Article topic: Medication-induced acute dystonia
Author name: Zaid Shakhatreh
Editor name: Ihda Mahmoud Bani Khalaf
Reviewer: Ethar Hazaimeh
Keywords: medication-induced acute dystonia, dystonia, muscle contractions, movement disorder, drug-induced, antipsychotic, extrapyramidal symptoms, EPS
Overview
Medication-induced acute dystonia is a movement disorder characterized by uncontrollable, repetitive motions of the body and is frequently observed in patients receiving drugs that modulate dopamine and other neurotransmitters in the brain such as antipsychotics,1 antiemetics, antidepressants, and anticonvulsants. 2 It is characterized by involuntary muscle contractions that can cause abnormal and often repetitive movements, postures, or both,3 usually occurring in the face, neck, or limbs, that can result in twisting or repetitive movements.4
The term dystonia was introduced by Hermann Oppenheim in 1911,5 but references to this disorder can be traced back to ancient times. Some statues, sculptures, paintings, and literary works may depict people with dystonia-like features.6 However, for a long time, dystonia was considered a psychogenic or hysterical condition, influenced by Freudian theories and the lack of clear neuropathology. It was only in the late 20th century that dystonia was recognized as an organic disease.6,7 Dystonia’s classification system is now informed by neurogenetics, with over 20 genetically defined subtypes and many more inherited or acquired conditions that include dystonia as a feature. However, some historical tensions remain unresolved, such as the role of psychological factors in both organic and functional dystonia. Advances in neuroimaging and cognitive neuroscience have challenged the dualistic mind-brain models and suggested more inclusive biopsychosocial approaches to dystonia. 6
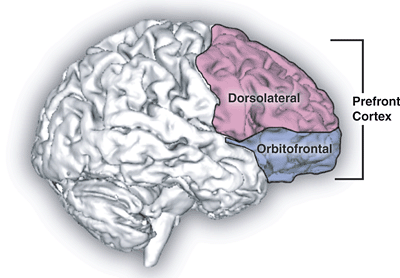
Pathogenesis and Etiology
The exact pathophysiology of drug-induced dystonia is not fully understood, but it is thought to be related to a disruption of the balance between dopamine and acetylcholine in the basal ganglia.8 Dopamine is a neurotransmitter that plays a critical role in regulating motor function, while acetylcholine is another neurotransmitter that opposes dopamine and helps to control muscle contractions. When dopamine receptors are blocked by medication, the balance between dopamine and acetylcholine is disrupted, leading to involuntary muscle contractions and spasms characteristic of dystonia.8
Antipsychotic and antidepressant drugs are the most common medications that induce acute dystonia.9,10 However, some antiemetics can also cross the blood-brain barrier and affect dopamine receptors in other parts of the brain, causing dystonic reactions.11 Some drugs are more likely to cause dystonic reactions than others. For example, high-potency neuroleptics such as haloperidol and fluphenazine have a higher risk than low-potency neuroleptics such as chlorpromazine and thioridazine.12–14 The risk also increases with higher doses, intravenous or intramuscular administration, rapid titration, and longer duration of treatment.13 Moreover, some individuals are more prone to develop dystonic reactions than others. For instance, young males, patients with a history of substance abuse or psychiatric disorders, and patients with genetic mutations in dopamine-related genes have a higher susceptibility.15,16,17
Some medical conditions or drugs can increase the risk of dystonic reactions by altering the levels or activity of dopamine or other neurotransmitters in the brain. For example, dehydration, hypocalcemia, hypomagnesemia, hypokalemia, stroke, traumatic brain injury, Parkinson’s disease, Huntington’s disease, Wilson’s disease, antihistamines, anticonvulsants, antimalarials, cocaine, caffeine, oral contraceptives.18–22
Epidemiology
The epidemiology of drug-induced dystonia is not well established, as different studies have used different definitions, methods, and populations to estimate its prevalence and incidence. However, some general trends can be observed based on the available literature. Drug-induced dystonia is more common in young males, especially those with a history of substance abuse(cocaine/alcohol) or psychiatric disorders.2,17,23 Its likelihood is higher in children and declines with advancing age. 24
Antipsychotics can cause acute dystonia in 2-3% of patients who receive them, usually within the first 48 hours of taking the drug.25 The frequency of acute dystonia reactions can range from 2.8% to 25% depending on the type of antipsychotic being used.23,26
The prevalence of drug-induced dystonia varies depending on the type and dose of the drug, the duration of exposure, and the presence of risk factors. Therefore, the prevalence varies widely from 2% to 90%. 2
Clinical Presentation and Complications
Acute dystonia can occur within minutes to hours of taking a single dose of a dopamine-blocking drug or within 24 to 96 hours of starting or increasing the dose of such a drug.12 Some dystonic movements last several seconds/minutes but others can last for weeks/months. This can lead to permanent bone deformity and impairment in function.22
The clinical presentation and signs and symptoms of drug-induced dystonia vary depending on the affected body region and the severity of the condition. Some of the common symptoms and signs are:
- Oculogyric crisis: an involuntary upward or lateral deviation of the eyes, causing difficulty in seeing and blinking. It can be accompanied by facial grimacing, tongue protrusion, and neck extension.27
- Torticollis: a condition where the neck muscles contract and cause the head to tilt or twist to one side. It can cause pain, stiffness, difficulty in moving the head, swallowing problems, and cosmetic concerns.22
- Trismus: a spasm of the jaw muscles, limiting the opening or closing of the mouth.28
- Laryngeal dystonia: a condition where the vocal cords spasm and cause difficulty in speaking or breathing. It can cause hoarseness, strained or breathy voice, choking sensation, coughing, or respiratory distress.17
- Opisthotonus: contraction of the back muscles that cause the body to arch backward.17
- Tremor.22
Drug-induced dystonia can have various complications that affect the quality of life and health of the patients. Some of these complications are:
- Rhabdomyolysis: A syndrome characterized by muscle necrosis and the leakage of intracellular muscle constituents into the circulation, which can impair renal function.29 Rhabdomyolysis can occur as a rare complication of drug-induced dystonia,30 especially if prolonged dystonia is present. It can cause muscle pain, weakness, dark urine, fever, nausea, vomiting, etc. It can lead to kidney failure if not treated promptly.29
- Dystonic storm: This is a life-threatening condition where severe and generalized dystonia occurs along with fever, sweating, tachycardia, hypertension, etc. Dystonic storms can occur as a rare complication of drug-induced dystonia, especially in patients with primary known dystonia (e.g., DYT1 dystonia). It can be triggered by infection or medication adjustment in some cases. It can cause respiratory failure, cardiac arrest, or death if not treated urgently.31
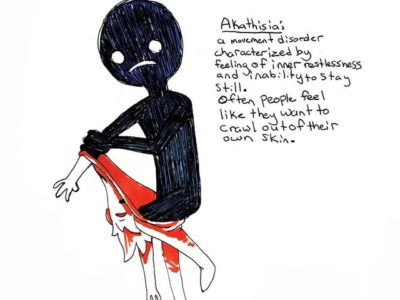
- Extrapyramidal symptoms (EPS): These are a spectrum of movement disorders that arise from the disruption of the basal ganglia, a brain region involved in motor control. Drug-induced dystonia can be considered a subset of extrapyramidal symptoms that share a common pathophysiology and etiology. EPS includes dystonia, akathisia (restlessness), parkinsonism (slowness and stiffness), and tardive dyskinesia (involuntary movements of the face and limbs). EPS can interfere with social functioning, communication, motor tasks, and activities of daily living. They can also cause psychological distress and poor adherence to treatment.32
Diagnosis and workup
The diagnosis of drug-induced dystonia is based on the history of exposure to a likely causative medication, and the clinical features of the movement disorder, by the observation of the type and pattern of abnormal movements and postures, which requires expert neurological assessment.33
The first diagnostic criteria were proposed by Herz,34 who suggested that dystonic movements and postures are the hallmark phenomenology of dystonia. They form the main physical signs and are complemented by three other physical signs: gestes antagonists (“sensory tricks”), mirror dystonia, and overflow dystonia. Fahn observed that dystonic movements are often mistaken for other types of involuntary movements, and they can vary in speed and regularity.35 Sometimes, they can appear as tremors alone, without any other hints of dystonia. This can make it hard to recognize dystonia in patients who only have tremors. 36 The exact criteria for diagnosing dystonia in different parts of the body are not clear yet, and some cases may go unnoticed. Focal dystonia syndromes lack specific diagnostic criteria; hence, only general criteria are currently available.33
Neuroimaging and lab tests may be helpful to rule out other causes of dystonia, such as structural lesions, metabolic disorders, or genetic conditions, especially when dystonia is combined with other neurological features.37 A recent review summarized more than 100 different disorders where dystonia may be combined with other features.38
Some examples of neuroimaging and lab tests that may be used in drug-induced dystonia are:
- MRI or CT scan to look for any brain lesions or degenerative conditions.33
- Blood or urine tests to measure the levels of the drug or its metabolites, or to check for any signs of toxicity, such as liver or kidney dysfunction, or electrolyte imbalance.33,39
- Genetic tests to screen for any mutations that may predispose to dystonia, such as variants in the DRD2 gene that encodes the dopamine D2 receptor.33
- Electromyography (EMG). This test measures the electrical activity within muscles.33,39
A characteristic and almost unique feature of dystonic movements is the presence of sensory tricks or gestes antagonists. These are actions or stimuli that temporarily stop the muscle spasms. For instance, some people with cervical dystonia (torticollis) can touch their chin or face to relieve their neck contractions. Some people with oro-lingual dystonia can put a finger on the lips or an object in the mouth to ease their mouth spasms. Sensory tricks may involve changes in the brain’s sensory feedback or motor planning mechanisms.22
DSM-5 criteria for medication-induced acute dystonia
The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) criteria for medication-induced acute dystonia is as follows40:
1- The condition involves involuntary and sustained muscle contractions that affect different parts of the body, such as:
- The eyes, causing them to roll upward or sideways (oculogyric crisis)
- The head and neck, causing them to twist or tilt in abnormal positions (torticollis or retrocollis)
- The limbs or trunk, causing them to bend or arch in painful ways
2-The condition develops within a few days of starting or increasing the dose of a medication that affects the brain and movement (such as a neuroleptic) or after reducing the dosage of a medication used to treat extrapyramidal symptoms.
Differential diagnosis
Drug-induced acute dystonia reaction may be challenging to distinguish from other conditions, these include Huntington’s disease, Wilson’s disease, Parkinson’s disease, conversion disorder, tetanus, focal seizure, strychnine poisoning, hypocalcemia, anticholinergic toxicity, meningitis, neuroleptic malignant syndrome, stroke, temporomandibular joint dislocation, mandibular fracture, orbital fracture, and clonus.13,32,41
Treatment and management
Discontinuation or reduction of the causative drug: This is an important step in managing medication-induced acute dystonia. involves gradually stopping or reducing the dose of the offending medication, under the guidance of a doctor. If the medication is essential for the patient’s mental health, a different class of antipsychotics, called atypical neuroleptics, may be used instead. These drugs have a lower risk of causing dystonia.47
Both pharmacological and non-pharmacological treatments have proven effective for drug-induced dystonia, The following are some of the available treatment methods:
- Anticholinergic drugs: These are the most effective medications for dystonia, according to clinical evidence and expert opinion.42 Anticholinergic drugs can help relax the muscles and reduce the spasms caused by dystonia. Examples of anticholinergic drugs that are commonly used include benztropine, trihexyphenidyl, biperiden, and procyclidine. These drugs are usually given orally or intramuscularly as soon as possible after the onset of symptoms. They may cause side effects such as dry mouth, blurred vision, constipation, urinary retention, confusion, and sedation.37
- Benzodiazepines: They enhance the activity of gamma-aminobutyric acid (GABA), a neurotransmitter that inhibits nerve impulses in the brain. Benzodiazepines can help calm the nervous system and reduce anxiety and agitation associated with dystonia. Some benzodiazepines that are used for dystonia are diazepam, lorazepam, clonazepam, and alprazolam. These drugs are usually given orally or intravenously as an adjunct to anticholinergic drugs. They may cause side effects such as drowsiness, dizziness, memory impairment, dependence, and withdrawal symptoms.37
- Diphenhydramine: This is an antihistamine drug that inhibits histamine receptors and prevents allergic reactions. Diphenhydramine also has anticholinergic properties and can help relieve dystonic symptoms. It is usually given intravenously or intramuscularly as an alternative to anticholinergic drugs.43,44
- Intrathecal baclofen is a form of treatment that involves delivering baclofen, a muscle relaxant drug, directly into the spinal fluid around the brain and spinal cord.37,45
- Levodopa: This is a medication that is used to treat Parkinson’s disease and some forms of dopa-responsive dystonia. Levodopa is converted into dopamine, a neurotransmitter that regulates movement, in the brain. Levodopa can help improve dystonic symptoms in some patients with drug-induced acute dystonia, especially if it occurs as a side effect of antipsychotic drugs or other drugs that affect the dopamine system in the brain.42,46
- Botulinum toxin injections: Botulinum toxin works by blocking the release of acetylcholine at the neuromuscular junctions, thereby paralyzing the muscles. Botulinum toxin can help reduce dystonic spasms and improve function and appearance in focal or segmental dystonia. It may cause side effects such as pain, bruising, swelling, weakness, infection, and antibody formation.33
- Speech therapy: a form of therapy that involves exercises and techniques to improve speech production and communication skills. Speech therapy can help people with dystonia affecting their oral muscles to speak more clearly and fluently.32
- Physical therapy: This is a form of therapy that involves exercises and stretches to improve muscle strength, flexibility, coordination, and posture. Physical therapy can help prevent muscle stiffness and contractures caused by dystonia. It can also help improve mobility and function in daily activities.33
- Psychotherapy: therapy that involves talking to a mental health professional to address emotional and psychological issues related to dystonia. Psychotherapy can help people with dystonia cope with stress, anxiety, depression, low self-esteem, social isolation, and stigma.32
- Surgery is not a common treatment for drug-induced dystonia, but it can be considered for some patients who do not respond to other treatments.42 Surgery for dystonia usually involves deep brain stimulation (DBS), which is a procedure that involves implanting electrodes in specific areas of the brain and connecting them to a battery-operated device that delivers electrical impulses to modulate the abnormal brain activity that causes dystonia.33,42,45
Prophylaxis
Anticholinergics should be maintained after the resolution of dystonia as a prophylactic measure against recurrence, in conjunction with antipsychotics. The typical protocol involves co-administering an anticholinergic with the antipsychotic for 4 to 7 days, followed by a slow tapering of the anticholinergic dose. The presence of other acute extrapyramidal adverse effects, such as parkinsonism, may warrant a longer duration of anticholinergic therapy.2 Long-term anticholinergics in schizophrenia patients on antipsychotics may have detrimental effects on cognitive function and quality of life.48 Therefore, current guidelines generally discourage the preventive or long-term use of anticholinergics in this population.48 A meta-analysis showed that diphenhydramine prophylaxis reduces extrapyramidal symptoms in patients receiving antiemetic as a bolus, but not as an infusion; hence, this meta-analysis suggested that the optimal strategy would be to give the antiemetic as an infusion without anticholinergic prophylaxis.32
Prognosis and effect on life
The prognosis and long-term effects of medication-induced acute dystonia depend on several factors, such as the type, dose, and duration of the offending drug, the age and genetic susceptibility of the patient, and the presence of other neurological or psychiatric conditions. In general, Dystonic reactions are rarely life-threatening,2 The adverse effects often cause distress for patients and families, but it usually responds well to treatment.13
The impact of medication-induced acute dystonia on quality of life is variable and depends on the severity, frequency, and psychological and social consequences. Some patients may experience anxiety and fear, as well as embarrassment or stigma, which may eventually lead to depression due to their dystonic symptoms.22,45 They may also have difficulties with daily activities, work, education, or interpersonal relationships.22 Therefore, it is important to provide adequate education and support to these patients and their caregivers.49
Conclusion
Medication-induced acute dystonia is a serious and distressing condition that affects many patients who use antipsychotic drugs. This field faces many challenges and limitations, such as the lack of standardized criteria, guidelines, and protocols, the variability in clinical presentation and response to treatment, and the potential for misdiagnosis and adverse outcomes. Future research should explore the genetic and environmental factors that influence the susceptibility and severity of dystonia, evaluate the efficacy and safety of available drugs that can prevent or treat this condition, and improve the awareness, education, and care of patients who suffer from this condition. This topic is important and deserves more understanding and recognition.
References...