Article topic: Neuroleptic Induced Parkinsonism
Author name: Mahmoud Abu Tafesh
Editor: Ihda Mahmoud Bani Khalaf , Sadeen Eid.
Reviewer: Ethar Hazaimeh
Keywords: drug–induced, tremor, antipsychotic, dopamine receptors, secondary parkinsonism
INTRODUCTION
Drug-induced parkinsonism is the second most common reason of parkinsonism after Parkinson’s disease and their distinction has important implications in terms of management, treatment, and prognosis. (2) However, distinguishing between these conditions can be challenging from the clinical aspect, especially in the early stages. (2)
Drug-induced parkinsonism (DIP) was initially described as a complication of antipsychotic drugs. Still, it was later recognized as a possible side effect of several other compounds including antiemetics, cholinomimetics, antidepressants, anti-vertigo medications, calcium channel antagonists, antiarrhythmics, and antiepileptic drugs. (3) However, the most common cause of DIP is Neuroleptic Induced Parkinsonism. (4)
Epidemiology
The true prevalence of drug–induced parkinsonism is not confirmed as the case is often under–recognized and epidemiological studies tend to include all categories of parkinsonism or drug–induced movement disorders, rather than drug–induced parkinsonism alone. (5)
The elderly are more prone to developing drug-induced parkinsonism with neuroleptics. (6) In a case-controlled study to evaluate the use of neuroleptic drugs in the 90 days before starting antiparkinson treatment, older people were about 5 times more prone to be commenced on antiparkinson medications while taking neuroleptics compared to non-users. (6) There are 7 Authors who concluded that drug-induced parkinsonism is often misdiagnosed as Parkinson’s Disease (PD) in the elderly. Drug-induced parkinsonism develops in almost 100% of patients with HIV infection treated with neuroleptics. (7)
Pathology
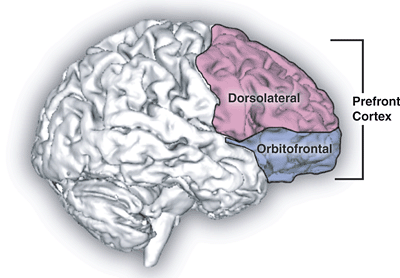
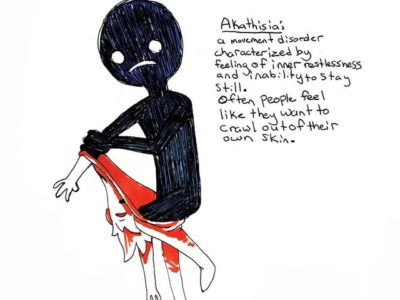
The history of Drug-Induced Parkinsonism (DIP) parallels antipsychotics. (8) Parkinsonism as a side effect of chlorpromazine was first reported 3 years after its release. (8) It was soon recognized that all typical antipsychotics had the potential to cause Extra Pyramidal Symptoms (EPS), including parkinsonism, acute dystonia, and akathisia. (8) Typical antipsychotics are chlorpromazine, promazine, haloperidol, perphenazine, fluphenazine, and pimozide. (8) About 80% of patients taking typical antipsychotic drugs show more than one kind of EPS. (8) Dopamine receptors are heavily distributed in the brain, and typical antipsychotics may act on dopamine receptors in the striatum. Therefore, all patients taking antipsychotics have the risk of developing parkinsonism and other EPS.(8) Parkinsonism usually appears days to weeks after starting to take antipsychotics, but in rare cases, the onset delay may be several months or more. (8) Scientists thought that the risk of EPS is low for atypical antipsychotics. (8) Atypical antipsychotics include clozapine, risperidone, olanzapine, aripiprazole, and quetiapine. (8) Scientists originally thought that their relatively low frequency of associated EPS was because of them being more strongly antagonistic toward serotonin-2A receptors than toward dopamine receptors. (8) Scientists have considered this serotonin-dopamine hypothesis a useful model for developing atypical antipsychotics that shows superior antipsychotic efficacy with a lower incidence of EPS compared to typical antipsychotics. (8) The recent “fast-off” theory suggested that their fast dissociation from D2 receptors after they have blocked them can explain their lower risk of EPS.(8)
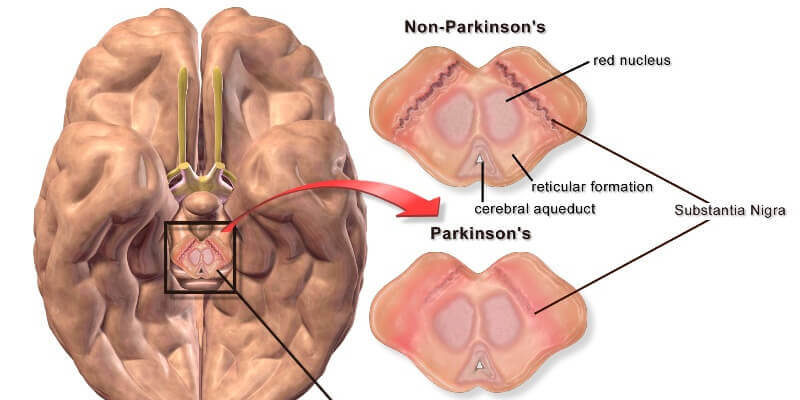
The reversal of parkinsonism after stopping offending drugs does not indicate the disappearance of underlying pathology. (4) Neuroleptics can unmask preclinical Parkinson‘s Disease (PD) in patients with insufficient Substantia Nigra (SN) damage for the disease to manifest clinically. (4) Though the mechanism of sustained parkinsonian features after stopping neuroleptics remains to be established, it is uncommon that dopamine receptor block leads to retrograde SN neuronal degeneration. Also, l‐dopa does not appear to be toxic to SN. (4)
Clinical presentation and complications
The clinical features of Drug-induced parkinsonism (DIP) are variable but in summary, they include variable tremors, depression, and dementia that may present before the onset of parkinsonism. (9) And the onset of these symptoms is more often in the elderly. (9) The differential diagnosis between DIP and other types of parkinsonism is not always easy and may not be possible based only on the clinical symptoms. (9) idiopathic Parkinson’s Disease (IPD) is characterized by asymmetric involvement of body limbs. Asymmetry is less characteristic of DIP although it may occur. (9) In contrast with vascular parkinsonism, which heavily involves the legs and produces frequent impairment of gait, DIP produces a less severe gait disorder and a relatively more pronounced ‘masked’ facial expression. (9)
Parkinsonism has also been related to a series of abused substances. (10) Scientists have associated Alcohol with withdrawal from Parkinsonism. (10) Cocaine is known to cause parkinsonism due to direct vascular damage and is a major risk factor for antipsychotic-induced extrapyramidal side effects. (10)
There is a study that reports that physicians should be aware of DIP as a potential neurological complication after bone marrow transplant (BMT) to avoid further taking of drugs that could aggravate symptoms. (11) The natural course of Neuroleptic induced parkinsonism (NIP) remains unknown, including whether NIP is a risk factor for the later development of tardive dyskinesia. (12)
Diagnosis
Neuroleptic drugs cause basal ganglia side effects which are frequently ignored, misdiagnosed, or mistreated by the patient or physician. (13) Such side effects must be anticipated and appropriate management instituted so that patient compliance with the drug regimen is increased and the therapeutic relationship is controlled. (13) Side effects can be detected in frequent and complete examinations of the head and neck, limbs, chest, and back. (13) The various medications for drug-induced parkinsonism are reviewed, with an emphasis on the indications for section and the effects of each drug. (13)
The examination of a patient who may have side effects from neuroleptics must be thorough and frequently repeated. (13) That enables the correct treatment to be initiated and the patient’s progress to be monitored. (13) Because only one extremity or one muscle group may be affected by drug-induced parkinsonism, each part of the body must be examined by the physician. (13)
For the head and neck, when side effects are present, the face is characterized by masked facies and rigidity of muscles both at rest and during active movements, such as talking or smiling. (13) But extremities, each limb, and joint should be examined separately. (13) However in the trunk and other areas, dystonias or muscle contractures can occur in the back, eyes, or one of the extremities. (13)
DSM5 criteria for Neuroleptic induced Parkinsonism
The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) criteria for neuroleptic-induced parkinsonism are as follows (14):
A. Development of at least two of the following parkinsonian symptoms: resting tremor, cogwheel rigidity, bradykinesia, and postural instability.
B. Symptoms must develop within four weeks of starting or increasing the dose of a neuroleptic medication or within four weeks of reducing or stopping an effective antiparkinsonian medication.
C. The symptoms must not meet the criteria for dementia with Lewy bodies, Parkinson’s disease, or another specific Parkinsonian disorder.
D. Symptoms must cause distress and/or functional impairment.
It is important to note that neuroleptic-induced parkinsonism is a common side effect of many antipsychotic medications, and it is important to monitor individuals for the development of these symptoms when prescribing such medications.
Figure 1: I-FP-CIT PET imaging in two DIP patients. DAT uptake was normal and symmetric in the bilateral striatum in a pure DIP patient (A). In contrast, it decreased severely in the right striatum in a patient who was diagnosed with PD unmasked by DRBAs (B). DAT: dopamine transporter, DIP: drug-induced parkinsonism, DRBA: dopamine receptor blocking agents, PD: Parkinson’s disease. (8)
Treatment and management
There are three major components in the management of side effects caused by neuroleptic-induced parkinsonism. (13) Which are education and reassurance, a decrease in the dosage of the neuroleptic drug, and the administration of an antiparkinsonian drug. (13)
Patients should be forewarned that side effects may occur and that their appearance is a sign that tells us that the medication is working. (13) Patients should be encouraged to report side effects early. (13) They can be reassured that most side effects remit spontaneously within a few days or weeks, and that medication is available for more serious side effects. (13)
Decreasing the dosage of the neuroleptic drug is often the best approach if the psychosis (on anxiety or impulsivity) that warranted its use is under control. (13) The physician and the patient must weigh the advantages of a decrease in the side effects with the disadvantage of possible recurrences of symptoms. (13) If the neuroleptic cannot be decreased, then it may be prudent to prescribe medication for the side effects. (13)
It is commonly assumed that all antiparkinsonian agents are equally effective, but it appears that there may be important differences between the drug groups in their effectiveness and side effects. (13) The earliest drugs used for basal ganglia side effects included atropine, belladonna, scopolamine, stramonium, and hyoscine. (13) Even among these older drugs, a differential effect was noticed, with scopolamine and hyoscine more effective for tremors, and atropine and stramonium better for rigidity and dystonias. (13) However, these drugs caused prominent anticholinergic side effects, and today synthetic preparations are more commonly used. (15) Although many of the agents useful in treating Parkinson’s disease have been useful for drug-induced parkinsonism, L-dopa has not been very effective because of the dopamine blockade of the neuroleptics. (15)
Table 1: Antiparkinsonian Drugs Available in France in 2007. (16)
Risk factors
The age and size of hyperechogenic Substantia Nigra (SN), measured by transcranial ultrasound (TCS), seem to be associated with the occurrence and severity of NIP in neuroleptic-treated psychiatric patients. (17)
In contrast, smoking appears to have a certain protecting effect. (18) It’s accepted that the prevalence of smoking is increased in psychiatric patients as compared to healthy controls. Studies have reported prevalence rates to vary from 68% (19) to 94% .(18) in schizophrenic patients, whereas depressed patients showed an elevated lifetime prevalence of smoking with 74% compared to 53% in healthy controls. (20) Concerning the protecting effect, tobacco smoke acts as a brain MAO-B inhibitor. (21) and reduces crucial role by inducing microsomal enzymes, thus, increasing hepatic metabolism. (23) This did not result in higher neuroleptic doses for smokers as other authors reported, but was associated with a greater number of prescribed neuroleptic drugs. (17)
Prognosis
Scientists found it difficult to predict the prognosis in patients with DIP. (18) Scientists evaluated whether the combined use of F-N-(3-fluoro propyl)-2 beta-carbon ethoxy-3beta-(4-iodophenyl) nortropane (FP-CIT) positron emission tomography (PET) and cardiac meta-iodobenzylguanidine (MIBG) scintigraphy can be used to help differentiate the prognosis in patients with DIP. (18) Among 20 patients enrolled, only 16 showed normal Dopamine transporter (DAT)uptake and normal myocardial sympathetic innervation. After the withdrawal of the suspected drugs, the patients experienced a clinical remission of parkinsonian motor symptoms in 3 months and did not face any new movement symptoms after at least 2 years of follow-up. (24)
Absence of NIP in psychotic patients receiving adjunctive ECT
A hypothesis is proposed that bilateral electroconvulsive therapy (ECT) protects against neuroleptic-induced parkinsonism and thereby may reduce the risk for the subsequent development of tardive dyskinesia. (25)
References...