Article: Neuroleptic Malignant Syndrome
Author: Reem Tayih
Editor: Ihda Mahmoud Bani Khalaf , Sadeen Eid
Reviewer: Ethar Hazaimeh
Keywords: Neuroleptic Malignant Syndrome, Antipsychotics, Differential Diagnosis, Pathophysiology
Overview
Neuroleptic Malignant Syndrome (NMS) is an idiosyncratic life-threatening medical emergency that requires immediate care. (1) NMS is generally conceptualized as a disorder triggered in the brain by neuroleptic blockage of the D2 dopamine receptors in the hypothalamus and brainstem regulatory systems that in turn causes the generalized systemic hypermetabolic syndrome. (2) The most common cause of Neuroleptic Malignant Syndrome (NMS) is the use of Antipsychotic medications, more often first-generation typical Antipsychotics. The typical clinical presentation includes symptoms such as muscular rigidity, altered consciousness, hyperthermia, and autonomic instability. (3) Despite the fact that it is uncommon, NMS remains a critical consideration in the differential diagnosis of patients presenting with hyperthermia and altered mental status because it requires prompt recognition to prevent consequential morbidity and death. (3)
Epidemiology
Incidence rates throughout the years ranged from 0.02%-3%,(4) which is significant. Patients of both sexes and all ages (from children to the elderly) seem to be affected by Neuroleptic Malignant Syndrome (NMS), but young adult males predominate. (2) Instantaneous management and treatment of NMS are crucial since reported mortality rates for NMS vary between 5%-20%. (5) Symptom severity and the occurrence of medical complications are the strongest predictors of mortality. (6) Fortunately, the incidence rate is decreasing due to the development of newer drugs (atypical Antipsychotics) and increased awareness of the condition. (7)
Pathophysiology of NMS
The pathophysiology of Neuroleptic Malignant Syndrome is not completely understood. (20) Several theories have been suggested, with the most common being:
- Blockade of Dopamine receptors
- Genetic predisposition for reduced function of D2 receptors (21)
- Autonomic dysfunction and Sympathoadrenal hyperactivity
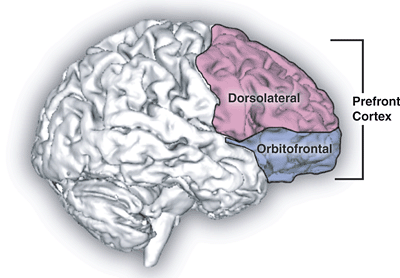
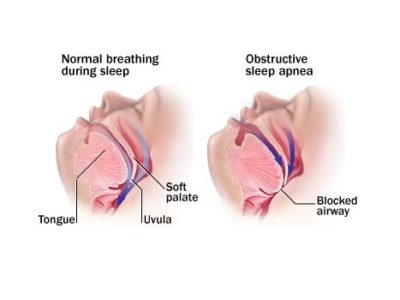
Theories suggest that the blockade of D2-like receptors such as D3, D4, etc. induces the tremendous release of glutamate, which in turn causes the development of muscle rigidity and neurological signs. (22,17) The musculoskeletal symptoms are most likely to be caused by the blockade of D2 receptors, causing the abnormal function of basal ganglia similar to that of Parkinson’s disease. (23) Nevertheless, this theory doesn’t fully explain the symptoms that accompany NMS, so other theories have been suggested such as the Sympathoadrenal hyperactivity hypothesis. (24,23)
The release of calcium is increased from the sarcoplasmic reticulum with antipsychotic use. (25) This can result in increased muscle contractility, which can play a role in muscle rigidity, and the development of fever. Some antipsychotic drugs, such as typical antipsychotics, are known to block D2 receptors; several studies have shown that when dopamine drugs are withdrawn, symptoms similar to NMS are present. (26)
Clinical Presentation and Diagnostic Criteria
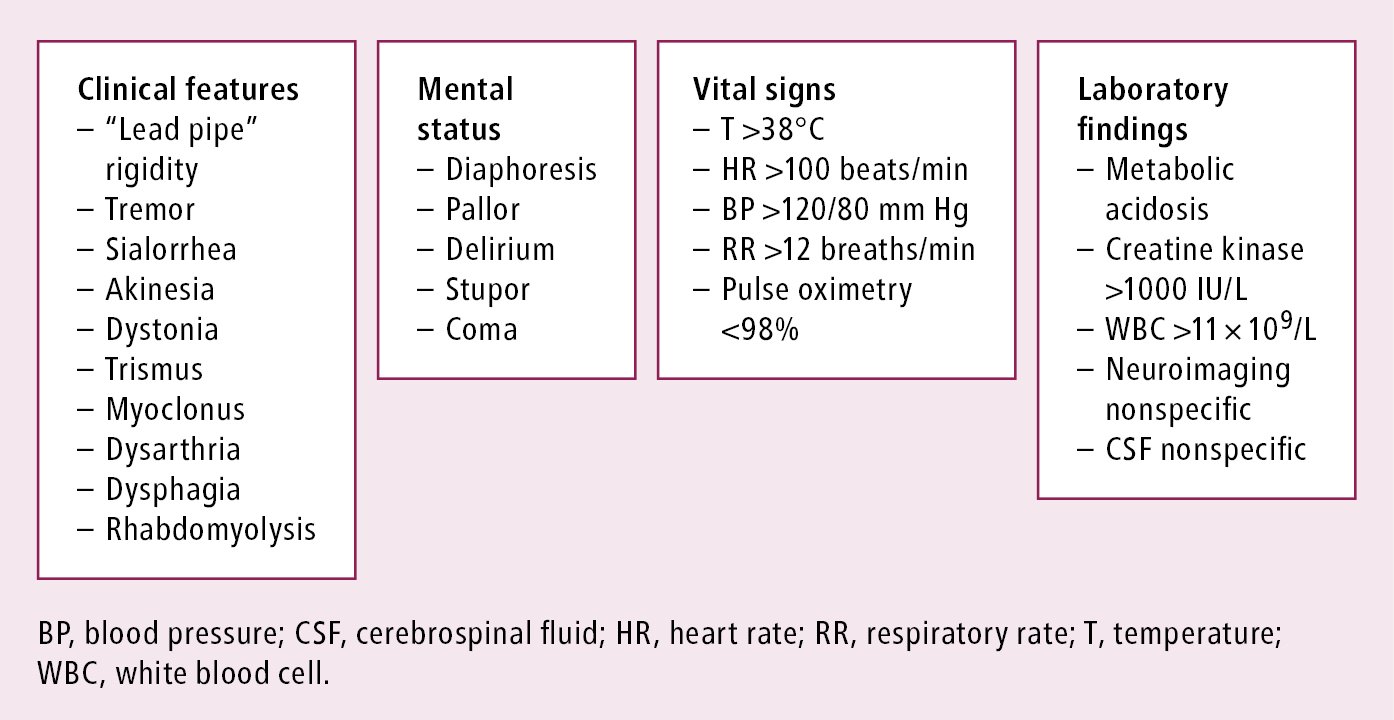
The main risk factor for developing neuroleptic malignant syndrome is the use of antipsychotic medications, especially high potency, and long-acting IM depot forms. (8) Symptoms of NMS develop over several days, and they include hyperthermia, muscle rigidity, altered mental status, and autonomic rigidity. (9) Laboratory investigations are crucial to exclude any other complications. Laboratory abnormalities are associated with NMS, although none are sufficient enough to make a diagnosis. (10)
For instance, patients with NMS might have rhabdomyolysis, resulting in elevated levels of creatine kinase, transaminases, aldolase, and lactic acid dehydrogenase concentrations, this increases the risk of subsequent myoglobinuric renal failure. (11) Patients may also have metabolic acidosis, hypoxia, decreased serum iron concentrations, increased serum catecholamines, and leukocytosis. (12, 1) The results of CSF analysis are normal in most cases (95% of cases). (1) Neuroimaging tends to be within the normal range, and electroencephalography may show generalized slowing. (13) Several analyses show that the development of altered mental status and neurological signs appears before systemic signs. (1)
The DSM-5 criteria for NMS are: (14)
Major criteria (all required)
- Exposure to dopamine-blocking agent
- Severe muscle rigidity
- Fever
Other criteria (at least 2 required)
- Diaphoresis
- Dysphagia
- Tremor
- Incontinence
- Altered level of consciousness
- Mutism
- Tachycardia
- Elevated or labile blood pressure
- Leukocytosis
- Elevated creatine phosphokinase
Medications associated with Neuroleptic Malignant Syndrome
Usually, antipsychotic medications are associated with Neuroleptic Malignant Syndrome (NMS). (3) This syndrome appears with the use of typical Antipsychotics more often, especially the intramuscular depot form. (8) Antiemetic drugs are also associated with NMS, but less than Antipsychotics. (16)
The following table shows examples of drugs that can cause NMS:(3,17,18)
| Typical Antipsychotics | Atypical Antipsychotics | Antiemetic Drugs |
| Haloperidol | Olanzapine | Droperidol |
| Chlorpromazine | Clozapine | Domperidone |
| Bromperidol | Quetiapine | Promethazine |
| Thioridazine | Aripiprazole | Metoclopramide |
| Table (1) Common drugs associated with Neuroleptic Malignant Syndrome (NMS)(19). |
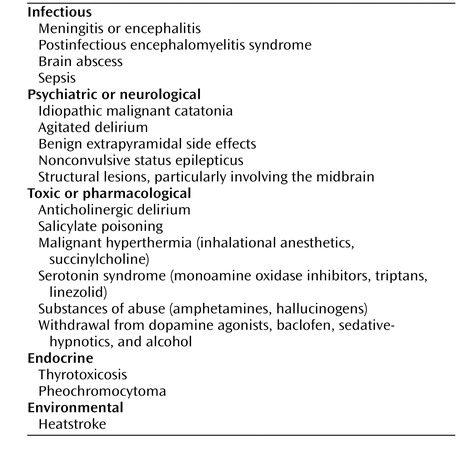
Differential Diagnosis
Serotonin Syndrome is a common differential diagnosis of Neuroleptic Malignant Syndrome (NMS) due to overlapping symptoms, however, it is easily distinguished due to the difference in causative agents. (18) Hyperthermia and muscle rigidity are usually less severe in Serotonin Syndrome than in NMS; In addition to that, Serotonin Syndrome has gastrointestinal symptoms that set it apart from NMS. (27,28) Malignant Catatonia may also present with fever, muscle rigidity, and altered mental status. (29,30) Not only that, but Malignant Catatonia presents with psychological symptoms such as agitation and psychosis. (31) Acute encephalitis, meningitis, and brain abscesses must be differentiated from NMS since they all have common symptoms such as fever and altered mental status; it is crucial since clinicians need to know whether to initiate treatment of CNS infections. (32) Intoxication with drugs such as amphetamines, cocaine, MDMA, and phencyclidine has similar symptoms to NMS. (33,3)
Pharmacological Treatment Options
Neuroleptic Malignant Syndrome (NMS) is considered a neurological emergency, and interventions should be immediately initiated due to its high morbidity and death rates. (3) In most cases, Neuroleptic Malignant Syndrome (NMS) is treated in the intensive care unit. (35) First-line treatment is the removal of the causative agent, which is the antipsychotic (or other offending agents). The morbidity and mortality risk associated with Neuroleptic Malignant Syndrome (NMS) outweighs the risk of untreated psychosis and agitation resulting from the sudden discontinuation of antipsychotic medications. (36)
The second key stage is the commencement of medical therapies. Initiation of IV fluids to restore hydration and correct electrolyte imbalances is a must since elevated levels of CPK pose a risk to the kidneys. (3) Neuroleptic Malignant Syndrome (NMS) is also associated with hyperthermia, which can be managed with cooling blankets or ice packs. (3) Fluid alkalization using bicarbonate has been shown to be useful in preventing renal failure. (1) Several complications arise due to Neuroleptic Malignant Syndrome (NMS), such as renal failure and disseminated intravascular coagulation (DIC) secondary to rhabdomyolysis,(1) Deep vein thrombosis and pulmonary embolism can also arise due to severe dehydration and lack of mobilization, difficulty in swallowing can also cause aspiration pneumonia, and other complications include cardiopulmonary failure, seizures, myocardial infarction, sepsis, and arrhythmias.(37)(38)
Several pharmacological interventions have been proposed for the management of Neuroleptic Malignant Syndrome, such as dantrolene sodium, benzodiazepines, and bromocriptine. (39) Benzodiazepines are widely used in the treatment of Neuroleptic Malignant Syndrome (NMS) since they help control agitation and promote muscle relaxation. (40) Adjunctive Dantrolene therapy is associated with the prolongation of clinical recovery. (41) In addition to that, treatment of Neuroleptic Malignant Syndrome (NMS) with Dantrolene monotherapy is correlated with higher overall mortality. (41) Although Dantrolene is not an evidence-based treatment of choice in cases of Neuroleptic Malignant Syndrome (NMS), it might be useful if premedication consisted of a neuroleptic monotherapy. (41) Bromocriptine is the second-line pharmacological treatment of Neuroleptic Malignant Syndrome (NMS) after the withdrawal of the causative agent. (42) A study has shown that Bromocriptine has a therapeutic effect of 94% when used as monotherapy and a therapeutic effect of 88% when used as a combination therapy. (43) Antipyretics may also be used to treat hyperthermia due to Neuroleptic Malignant Syndrome (NMS). (44)
| Stage | Clinical presentation | Proposed treatment | Treatment setting |
| I: Drug-induced | Rigidity, tremor | Reduce or switch antipsychotics Anticholinergic agents | Psychiatric ward |
| Parkinsonism | |||
| II Drug-induced | Rigidity; mutism; stupor | Discontinue, reduce or switch antipsychotics | Psychiatric |
| catatonia | Use lorazepam (up to 8 mg/day) | ward/MAU | |
| III Mild, early NMS | Mild rigidity; catatonia or confusion; temperature | Discontinue antipsychotics | MAU |
| 538 °C (100.4 °F); heart rate .5100 bpm | Use lorazepam (up to 8 mg/day) | ||
| IV: Moderate NMS | Moderate rigidity; catatonia or confusion; temperature | Discontinue antipsychotics | ICU |
| 38-40 °C (1004-104 °F); heart rate 100-120 bpm | Intensive care | ||
| Lorazepam (up to 8 mg/day), bromocriptine (up to 15 mg/day) or
amantadine (up to 300 mg/day); ECT as second-line therapy |
|||
| V: Severe NMS | Severe rigidity; catatonia or coma; temperature AO °C | Discontinue antipsychotics | ICU |
| (104 °F); heart rate 120 bpm | Intensive care |
Table 2 Treatment stages of Neuroleptic Malignant Syndrome (NMS) (45) (36) (46)
Conclusion
Neuroleptic Malignant Syndrome (NMS) is a rare, uncommon syndrome associated with the use of medications such as Antipsychotics (e.g. Olanzapine, Haloperidol, etc.). This syndrome has deliberating life-threatening symptoms that require immediate management. It has a mortality rate of up to 10%, so clinicians should be careful while prescribing certain medications. It can be managed through several psychopharmacological interventions such as benzodiazepines, dantrolene sodium, and bromocriptine. Despite its lethality, it is treated successfully most of the time with the right interventions.
References...