.
Editors: Mohammad Omari , Haneen A. Banihani, Ihda Mahmoud Bani Khalaf, Sadeen Eid
Reviewer: Ethar Hazaimeh
Overview
Premenstrual dysphoric disorder (PMDD) is a common mood disorder with distinct affective, cognitive, and physical symptoms affecting millions of women during their reproductive age [1]. According to DSM-5 criteria, these symptoms occur in the last week before menses and continue within 3-4 days after menses, confirmed by specific tools for a daily rating of symptoms for at least two menstrual cycles [1]. Despite sharing the cyclicity of psychological and physical symptoms that impair the patient’s social and occupational life, Premenstrual dysphoric disorder should be considered a separate entity from premenstrual syndrome (PMS) in aspects of hopelessness, tension, extreme moodiness, and marked irritability, as these severe affective symptoms lead the women with PMDD to seek medical help more than women with PMS [2]. Different studies showed an association between PMDD and decreased work productivity that leads to absence, adding to the economic burden of the disorder[3]. Interestingly, women with PMDD were at increased risk of reporting suicidal ideations, thoughts, plans, and attempts than PMS patients and the general population, although that didn’t implicate any significant suicide risk profile in terms of frequency and completion [4].
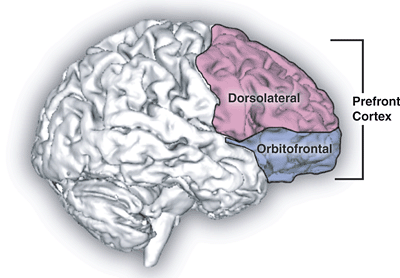
PMDD is characterized by at least five symptoms, mainly affective, that are present in the luteal phase of most menstrual cycles. In addition, behavioral and somatic symptoms can accompany the main affective symptoms, such as changes in appetite or food cravings, changes in sleep, loss of energy, or physical complaints (i.e., breast tenderness or bloating), which can overlap with other mood disorders. Yet, it is distinguished by its predictable cyclicity, confined to the premenstrual period[1]. It is thought that the altered sensitivity to the fluctuating serum levels of ovarian hormones that occur during the menstrual period, especially progesterone, in the brain-sensitive regions involved in top-down control and mesolimbic emotional processing, plays a role in the symptomatology of this disorder, according to some studies [5-7].
PMDD affects nearly 1.8 – 5.8 % of women of childbearing age. The incidence of new cases over a 40-month follow-up period is 2.5%. Onset can occur at any point after menarche. Many individuals, as they approach menopause, report worsening symptoms but cease after that, although cyclical hormone replacement can trigger the re-expression of symptoms [1].
Etiology and Pathogenesis
Recently, the etiology behind PMDD has been an active area of investigation and an important subject for randomized controlled clinical trials[8]. It can be divided into genetic, biological, environmental, or psychosocial factors. There are no studies examining the familial association based on DSM-5 criteria for PMDD because of the difficulty in obtaining prospective symptom reporting in a large sample of first-degree relatives of multiple generations[9]. However, the heritability of premenstrual symptoms can range from 35.1% to 56%, according to old studies[10,11].
Progestrone and Allopregnanolone
More substantial evidence for its pathogenesis was found by studying progesterone, its primary active metabolite, Allopregnanolone (ALLO) levels, and its effect on (GABA) A receptor function. ALLO is a positive modulator of the (GABA) A receptor with anxiolytic, anesthetic, and sedative properties like that of alcohol and benzodiazepines[12], so the rapid withdrawal of high serum levels of progesterone and ALLO at the end of the luteal phase may lead to upregulation of the receptor and may play a role in the anxiety and depressive-like behavior [13], [14]. Giving their (GABA) A sensitivity to progesterone and ALLO, especially in regions involved in aggression and cognitive control (i.e., angulate cingulate gyrus (ACC) and medial prefrontal cortex (mPFC)), PMDD patients randomized to selective progesterone receptor modulator (SPRM) treatment, which works by progesterone antagonism, had shown lower aggression scores and enhanced brain reactivity to negative stimuli compared with placebo group suggesting a beneficial role of progesterone antagonism and anovulation[6].
Given the CNS sensitivity of PMDD patients, the decline in the estrogen serum level in the luteal phase may add to the symptomatology of PMDD in terms of mood, cognition, sleep, eating, and other aspects [15], considering the possible estradiol-enhancing effects on the serotonergic system through increasing serotonin transporter mRNA expression[16], and decreasing monoamine oxidase A (MAOA) [17]. Moreover, patients with PMDD experience serotonergic abnormalities exacerbated in the luteal phase; one of them is the deficiency of the whole blood level of total serotonin 5-HT [18], adding evidence to the increased sensitivity to estrogen among patients with PMDD. One study found that single nucleotide polymorphisms in the estrogen receptor alpha (ESR1) gene were associated with an increased risk for PMDD [19].
Women with PMDD who are carriers of the Val66Met polymorphism of the Met allele of the brain-derived neurotrophic factor (BDNF) had lower front cingulate cortex activation during the luteal phase [20]; in addition, they had significantly higher serum BDNF levels, especially during luteal phase [21]. However, further investigation is needed as the obvious association is inconclusive despite the evidence of cyclicity across the menstrual cycle [22].
Immune System Dysregulation
Some evidence suggests the role of immune system dysregulation, as the luteal phase is associated with increased production of soluble interleukin 6 receptor (IL-6R) and increased expression of proinflammatory IL-6 and tumor necrosis factor alpha (TNF-A)[23,24]. C-reactive protein (CRP) level follows a cyclic pattern, as a tenfold increase in progesterone was associated with a 20-23% CRP increase [25,26].
The most relevant environmental factors associated with PMDD include stress, interpersonal trauma, seasonal allergies, and sociocultural aspects of female sexual behavior and gender roles [1]. Looking at the literature, the role of stress as an etiology of PMDD is controversial. Some studies found an association between traumatic history, physical and emotional abuse, and PMDD [27,28], but others demonstrated no increased risk compared with healthy counterparts [29]. The GABAergic sedative effect of ALLO promotes homeostasis during periods of acute stress[30], but the response becomes blunted with chronic stress [31], so administering exogenous ALLO may correct chronic stress-induced depressive and anxiety-like behaviors [32].
Estrogen
Estrogen plays a vital role in normal sexual and reproductive development in women. It comes in multiple forms, but the most important is estradiol, secreted in significant amounts by ovaries and small quantities by the adrenal cortex and pregnancy; it’s released from the placenta, too [17].
In some trials, they found that polymorphism in the alpha gene in estrogen receptor is associated with the risk of PMDD and demonstrated a low estradiol level among women with PMDD [8].
A study that tests the effect of alteration in hormonal levels among PMDD demonstrates an increase in the risk of mood symptoms among women whose estrogen is in a lower concentration, such as in the premenstrual phase, postpartum, and post-menopause.
Tamoxifen, a medication that suppresses estrogen function, contributes to depression’s pathophysiology. These results suggest that withdrawal from estrogen contributes to mood symptoms with PMDD [62].
Estrogen facilitates higher cognitive functions by affecting brain regions like the prefrontal cortex and hippocampus. These regions are most known for their involvement in regulating one’s mood and cognition and initiating a complex set of signal transduction pathways via estrogen receptors [18]. By these signals, estrogen can modulate the function of various neurotransmitters, such as serotonin and GABA [63].
Clinical presentation and complications
The fundamental features of premenstrual dysphoric disorder are mood lability, irritability, dysphoria, and anxiety, which are present in the premenstrual period and resolve shortly after menses [1]. Many women may complain of physical symptoms such as headache, fatigue, cramps, backache, weight gain, acne, constipation, diarrhea [33], and behavioral changes. The symptoms should be confirmed by a prospective daily rating for at least two menstrual cycles accomplished via tools such as the Daily Record of Severity of Problems (DRSP)[34]. The symptoms would be manifested as long as cyclic ovarian hormonal activity persists, meaning that a significant part of women affected could be adolescents [35]. Building on that, PMDD is not found in periods of hypothalamic amenorrhea, pregnancy, breastfeeding, and following menopause[36,37]. Rarely, delusions and hallucinations have been described in the late luteal phase of the menstrual cycle [1].
Like many disorders included in DSM-5, The condition is disabling as it can impair the function of women in different settings. Clinically significant distress with or without a noticeable and marked impairment in the ability to function socially or occupationally in the final week before menses is of major concern, as impairment in social functioning may be manifested by marital discord and problems with children, other family members, or friends. In addition, PMDD had significant effects on concentration [1].
Diagnosis and workup
According to DSM-5 American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders criteria:[1]
Cِriterion A: In most menstrual cycles, at least five symptoms must be present in the final week before the onset of menses (luteal phase), start to improve within a few days after the beginning of menses, and become minimal or absent in the week post menses (follicular phase) At least one (or more) of the following symptoms must be present:
Criterion B:
- Marked affective lability (e.g., mood swings, feeling suddenly sad or tearful, or increased sensitivity to rejection).
- Marked irritability or anger or increased interpersonal conflicts and problems.
- Marked depressed mood, feelings of hopelessness, or self-deprecating(disapproval) thoughts.
- Marked anxiety, tension, and/or feelings of being keyed up or on the edge.
Criterion C: At least one (or more) of the following symptoms must additionally be present, to reach a total of five symptoms when combined with symptoms from Criterion B above.
- Decreased interest in usual activities of life (e.g., work, school, friends, hobbies).
- Subjective difficulty in concentration.
- Lethargy, easy fatigability, or marked lack of energy.
- Marked change in appetite, overeating, or specific food cravings.
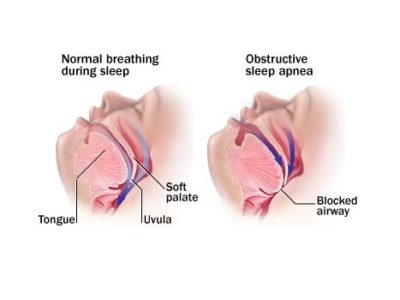
- Hypersomnia or insomnia.
- A sense of being overwhelmed or out of control.
- Physical symptoms such as breast tenderness or swelling, joint or muscle pain, a sensation of “bloating,” or weight gain.
Note: The symptoms in Criteria A-C must have been met for most menstrual cycles that occurred in the preceding year.
Criterion D: The symptoms are associated with clinically significant distress or interference with work, school, usual social activities, or relationships with others (e.g., avoidance of social activities; decreased productivity and efficiency at work, school, or home).
Criterion E: The disturbance is not merely an exacerbation of the symptoms of another disorder, such as major depressive disorder, panic disorder, persistent depressive disorder (dysthymia), or a personality disorder (although it may co-occur with any of these disorders).
Criterion F: Criterion A should be confirmed by prospective daily rating tools during at least two symptomatic cycles, although the diagnosis may be made provisionally prior to this confirmation.
Criterion G: The symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication, or other treatment) or another medical condition (e.g., hyperthyroidism).
Importantly, physical and behavioral symptoms in the absence of mood and/or anxiety symptoms make the diagnosis of PMDD insufficient [1]. The Premenstrual Tension Syndrome Rating Scale is an important tool as it has a self-report and an observer version, both of which have been validated and used widely to measure illness severity [1].
Treatment and management
Selective serotonin reuptake inhibitors (SSRIs) are the first line of treatment for patients with PMDD, given that they have shown efficacy in multiple controlled clinical trials [38-41], and their action in stabilizing the serotonin level, which is thought to be deficient in these patients, thus playing a major role in pathogenesis and symptomatology of this disorder[18]. It was found that there was no difference in efficacy between SSRIs administration only in symptomatic premenstrual period and with continuous daily administration[38]. In contrast to weeks that are required for response in major depression, SSRIs have been shown to have a shorter duration of onset in PMDD, taking effect within hours to days [42]. Active treatment with sertraline has shown to be effective in treating irritability and anger cardinal symptoms of PMDD [43], with weaker effects on depressive and somatic symptoms [38]. Treatment of PMDD patients with comorbid bipolar disorder poses challenges, as SSRIs have a risk of treatment-emergent manic episodes [44].
Oral contraceptives (OCPs), according to some clinical trials, have been shown to significantly improve PMDD symptoms through a combination of drospirenone and ethinyl estradiol (EE) dosed for 24 active days and 4 inactive days for a 28-day cycle [45,46]. On the other hand, other studies have found that the combination with 21 active days and 7 inactive days dosing didn’t show more efficacy than placebo [47]. It is suggested that continuous dosing of OCP without a hormone-free period might be more efficacious than traditional dosing [48], although some studies have shown no difference [49].
Gonadotropin-releasing hormone agonist (GnRHa) Leuprolide is effective, although the significant side effects of ovarian suppression might interfere with compliance and efficacy[50]. Given its major role in pathophysiology, novel pharmacotherapies such as sepranolone, an allopregnanolone antagonist, have been developed and showed a significant reduction in symptoms [51], considering it a promising drug in treating PMDD.
Cognitive behavioral therapy (CBT), especially internet-based, has been shown to decrease the disease burden and its impact on everyday life by increasing cognitive and behavioral coping strategies [52], although it doesn’t produce the effect as rapidly as SSRIs like fluoxetine [53].
Risk factors
Genetics, age of puberty, socioeconomic status, educational level, and cognitive factors were all implicated as possible risk factors [54-57]. Val66Met polymorphism of the Met allele of the brain-derived neurotrophic factor (BDNF) is one of the popular studied genes that may increase the risk in the susceptible carriers[20], [58]. The age of puberty is inversely correlated with developing premenstrual symptoms, and late menarche has a lower risk of developing PMDs [56].
PMDD was significantly higher among older women with low socioeconomic status and lower-educated women [54,55 ]. A study has shown that negative cognitive styles are an important factor in the development of PMDD [57].
Prognosis
Previous results have demonstrated that the different types of impairment and reduced quality of life found with PMDD were comparable in severity to that found in MDD and dysthymia, with worse impairment in social activities and hobbies than in dysthymia, and similar relational impairment in social, marital, and parental relationships in comparison with women diagnosed with MDD. In contrast, women with MDD had more significant occupational and social impairment [59]. The emotional, psychological, and physical symptoms were different in their association with impairment, as the psychological symptoms were the strongest predictors of impairment, while the physical was the least associated with a significant functional impairment [60].
Importantly, PMDD as an independent disorder has a good prognosis in cases of appropriate diagnosis and management [61]. On the other hand, the increased reporting of suicidal ideations, thoughts, and attempts among women with PMDD can be a leading cause of significant morbidity and mortality [4].
References
References...