Article topic: Lumbar Puncture.
Author: Abdulelah Majdi Fehmi Otoum
Editors: Almutazballlah Qablan, Sadeen Eid
Reviewer: Omar Sanduka
Keywords: Spinal tap, Headache, Back pain, CSF
Overview
Lumbar puncture (LP) or spinal tap, is a procedure in which a needle is inserted into the lower back in order to obtain cerebrospinal fluid (CSF) sample from the subarachnoid space. 1 It’s used to help in the diagnosis of disease, measuring the CSF pressure, or providing treatment. 2
The first lumbar puncture was reported in the late 19th century 3 by the German Heinrich Irenaeus Quincke (1842 – 1922).4 In 1872 he demonstrated how the CSF flows in rabbits and dogs, by injecting red mercury sulfide into the subarachnoid space.5
Two decades later, Quincke presented his report to the Tenth Congress of Internal Medicine at Wiesbaden. Under the name of Ueber hydrocephalus, he mentioned 3 cases: 6
- Treated in 1888, a case of a 12 year-old-boy who underwent 6 ventricular punctures but eventually died.
- Treated in 1890, a case of a comatose boy nearly two years old with the suspicion of TB- meningitis. 3 LPs were performed at three-day intervals.
- Treated in 1891, a case of a 25-year-old man with hydrocephalus was relieved by an LP.
Procedure
A lumbar puncture consists of multiple steps, most of which are easily understood. On average, the procedure takes about 45 minutes.1 Prior to the procedure, the physician will discuss its details with the patient, inform them of the risks & benefits and obtain written consent.3 During a lumbar puncture a sedative could be given to ensure relaxation of the patient. Then, the following steps are applied: 6,7
- The patient is placed in a chest-knee position. The back is cleaned with an antiseptic solution. Then, a local anesthetic is given to numb the surrounding area where the needle is given.
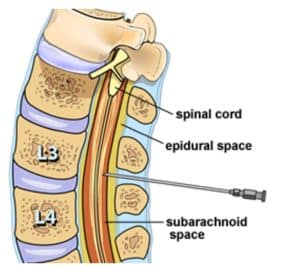
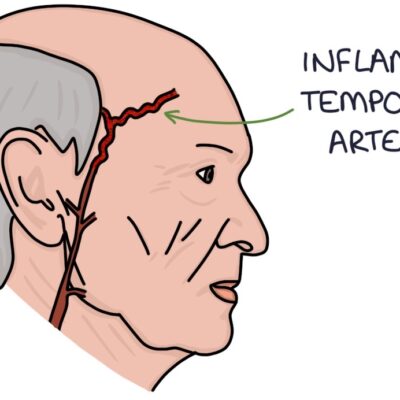
Figure 1. A needle is placed in the subarachnoid space at the level between the third & fourth lumbar vertebrae to collect a sample of cerebrospinal fluid. (6)
- A hollow needle is inserted into the patient’s back, between the third and fourth lumbar vertebrae (L3-L4) to avoid damaging the spinal cord; Figure 1. Slight pressure or a burning sensation might be felt during needle insertion.
- About 5-20 ml of CSF is collected in 2-4 tubes. Depending on the situation the physician might also measure the patient’s CSF pressure, inject a drug, or insert a lumbar drain.
- Finally, the needle is removed, a bandage is placed on the puncture site, and the tubes are sent to the laboratory.
Anatomy:
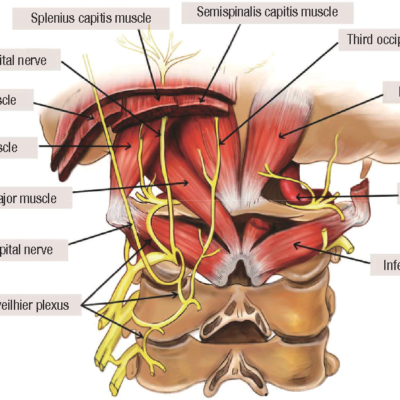
The anatomical order in which the needle in a lumbar puncture passes through goes as follows: 3 (Figure 2-3)
1- Skin.
2- Subcutaneous (SC) tissue.
3- Supraspinous ligament.
4- Interspinous ligament.
5- Ligamentum flavum.
6- Epidural space.
7- The subarachnoid space.
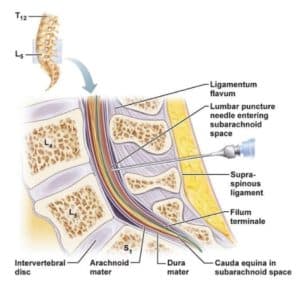
Figure 3. Anatomical site of the lumbar puncture. (15)

Figure 2: Cadaveric sagittal section through lumbar spine showing proper needle trajectory. (3)
Clinical Applications
Lumbar punctures are both diagnostic and therapeutic, as they can aid the diagnosis of multiple conditions6,4; Table 1. Nevertheless, multiple factors are considered before performing a lumbar puncture. These include the clinical presentation, lab values, and local and/or national guidelines.4
In patients with febrile seizures, the prevalence of meningitis and encephalitis is relatively low (9 out of 148).9
Table.1 Demonstrates the diseases which can be diagnosed via lumbar puncture.4
| Infectious diseases | Bleeding | Inflammatory conditions | Other conditions |
| Meningitis | Subarachnoid Hemorrhage | Guillain-berry syndrome | Reye syndrome. |
| Encephalitis | Multiple sclerosis | Pseudotumor cerebi (Benign intracranial hypertension) | |
| Neurosyphilis | Normal pressure hydrocephalus | ||
| Myelitis |
Contraindications
In certain settings, an LP should be avoided due to the high risks and co-morbidities resulting from the procedure:
- Dual Arterio Venous Fistula (DAVF): It has been shown that DAVF could mimic the signs and symptoms of benign intracranial hypertension (BIH), a condition relieved by performing a lumbar puncture. 3 cases were reported of patients deteriorating after LPs, two of them had DAVF type II (a + b), and the third was type II (a) DAVF.8
- Use of antiplatelet agents:
| Salicylic acid: |
| Do not discontinue prior to performing an LP. |
| Clopidogrel or dual antiplatelet therapy: |
| High thrombotic risk
Emergency LP – Perform LP Elective LP – Continue antiplatelet therapy. |
| If clopidogrel is given alone consider replacing clopidogrel with aspirin and perform LP one week after replacement. |
| If dual therapy is being used continue it and consider postponing LP and performing it when aspirin alone is possible. |
- Anticoagulant therapy: performing LP on a patient on an anticoagulant medication is risky due to susceptibility to hemorrhage, hematoma, and thrombosis from drug interruption.10 (Table 2-4) demonstrates the recommendation to do an LP in these patients with regard to drug pharmacology, urgency, and thrombotic risk.10 It is worth mentioning that this is a controversial topic with various perspectives, but for
the sake of clarity we mainly focused here on the patient’s own
bleeding risk, family history, the drug used, and other
factors. - Space-occupying lesion: In an emergency setting, when urgent LP is needed, it is recommended to perform CT or MRI imaging to space-occupying lesions. Signs & symptoms caused by lesions and/or hydrocephalus might be worsened with LP. Cases have been reported to have deteriorated after urgent LPs in the ER.11
Complications:
- Post-dural puncture headache (PDPH): According to the international headache society (IHS), a PDPH is defined as a headache that manifests 5 days after the performance of a lumbar puncture due to CSF leakage in the dura matter.12 This type of headache is common after LPs. Therefore, it is preferred to use a thin, atraumatic needle for this procedure.13
Others: Numbness, back pain, local swelling, hemorrhage, and brain stem herniation. 1,6,14
Table 3. Recommendation for performing (LP) in patients treated with injectable anticoagulants.10
| Intravenous heparin |
| Perform LP 4 hours after heparin discontinuation or once activated partial thromboplastin time (aPTT) is in the normal range. |
| Unfractionated subcutaneous heparin |
| Perform LP 4–6 hours after the last dose of subcutaneous heparin. |
| Subcutaneous low molecular weight heparin (LMWH) |
| Perform LP 12 hours after the last dose of LMWH. In patients with renal insufficiency and in patients using therapeutic doses of enoxaparin, this time should be prolonged to 24 hours. |
Table 4. Recommendation for performing lumbar puncture (LP) in patients treated with oral anticoagulants.10
| Warfarin (Marevan® or Coumadin®) | NOACs (Dabigatran-Pradaxa®, Rivaroxaban-Xarelto®, Apixaban-Eliquis®) |
| High thrombotic risk
1- Emergency LP – Perform LP. 2- Elective LP – Replace warfarin (bridging therapy) 5 days prior to LP: In normal renal function – replace with therapeutic LMW heparin and perform LP 12 hours after the last dose. In impaired renal function – replace with therapeutic unfractionated heparin and perform LP 6 hours after the last dose. Low thrombotic risk 1- Emergency LP – Consider rapidly reversing the warfarin effect and perform LP as soon as INR is 1.5 or below. 2- Elective LP – Discontinue warfarin for 5 days before LP. |
High thrombotic risk
1- Emergency LP – Perform LP (postpone one day if possible) 2- Elective LP – Replace (bridging) NOAC for at least 1 day with normal renal function and 3 days with impaired renal function. In normal renal function – replace with therapeutic LMW heparin and perform LP 12-24 hours after the last dose. In impaired renal function – replace with therapeutic unfractionated heparin and perform LP 6 hours after the last dose. Low thrombotic risk 1- Emergency LP – Perform LP (postpone one day if possible) 2- Elective PL – Discontinue NOAC for 1 day if normal renal function and 3 days with impaired renal function. |
NOACs: new oral anticoagulants; LMW: low molecular weight.