Article Title: Medication-induced Akathisia
Author: Mouns Saed Radaideh
Editors: Ihda Mahmoud Bani Khalaf , Sadeen Eid.
Reviewer: Ethar Hazaimeh
Keywords: akathisia, antipsychotics, motor restlessness, dopamine D2 receptors, medication-induced
Overview
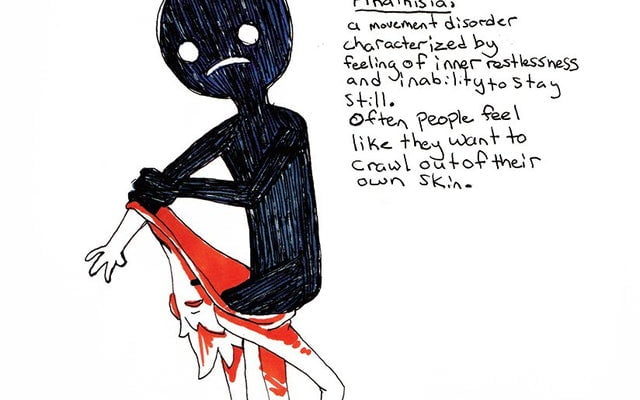
Akathisia is a very common and distressing movement disorder that can be associated with antipsychotic drug use. It is characterized by subjective (inner restlessness) and objective (excessive movements) components. Akathisia may have a negative impact on clinical outcomes and even lead to treatment discontinuation. (1)
Diagnosing akathisia is sometimes hard as it can be confusing – A mild degree of akathisia could be misattributed to psychotic agitation, resulting in further escalation of the offending drug. On the other hand, it can co-occur or be caused by other psychiatric and organic conditions (including acute psychosis, comorbid affective disorders, drug withdrawal states, insomnia, and delirium), as well as other psychotropic medication, most commonly antidepressants. (2)
Propranolol, a non-selective beta-adrenergic receptor antagonist, is considered to be the first-line treatment for antipsychotic-induced akathisia (AIA). (3)
History & Epidemiology of Akathisia.
Akathisia is a term derived from the Greek for ‘inability to sit’. Refers to a neuropsychiatric syndrome characterized by subjective and objective psychomotor restlessness. Although recognized soon after the use of antipsychotic medication. (4) Historically, the dominant symptom of akathisia is disorientation. Haskoves, who described the syndrome in 1901, concluded that the illness was hysterical. Bing classified akathisia as a “psychosis” characterized by a “morbid fear of sitting,” but explained it in another chapter as a way to overcome the muscle stiffness of Parkinson’s disease. Oppenheim described akathisia as a form of neurosis, “usually a form of a phobia”. (5) Wilson designated it “hysterical” in one chapter of his classic textbook, and also described the syndrome in association with Parkinson’s disease in a later chapter. (5) The incidence of the disease among people using antipsychotic drugs ranges from 5-50% depending on the duration of treatment and the drug used. (6)
Pathogenesis and etiology
Akathisia was initially classified as part of the extrapyramidal syndrome (EPS) induced by antipsychotic drugs, but some evidence suggests that akathisia is distinct from other EPS manifestations. (6) The mechanism is the inhibition of dopaminergic neurotransmission in the nigrostriatal pathway for acute events, whereas tardive dyskinesia has been attributed to D2 receptor upregulation and subsequent hypersensitivity to dopamine following prolonged exposure to D2 antagonists. Patients are characteristically indifferent to EPS and the presentation is more distressing to observers of the movement disorders than to those experiencing them.(6)
Akathisia is classified according to the time range of symptoms development. Acute akathisia occurs within a few days to weeks of the beginning of treatment or increasing the dose of antipsychotic medication. If akathisia develops later, it is considered subacute or chronic. (7) Chronic akathisia is when akathisia has been present for several months. In contrast, tardive akathisia occurs later (1-3 months) during treatment with antipsychotics, and it may even appear after antipsychotic discontinuation or dosage reduction. Tardive akathisia is reduced by increasing the antipsychotic dose but it may also persist for months to years after the antipsychotic is discontinued. (7) Despite that akathisia can occur due to antipsychotic drug withdrawal, it can also occur with illicit substance intoxication and withdrawal states. The syndrome is most seen with the use of cocaine, methamphetamine, MDMA, ecstasy, and GHB. Alcohol and opioid withdrawal can give rise to anxious, restless states which are similar to akathisia.(8)
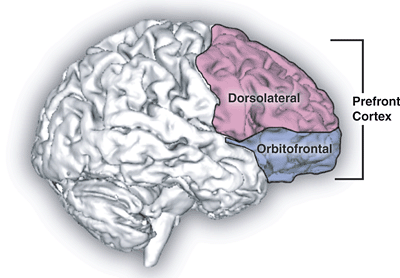
The neurotransmitters mostly associated with akathisia are gamma-aminobutyric acid (GABA) and serotonin. GABA (mainly via GABAA receptor interactions) produces an influence on dopamine-dependent signaling, thus, increasing or reducing activity. With a distinctive distribution pattern, serotonin is also associated with motor regulation through serotonin receptors found in several cortical areas as well as the striatum. More specifically, serotonin manages dopaminergic motor function in the Nigro-striatal system. (7)
Clinical presentation and complications
The presentation of akathisia is different from restless leg syndrome (RLS), though the pathophysiological foundation may be similar. Patients with RLS complain of an intolerable sensation in the legs and an insurmountable urge to move them. It is worse during the night and the pain associated with it is primarily due to its disruptive effect on sleep. Patients may have a history of drug abuse, as RLS is commonly present in the post-acute withdrawal syndrome of many illicit drugs. It is also associated with iron deficiency. (6)
When akathisia is mild to moderate in severity, the lower extremities are predominantly involved, usually from the hips to ankles, and the movements take the form of shifting positions while standing and moving the feet while sitting. (9) The predilection to affect primarily the lower extremities is often helpful in differentiating akathisia from other antipsychotic-induced side effects that tend to affect other body parts. With increasing severity, however, akathisia can involve the entire body, resulting in near-unceasing writhing and rocking movements often accompanied by jumping around, running, and occasionally flinging oneself out of a chair or a bed. (9) Patients typically exhibit other evidence of mild or early extrapyramidal dysfunction such as decreases in facial expression (despite complaints of extreme subjective distress), a rapid shuffling gait with a lack of accessory movements, decreased blink rate, and a positive glabellar reflex. A mild intention tremor and cogwheel rigidity can also be present. Mild rigidity can best be drawn out by recruitment. Movement rating scales are important instruments for adequate identification. (10)
Diagnosis
The clinical diagnosis of akathisia may be complicated because the intensity can vary according to the case and the degree of arousal. It has to be differentiated from psychotic agitation and anxiety, substance abuse or withdrawal syndromes, some somatic illnesses (for example, hyperthyroidism, hyponatremia), or neurologic disorders (for example, Parkinson’s disease, restless legs syndrome) The Barnes Akathisia Rating Scale (BARS), a 4-item scale. with good validity and reliability, recommended to diagnose akathisia, as well as to monitor its severity. (11)
The patients with akathisia would experience a desire to move, an awareness that they could not keep their legs still, or a compulsion to move which was often particularly referable to the legs. (12) Many patients complained that the condition was least tolerable when they were required to stand still, for example when lining up for meals or medication on the ward, waiting at the supermarket checkout, or standing in the kitchen while cooking. These symptoms constitute the subjective diagnostic criteria for akathisia included in the item ‘awareness of restlessness’ on the scale. (12)
The BARS rate the observable movements on a separate Objective item, with severity points attached with descriptions of the nature of the movements and the proportion of time they are exhibited. (13)
After assessing the objective and subjective (awareness of restlessness and distress related to restlessness) components of BARS, the assessor will systematically gain information on the intensity of the feelings of restlessness, the level of associated distress, and the type and frequency of fidgety, restless movements. This allows for an overall measure of severity to be made using the Global item. It was anticipated that the Global item score, incorporating all these elements of the condition, would provide a better reflection of overall severity than a sum of the other items, and would be relevant for most research and clinical purposes. (13) The Global item score allows for prevalence or incidence estimates: using accepted definitions of akathisia, the diagnostic threshold score on the Global item is 2 (i.e. a score of 2 or more indicates the presence of akathisia) (Barnes, 1989). (13)
| Barnes Akathisia Rating Scale
|
Prince Henry Hospital Akathisia Rating Scale
|
| OBJECTIVE (rated 0-3)
0. Normal – occasional fidgetiness 1. Characteristic movements – present less than half the time 2. As above: present for at least half the time 3. Constant during the time observed
|
OBJECTIVE (each rated 0-3)
1. Sitting 1. Semipurposeful/purposeless leg/feet movements 2. Semipurposeful hand/arm movements 3. Shifting body position in chair 4. Inability to remain seated
|
| SUBJECTIVE
Awareness of restlessness (0-3) 0. Absence of inner restlessness 1. Non-specific inner restlessness 2. Awareness 3. Awareness of intense compulsion 2. Standing
|
2. Standing
1. Purposeless/semi-purposeless leg/feet movements 2. Shifting weight and/or walking-on-the-spot 3. Inability to remain standing (walking/pacing)
|
| Distress related to restlessness (0-3)
0. None 1. Mild 2. Moderate 3. Severe
|
SUBJECTIVE (each rated 0-3)
1. Feelings of restless, especially in legs 2. Inability to keep legs still 3. Inability to remain still, standing or sitting
|
| Global clinical assessment of akathisia (ratings 0-5)
(anchor definitions provided) 0. Absent 1. Questionable 2. Mild (anchor definitions provided) 3. Moderate 4. Marked
|
Global rating
Absent: 0 Mild: 1 Moderate: 2 Severe: 3
|
Table 1: Standardized recording of akathisia: two scales derived from a single source.[14]
DSM 5 diagnostic criteria for drug-induced akathisia
Here are the DSM-5 criteria for drug-induced akathisia:
- Restlessness or the need to move frequently, which is usually accompanied by an unpleasant subjective sensation (e.g., crawling, creeping, pulling, itching, tingling, burning, or aching) in the lower limbs. (15)
- restlessness is caused by antipsychotic or other dopamine-receptor-blocking agents (e.g., metoclopramide).(15)
- The restlessness is not due to a medical condition (e.g., parkinsonism, dystonia, chorea, or tics) or akathisia caused by another medication. (15)
- restlessness is not better accounted for by another mental disorder (e.g., anxiety disorder, obsessive-compulsive disorder, or attention-deficit/hyperactivity disorder). (15)
Treatment and Prognosis
Sadly the actual evidence base for treatments of akathisia is very small, and many of the recommendations are based on clinician experiences, case reports, and reports from studies of drugs where akathisia was not a primary concern. (9) First, the cause of the akathisia should be identified and initial treatment aimed at that cause. Since the most of patients with akathisia probably developed it secondary to psychotropic medications, the initial recommendation is, if possible, to reduce or switch medication. (9)
For treatment, anticholinergic drugs such as benztropine, biperiden, and benzhexol were most used in the past. In fact, some investigators considered a response to an anticholinergic drug as diagnostic for acute akathisia. (16) Other studies have shown that only some patients respond, and often partially, and this response may relate to the presence of Parkinsonian side effects. Some favor benzhexol over other drugs when they do use them, but research evidence for this is lacking. (16,17)
The doses commonly used in the treatment are 2 to 6 mg/day of benztropine, or the equivalent, although higher doses may sometimes be necessary. Benzodiazepines, especially diazepam, lorazepam, and clonazepam, have been used again with partial success, as have other sedative drugs such as barbiturates and diphenhydramine. (16)
In the last few years, adrenergic drugs have received a lot of attention. (18)A number of studies have shown that small doses (20 to 60 mg/day) of propanol can produce a significant improvement that usually occurs within a few hours. (19) Most studies of propranolol have been uncontrolled, but all have been positive, and a recent double-blind cross-over study has supported this conclusion. (19) Others have reported benefits with selective beta-1 antagonists(20) and even with peripherally acting beta-adrenergic antagonists,(21) but these results have not been consistent; propranolol is at present the preferred drug. Clonidine is also reported to be successful. (22)
Rarely, dopamine agonists like bromocriptine and amantadine have been tried. (23) Finally, piracetam,(24) buspirone, and opiates have been suggested to be of benefit in case reports of more severe akathisia. (23)
A slower infusion of metoclopramide decreases the rate of akathisia. A double-blind clinical trial of patients aged 18 years and older who were to receive intravenous metoclopramide for treating nausea, vomiting, or headache was eligible. Patients were excluded if they were taking medications that might mimic or mask akathisia, had a movement disorder, or renal insufficiency, or were unable or unwilling to consent. In conclusion, a slower infusion of metoclopramide reduces the incidence of akathisia. (28)
Risk factors
Although acute antipsychotic-induced akathisia is often thought of in association with schizophrenia, it appears that patients with mood disorders, particularly bipolar disorder, may be at higher risk. (9)
Other risk factors may include exaggerated dose or rapid dose increase, traumatic brain injury, cancer, and possibly iron deficiency. (9) No proven evidence of risk is associated with age, gender, or ethnic background. (25) Chronic or tardive akathisia may be related to advanced age and female gender, just as is tardive dyskinesia. (26)
Patients in palliative care units may face several neuropsychiatric syndromes that include delirium, agitation, and other behavioral disturbances due to types of neurological and neuropsychiatric conditions. In addition, they also develop nausea and other general medication disturbances. (27)
Conclusion.
It’s important to raise awareness about akathisia and its symptoms, as well as to advocate for more research into effective treatments. By doing so, we can help those who suffer from this condition and improve their quality of life.