Article topic: Benign paroxysmal positional vertigo (BPPV)
Author: Yasmin Dahabreh
Editors: Ainaa A.Alzamari, Hamid Ghanem
Reviewer: Ethar Hazaimeh
Keywords: Benign paroxysmal positional vertigo (BPPV), Canalolithiasis, Cupulolithiasis, vertigo, nystagmus, torsional nystagmus, repositioning maneuvers, Dix-Hallpike maneuver.
Abstract
Background: vertigo is a sensation when the patient feels that the environment or himself is spinning. There are many subtypes of vertigo that are mainly divided into central and peripheral vertigo. BPPV is considered the most common cause of peripheral. Symptoms such as vertical, torsional, and horizontal nystagmus, nausea, and vomiting typically occur. It is attributed to calcium debris that either floats or attaches to the cupula. There are many types but the vast majority are the lateral and the posterior-canal types, hence its diagnosis requires which type is affected so the treatment that includes many maneuvers.
Methods: A systematic review search was done which studied primarily Benign Paroxysmal Positional Vertigo (BPPV) through the literature databases.
Conclusion: Vertigo is caused by a type of balance disorder called BPPV, at least 20% of patients will complain of vertigo during a clinic visit. It is usually misdiagnosed with other diseases. It is also diagnosed and treated depending on the type is injury.
Introduction
Benign Paroxysmal Positional Vertigo (BPPV) is a brief episode of mild to severe dizziness that is induced by changes in head positions. It is one of the most common causes of vertigo; as it accounts for 14–42% of patients presenting with vertigo (1). A patient with BPPV feels like the surrounding environment is spinning, causing a loss of balance, that may associated with vomiting and nausea (1, 2). It can also be defined as transient position-induced horizontal, vertical, or torsional nystagmus (1). BPPV is explained by the migration of otoliths (calcium debris) freely in the endolymph, or collection in the cupula (2). This disease affects elderly women more than other people (3). This type of disorder is usually misdiagnosed with other benign to life-threatening diseases that can cause vertigo (2), such as Ménière disease, unilateral vestibular loss (UVL), vascular loop syndrome, and many others (2). Risk factors for BPPV are osteoporosis, vitamin D deficiency, diabetes mellitus, hypertension, and hyperlipidemia (4). Diagnosis for this disorder depends on the type of canal that is affected (5). There are many types of BPPV but the posterior canal type is considered the most common with (80-90%) incidence among patients, then lateral type (10-20%) and other atypical types (2-3%) (6).BPPV is treated by maneuvers that rely on the type of the affected canal; medication is used for BPPV comorbidities, on the other hand, surgical procedures are used as the last option after long-term ineffective treatment(7).
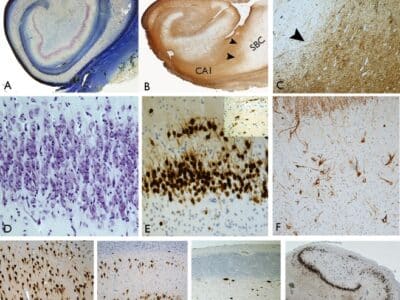
Pathophysiology
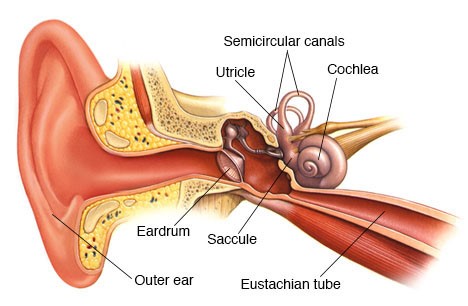
There are two attributed hypotheses to BPPV pathophysiology, which are canalolithiasis and cupulolithiasis. In canalolithiasis, the otoliths move freely in the endolymph (fluid in the semicircular canals normally detects angular head acceleration) because of gravity (8). Due to the viscosity of the endolymph, these particles create a current, which will lead to a cupular displacement. The heavy debris in the canal causes inappropriate movement of the fluid with linear accelerations such as gravity and causes an inappropriately spinning sensation when the head shifts with gravity. The other hypothesis (cupulolithiasis) (9) states that deposits of the otoliths or otoconia collect and adhere directly to the cupula and settle there, making it more responsive to gravity (10). These two mechanisms either increase or decrease the depolarization rate and change the angular head acceleration, which is not supposed to occur in an average person. Canololithiasis probably occurs more commonly than the other hypothesis (10).
Clinicopathologic studies showed that canalolthiasis appeared to be more common in typical BPPV. Other studies have demonstrated that otoconia may be the source of the canaliths by floating in the lumen with and without linking filaments and attached to a gel matrix. Age-related destruction of the gel matrix and the filaments or the otoconia themselves can create an idiopathic BPPV (3). Other theories have been published that suggest bone loss could be the source of otoconia (the calcium deposits). In one study, patients with BPPV had low bone density, and the rates of osteopenia and osteoporosis were higher compared to the control group(11). Therefore, osteoporosis and vitamin D deficiency may increase the risk of BPPV (4,12).
BPPV can be due to a secondary cause such as head injury or inner ear disease that causes a detachment of the otoconia from the utricle or degeneration and uncoupling of otoconia such as sudden sensorineural hearing loss, Meniere’s disease or vestibular neuritis, ear surgery, herpes zoster oticus, and inner ear ischemia (10,13,14). BPPV has the possibility to show during surgeries such as elevating the floor of the maxillary sinus. In rare situations, decompression sickness can be caused due to nitrogen bubbles in the canals. Moreover, it could show in giant cell arteritis (GCA) (15). A survey revealed that BPPV is independently associated with age, hypertension, hyperlipidemia, and stroke(3)
Clinical manifestations
BPPV is divided into many subtypes; these subtypes are further divided into typical and atypical types (9). The typical types consist of the posterior-canal-type (canalolithiasis), lateral-canal-type BPPV (canalolithiasis), and lateral-canal-type BPPV (cupulolithiasis) all of them meet specific criteria according to specific symptoms and signs. On the other hand, the atypical BPPV does not meet the criteria, such as the anterior-canal-type of BPPV (canalolithiasis), the posterior-canal-type of BPPV (cupulolithiasis), and the multiple-canals-type of BPPV (9).
Patients with BPPV usually present with multiple vertigo episodes, which are described as dizziness, passing out, ringing in the ear, and torsional, vertical, or horizontal nystagmus that last for one minute or less, depending on the type of BPPV which can happen more than once in weeks or months. It can be provoked by changing head positions, such as looking upward while standing, sitting, or in a supine position. These episodes may be associated with vomiting or nausea. Most importantly, it is important to mention that there is no neurological or hearing loss in this type of disorder. Some have reported the presence of inner ear damage before BPPV. Fifty percent of the patients complain of imbalance between attacks even after treatment. Clinicians can observe gait disturbances and the appearance of nystagmus (10,16).
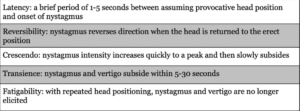
Table (1): Definitions of Findings supporting the Diagnosis of Benign Paroxysmal Positional Vertigo (10).
Diagnosis
A detailed history should be taken in order to diagnose BPPV. Provoking maneuvers are being used in the physical examination with a typical history of BPPV. These maneuvers can help by triggering nystagmus to occur thus it can manifest the canal in which the ear is affected (17).
Dix-Hallpike is the diagnostic maneuver for some types of BPPV; this maneuver has around 55 to 80% effectiveness and sensitivity in diagnosing BPPV (18). When performing this maneuver, the patient should be seated so that their head would be over the edge of the table when they reclined back to supine. They should then perform a 45-degree cervical rotation toward the test side, lie down, and allow their head to move 30 degrees off the edge of the table while being watched for nystagmus. Nystagmus can have latency and not be present immediately so the physician should assess the nystagmus for at least 30 after finishing the test (19).

Fig1. Dix-Hallpke maneuver, The physician stands the patient to the right side and rotates his head 45 degrees to the right, Then the patient moves from the sitting to the supine position where the right ear position and the patient’s neck are slightly upward. The latency, duration, and direction for both nystagmus and vertigo should be noted. The free-floating debris is thought to cause this type of disorder.
In typical posterior-canal BPPV, the nystagmus will be upward vertical or torsional nystagmus, in which the eye rotates in the direction of the affected ear. Torsional nystagmus where the eyes can rotate to the unaffected ear can be induced by the reverse Dix-Hallpike maneuver where the patient is brought back to the upright position (9). This nystagmus lasts less than one minute, is characterized by an increase then decrease in intensity, and is diminished after repeated head positioning (9,20).
A typical posterior type BPPV has the same diagnostic features it has a longer duration of vertigo that lasts for more than a minute (21). On the other hand, the atypical anterior canal BPPV is different from the typical BPPV by having downward vertical and torsional nystagmus (22).
If this maneuver was ineffective, meaning there was no nystagmus, or it showed horizontal nystagmus, that may indicate another type of BPPV, such as lateral type BPPV(23); in this situation, another maneuver should be applied(23). The most known one is the horizontal roll maneuver, when performing this maneuver; the patient will be lying on their back with their neck flexed by 30 degrees and their head rotated to the left or right by around 90 degrees. A positive Horizontal roll maneuver represents dizziness or rotatory vertigo due to changes in head positions relative to gravity (9). This vertigo has a short duration of less than one minute, described as an increase and then decrease in intensity, which can still decrease after multiple head positions (9).
This type is characterized by a geotropic nystagmus where the nystagmus is beating fast toward the ground and slow beating when it returns back after eight seconds of turning to the affected ear. In geotropic nystagmus, the affected side is the side where it has severe symptoms, for example, rightward horizontal nystagmus is induced by turning the head to the right ear if the right ear is the affected one (24,25). The nystagmus consists of major horizontal and minor torsional components (26).
If the patient has the atypical lateral BPPV, the previously mentioned maneuver will provoke a vertigo attack by specific head positions, this attack will last for more than one-minute duration (21). The intensity is not decreased during the attack (21). This vertigo is not associated with cochlear or other neurological symptoms. During the procedure by apogeotropic positional nystagmus, the pupils move against the ground (toward the ceiling) in fast beating and return to the original position by slow beat (27). It differs from the typical type that the nystagmus is induced toward the less harmful or more severe: leftward horizontal nystagmus indicates that the right ear is affected. The nystagmus consists of minor and major torsional components. They don’t appear with latency and last for more than one minute. Peripheral and central vestibular diseases that cause vertigo are ruled out (26).
There is a better way to diagnose lateral type by bow and lean, where the patient flexes his neck and then tilts the head backward, in this test, the horizontal canal will first align with the gravity before turning 180 degrees horizontally. Hence, the right nystagmus has a right beat toward the bow, and the left beats toward the lean (28).
Differential diagnosis
According to a study, 36 causes of nystagmus of the BPPV type were found to be due to other causes rather than the presence of canalolithiasis /cupulthiasis (10).
Table(2). The cases where the BPPV-type positional nystagmus and vertigo were caused by other disorders (Pseudo-BPPV) (10).
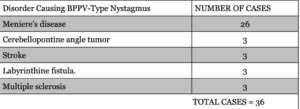
Table(2). The cases where the BPPV-type positional nystagmus and vertigo were caused by other disorders (Pseudo-BPPV) (10).
As the table demonstrated these cases were not reported as BPPV. For example, in cases where the positional nystagmus showed during or shortly after Meniere’s disease, it indicates they are a manifestation of Meniere’s disease (10). Cases of stroke and cerebellopontine angle tumor are considered pseudo-BPPV or diseases associated with BPPV (true BPPV) diseases could be similar to BPPV, such as postural or orthostatic hypotension, because both can cause dizziness that is stimulated by changing positions (29, 30). However, patients with orthostatic hypotension describe their dizziness as faint rather than vertigo, whereas 90% of BPPV patients have these symptoms. In addition, this kind of hypotension is not provoked by rolling down or BPPV maneuvers (29, 30).
Chronic unilateral vestibular hypofunction or unilateral vestibular loss (UVL) is where there is a loss in the vestibular function of the ear. This disease is associated with transient dizziness after rapid head turns, but this vertigo lasts only for two seconds, in the BPPV case, it lasts from 30 to 60 sec and does not require rapidity of head turns. Also, BPPV maneuvers are not a problem for UVL patients (31).
Labyrinthitis or vestibular neuritis, where there is an inflammation of the labyrinth or vestibular nerve, respectively, can also present with a nystagmus that is similar to BPPV (32-35). Other brain lesions such as stroke, Arnold-Chiari malformation, multiple sclerosis, cerebellar degeneration, ischemia, intoxication, Acoustic neuroma, and meningioma, can induce the appearance of nystagmus (32-35).
Meniere’s disease is a rare inner ear disorder. A report was published and believed that it is one of the other disorders that can cause BPPV-Type Positional Nystagmus and Vertigo. The distinction between Meniere and BPPV is based on history, vertigo, and symptomatology (10).
Vestibular migraine is a type of migraine where people experience a combination of vertigo and dizziness, and it can present as isolated positional vertigo, such as BPPV. Symptoms duration can be used as a distinctive feature because it usually lasts for hours, but in rare cases, it could last for a few seconds to a few minutes (36). retrospective review of 362 patients with positional vertigo where 10 patients were identified by vestibular migraine and distinguished from BPPV by having a shorter recurrence time (it is more likely to happen over hours to days rather than weeks to months (37). It targets younger patients usually (37). Moreover, its symptoms are often difficult to describe during vertigo episodes (37). Finally, positional nystagmus is atypical for BPPV.
Treatment
Treatment of BPPV relies on repositioning maneuvers, and it is crucial to not delay the treatment because the quality of life would be significantly affected (38). Repositioning maneuvers are the best evidence-based method for treating BPPV. Making the correct diagnosis and determining the affected side and the canal are very important in the treatment process (38, 39).
A typical posterior canal type is treated by physical theory. Its advantages are clearing the posterior canal of the floating debris and encouraging migration to the utricle, where otoconia are typically reabsorbed (40). Semont’s Liberatory Maneuver and Epley’s Canalith repositioning maneuver have good results and efficacy based on trials with a 90% success rate. Also, it is not dependent on the patient’s age and pre-existing neurological disorders (39, 40).
The Modified Epley Maneuver, also known as the Canalith Repositioning Maneuver (CRM), comprises five phases, each lasting three minutes, designed to transfer the otoconia sequentially from the posterior canal to the common crus and finally to the vestibule(41). It starts with a patient on the bed with the head rotated to the left for the left posterior canal about 45 degrees, then quickly moved to the Dix-Hallpike position with the affected ear downward, then the head is rotated 90 degrees toward the unaffected side, causing the movement of the debris in an ampullofugal stimulus and keeps rotating the head with 90 degrees toward the right causing the otoliths to exit the canal. Finally, the patient is slowly moved to the sitting position. An upward nystagmus with a torsional component toward the affected ear indicates that the maneuver worked successfully because it shows that the particles have left the posterior canal through the common crus (42).

Figure (2). Epley’s maneuver for left posterior canal BPPV. 1 the patient is on the bed with the head rotated 45° to the left side. 2. The patient is then moved quickly into the Dix-Hallpike provoking position with the affected ear downwards. 3. Slowly rotate the head 90 degrees toward the unaffected side. 4. the head and the trunk are moved 90 degrees to the right causing movement of debris and exit Canal, finally the patient is slowly moved into a sitting position(not represented in this fig)
The other maneuver that treats atypical type of posterior canal is the Liberatory or Modified Semont Maneuver where a rapid tilt of 180 degrees to the posterior canal plane emits the otoconia from the posterior canal by centrifugal force. For a left posterior canal BPPV, the patient should swiftly lean to the side that is affected while rotating their head 45 degrees to the right and hold that position for one minute(43). Free-floating otoconia moves toward the lower portion of the canal, causing an ampullofugal flow that, after a little latency, a typical positional nystagmus is triggered. The patient is then immediately (within 1.5 s) rotated into a right side-lying position with the nose down, creating an endolymphatic flow and a rotatory nystagmus beating towards the highest right ear. A reversed nystagmus indicated that this maneuver failed as a prognostic factor (44).In addition, the speed of rotation is critical to get the best results of this procedure because if it was performed slowly it could be ineffective because the debris can fall back into the canal (45).
In clinical practice, results have shown that Epley and Semont’s maneuvers have the same efficacy (46). Attacks tend to recur 10–20% of the time in the first two weeks, requiring one to three repetitions of the same treatment or choosing a different repositioning strategy (46). Other shorter maneuvers are proposed now to treat this type, such as the “Chair-based Abbreviated Reposi- toning Maneuver (ChARM) (47).
Horizontal type (HC) BPPV is classified into two subtypes that can be identified by their specific positional nystagmus. The more common is characterized by geotropic nystagmus, and the less common presenting apogeotropic nystagmus (48). This type is treated by modified Gufoni’s maneuver which is performed on the affected ear with the patient’s head turned 45° upward, then swiftly positioned it from sitting position to the affected side. The head is then turned 90 degrees toward the healthy ear (nose up). After that, the head should rolled to the unaffected side once the entire body is placed in the supine posture. The patient is then returned to a sitting position with the head tilted slightly forward. The head is then rolled to the unaffected side once the entire body is placed in the supine posture. The patient is then returned to a sitting position with the head tilted slightly forward. Each position should be held for three minutes (49).
On the other hand, the geotropic nystagmus (canalithiasis) is treated by the barbecue rotation maneuver (BBQ) (50). This maneuver is aimed to remove free otoconia from the HC by using centrifugal force; the patient is rotated 90 degrees in the direction of the healthy ear at a time. The procedure is not comfortable for obese, elderly, or motion-restricted patients (50). Gufoni’s maneuver can also be used, which allows the otoconial debris to exit the canal under the centrifugal force created by the rapid deceleration. An alternative maneuver is the forced Prolonged Position (FPP) which is advised for obese, elderly, and patients with restricted movement. In this way, otoconial debris can leave the canal under gravity (51, 52).
Anterior BPPV is treated by reverse Epley/Epley, and Yacovino maneuvers are the most widely used treatments for acBPPV with the advantage that Yacovina does not require the affected side to be known (53). It consists of four movements separated by 30-s intervals: the patient is moved first from sitting to a supine head-hanging position, then the head is tilted where the chin is the chest, and last, the patient sits up. The outcome of Yacovian depends on the duration of the downward nystagmus beat. Patients with nystagmus that lasts for less than one minute have better effects (54). Self-administered treatment is not recommended because the recurrence may not arise in the same canal (55).
Vestibular suppressant medications, such as antihistamines and benzodiazepines are not recommended treatments in acute BPPV (39). Otherwise, medication is helpful for comorbidities that may have developed before or after BPPV that decrease the quality of life, such as anxiety/depression and residual dizziness are frequent findings in BPPV patients. Hence Anti-vertiginous, anti-anxiety, and antiemetic drugs may be used (55).
In some cases, a normalized vitamin D serum is used to treat patients susceptible to detachment of otoconia from the utricular macula with low serum vitamin D levels and disorders of bone metabolism (56,57).
In severe cases, continuous BPPV may be treated by surgical procedures that can be safe and effective, but it should be recommended after a thorough follow-up when there have been no recurrences in other canals or when both sides are affected (58).
Conclusion
Benign positional paroxysmal vertigo is an inner ear disorder. Symptoms are characterized by a repeated brief attack of vertigo or dizziness that differs according to which type the patients have. There are many diseases that appear to be similar to BPPV in presentation, such as Meniere’s disease. The diagnosis and treatment rely on the repositioning maneuver, which varies depending on the affected side.
References
References...