Article topic: Blepharospasm
Authors: Noha el Masri, Rawan Chazbek
Editor: Lubna AL-Rawabdeh
Reviewer: Ethar Hazaimeh
Keywords: Blepharospasm, Dystonia, Botulinum Toxin, Blink reflex
Overview
Dystonia refers to a movement disorder causing intermittent or sustained muscle contraction, resulting in repetitive movements or postures. Dystonia can affect any body part whether an isolated region (focal dystonia) or multiple regions [1]. The most common types of dystonia are the ones involving one region of the body such as cervical dystonia in the neck, blepharospasm around the eyes, and writer’s cramp in the upper limb [2].
Blepharospasm is a form of focal cranial dystonia characterized by sustained, involuntary spasms of the muscles around the eyes (orbicularis oculi, corrugator, and procerus muscles). Symptoms can range from increased blinking to forceful eyelid closure leading to functional blindness (difficulty opening the eyes) [3].
It is sometimes referred to as benign essential blepharospasm when it occurs as an isolated condition. However, blepharospasm usually occurs with other types of focal dystonias such as oromandibular, facial, lingual, or oral dystonia… the co-existence of blepharospasm and oromandibular dystonia (involving oropharyngeal and jaw muscles) is called Meige syndrome [4].
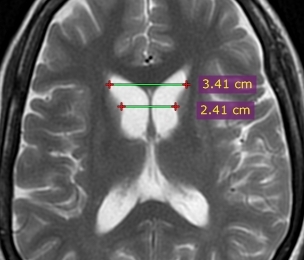
The pathogenesis of blepharospasm is not fully understood yet. The main problem in many types of dystonia is traditionally thought to be dysfunction of the basal ganglia. However, a growing body of evidence suggests the involvement of a network of other cortical and subcortical structures [5].
Treatment is based on symptom severity with botulinum toxin injection being the current first-line therapy, yet there are other medical and surgical options [4].
Introduction
The hallmark of blepharospasm is uncontrolled spasms in the orbicularis oris. However, it may involve other periocular muscles and even muscles of the face. In addition, the patients may present with non-motor manifestations including psychiatric and sensory disturbances [6].
Etiology
Studies suggest that blepharospasm has a multifactorial etiology. Multiple genes may be implicated, in addition to epigenetic and environmental factors that combine to induce the condition [6]. 25% of patients with blepharospasm have at least 1 family member having dystonia. The suggested pattern of inheritance is autosomal dominant with reduced penetrance [6].
Hypotheses suggest that phenotypic expression of blepharospasm and penetrance in individuals carrying susceptibility genes depends on the type and duration of environmental exposure, sunlight intensity may be an example [7].
On the contrary, secondary blepharospasm is usually caused by lesions affecting many brain regions including the thalamus, basal ganglia, cerebellum, midbrain, and cortex… which provides clues on the origin of the condition [6].
Neuropathology
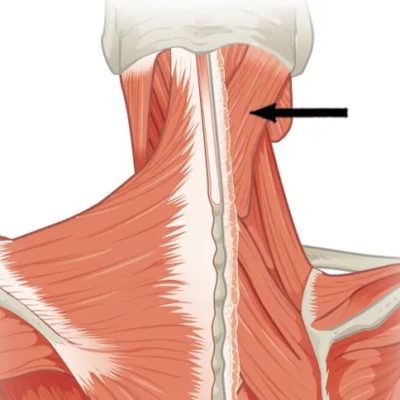
Current (theories) argue that blepharospasm results from defects in neural circuitry rather than defective single locus [3]. These abnormalities include loss of inhibition in many levels of the central nervous system, abnormal sensory-motor integration, and maladaptive plasticity. Yet it is still unclear how each abnormality is responsible for specific motor symptoms [6].
Early hypotheses suggest that descending pathways from basal ganglia might be responsible for the hyperexcitability of brainstem interneurons involved in the blink reflex. Subsequent studies doubted this concept by showing thalamic lesions causing blepharospasms that are not in areas receiving striatopallidal input (from basal ganglia) but receiving cerebellar afferents. Other studies propose that cerebellar lesions might lead to blepharospasm by causing loss of inhibition of the primary motor cortex [5].
![Figure 1 displays a simplified schematic diagram of a corneal reflex arc.[34] Khan Z. A. (2021),](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7886525/bin/PRM2021-6664736.001.jpg)
Figure 1 displays a simplified schematic diagram of a corneal reflex arc.[34] Khan Z. A. (2021),
Clinical manifestations and Complications
Motor manifestations
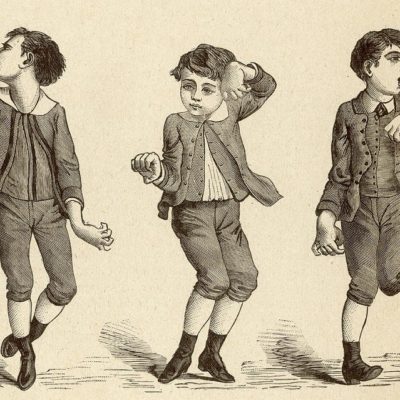
The most common symptom of blepharospasm is orbicularis oculi muscle spasms that are synchronous and bilateral [1]. Spasms can be transient or prolonged, and they can cause the eyelids to constrict or close [9].
Another manifestation that happens in some individuals is apraxia of eyelid opening (AEO). This symptom manifests as difficulty in opening the eyes and is caused by spasms of the pretarsal orbicularis oculi muscle [1]. It might also be present due to the failure of contraction of the levator muscle [6].
The contraction of the orbicularis oculi can also spread and extend to the muscles of the lower face and neck causing what is known as Meige Syndrome [1].
Non motor manifestations
Sensory manifestations can occur in blepharospasm, including burning and grittiness in the eyes, discomfort, and sensitivity to light and dry eyes [9].
The frequency of depression, obsessive-compulsive disorders, and mild cognitive disturbances is higher in subjects with blepharospasm, yet it does not correlate with the severity of motor signs [6]. This cognitive impairment has been reported in the fields of working, memory, processing speed, visual-motor ability, and short-term memory reflecting the changes in the cortical and subcortical areas of the brain [10].
Sleep impairment has also been reported in blepharospasm cases. However, it is unclear if the disturbance is due to the depression associated with the blepharospasm or if it is present as an entity by itself [6]. An association has been found between blepharospasm and abnormal sleep-wake patterns [11].
An additional feature in this subtype of cranial dystonia is the presence of abnormal dystonic eye movements during sleep but with lower frequency and duration [6].
Exacerbating and Relieving factors
Blepharospasm tends to be exacerbated with activity such as walking, driving reading, watching television, Enhanced light, Fatigue, stress, feeling sick, and dry eye symptoms also tend to cause an exacerbation of the symptoms [1][12].
On the other side, blepharospasm tends to be alleviated with relaxation, talking, and even when focusing on tasks. It is also relieved after sleeping, at nighttime, by looking down, closing the eyes, and even applying pressure on the temples [12].
Diagnosis
A diagnostic algorithm has been developed to differentiate blepharospasm from other conditions. The first step is to diagnose the presence of bilateral, synchronous, and stereotyped movements of the orbicularis oculi muscle, the presence of a sensory trick, or increased blinking. The following step is the detection of a sensory trigger or an increased blinking [13].
Multiple scales have been available to assess the severity of the blepharospasm. Mainly, we have the Jankovic Rating Scale, the Blepharospasm Disability Scale, the Functional Disability Score, the Blepharospasm Disability Index, and a recent one developed and validated in 2015 by Defazio G, Hallett M, Jinnah HA, and others [3].
The most commonly used one is the Jankovic Rating Scale which assesses the severity and frequency separately by giving a score from 0 to 4 to each of the items with 0 representing the absence of symptoms and 4 representing the most severe symptoms.
Blepharospasm Severity
0=None
1= Minimal, increased blinking present only with external stimuli (e.g. bright light, wind, reading, driving, etc.)
2= Mild, but spontaneous eyelid fluttering (without actual spasm), definitely noticeable, possibly embarrassing, but not functionally disabling)
3=Moderate, very noticeable spasm of eyelids only, mildly Incapacitating
4=Severe, incapacitating spasm of eyelids and possibly other facial muscles
Blepharospasm Frequency
0= None
1= Slightly increased frequency of blinking
2= Eyelid fluttering lasting less than 1 second in duration
3= Eyelid spasms lasting more than 1 second, but eyes open more than 50% of the waking time
4= Functionally blind” due to persistent eye closure (blepharospasm) more than 50% of the waking time [14].
Management of blepharospasm
Botulinum toxins injection
![Figure 2 displays botulinum toxin injection site options for blepharospasm [35]. Hassell, T. J. W., & Charles, D. (2020)](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7232182/bin/toxins-12-00269-g002.jpg)
Figure 2 displays botulinum toxin injection site options for blepharospasm [35]. Hassell, T. J. W., & Charles, D. (2020)
The most common side effect of BoNT is focal muscle weakness, including ptosis and lagophthalmos in blepharospasm. Other side effects include dryness of the eyes, diplopia, chewing weakness, dysphagia, dysarthria, mouth dryness, generalized weakness, allergic reactions, and flu-like symptoms [4].
Oral medications
Multiple oral medications varying in efficacy can be used. These drugs include anticholinergics, benzodiazepines, VMAT2 inhibitors, levodopa, and baclofen. Anticholinergic drugs and benzodiazepines are shown to be the most effective [4].
However, the most common use of these drugs is as an addition to Botulinum Toxins injections or before referring the patient for a more invasive method and in case of refraction to Botulinum Toxins injection [1] [3].
And these medications are known to have multiple side effects, the most important one is dependence on benzodiazepines [4].
Deep brain stimulation
Deep brain stimulation of the Globus Pallidus Internus has been used in multiple forms of medication refractory dystonia. While genetic testing can help guide expectations for hereditary variants of dystonia, the choice to proceed with deep brain stimulation should be based on clinical presentation [17].
In the case of blepharospasm, the use of deep brain stimulation is still limited. However, multiple case reports have proven the efficacy of using deep brain stimulation in the management of refractory isolated blepharospasm and Meige syndrome [18] [19] [20] [21].
A case report has shown the success of deep brain stimulation in treating medically resistant focal tardive blepharospasm. In addition, it has been proved that small pulse widths and high-frequency stimulations can regulate eyelid spasms [22].
Another report has suggested that in contrast to more globalized dystonic phenotypes, isolated cranial blepharospasm requires lower voltage needs and longer pulse widths [23].
Surgery
Surgery is used for the management of blepharospasm in case of refractory disease. It is based on recognizing the function of individual orbicularis oculi portions and the facial nerve branches [24]. The surgery of choice is myectomy, which showed a lower likelihood of recurrence and required fewer additional procedures when compared to facial nerve dissection. In addition, facial nerve surgery showed greater side effects from nerve palsy to regeneration [3].
The commonly used technique is the partial myectomy with correction of blepharospasm impacts on the face. Total myectomy can also be performed but increases the risk of postoperative lymphedema, lagophthalmos, and facial anesthesia [1].
Transcranial magnetic stimulation (TMS)
A repetitive TMS with low frequency aiming at reducing cortical excitability has shown positive feedback from both the subjective patient rating and physician rating and an acceleration in the blink reflex recovery curve based on a pilot study, however, more studies should be made [6] [ 25].
Photochromatic modulation
The wavelength and light intensity both contribute to the photophobia associated with blepharospasm [1]. Yet, photophobia is more triggered by the wavelength than the intensity of the light [26].
Lenses provide an excellent way of symptomatic treatment for this photophobia in blepharospasm patients, especially the FL-41 lens tint [27].
Risk factors
Multiple risk factors have been associated with blepharospasm. The first risk factor is a positive family history since multiple genes have been found to play a role in the development of blepharospasm [28] [29] [1].
The risk of blepharospasm is increased in women and the age group between 40 and 60 [6].
Other important risk factors that are non-inherited such as urbanization and jobs associated with stressful lifestyles [3]. Also, it is associated with increased screen usage and reading, psychiatric conditions, and previous ophthalmic conditions [1][30] [31] [32] [33].
References
References...