Topic: Progressive Multifocal Leukoencephalopathy (PML)
Author: Heba Allah Zuhair Huaishan
Editor: Abdel Rahman Bani Yassin, Ihda Bani Khalaf
Reviewer: Ethar Hazaimeh
Key words: JCV, PML, Progressive, multifocal, leukoencephalopathy, double-stranded DNA
Introduction
Progressive multifocal leukoencephalopathy (PML) is a rare and frequently deadly viral infection marked by progressive harm or demyelination of the brain’s white matter at various sites1
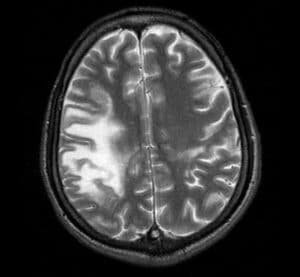
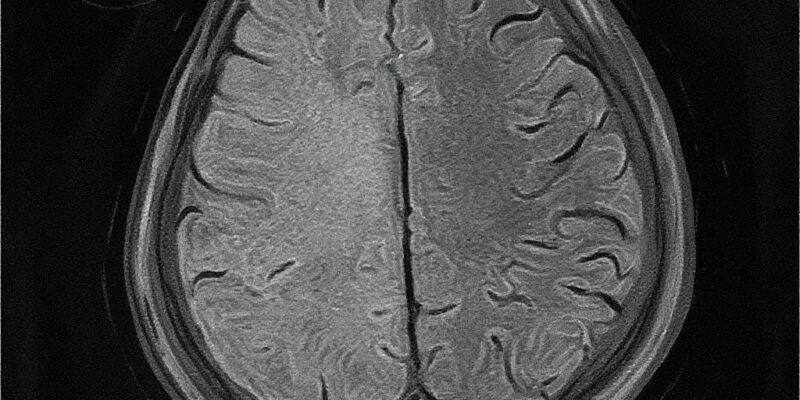
Figure 1: PML under MRI2
It is induced by JCV (John Cunningham virus), named after the initial patient in whom it was found3. The JC virus typically remains latent and is controlled by a healthy immune system. Thus, it is a benign disease unless the immune system is weak3.
Epidemiology
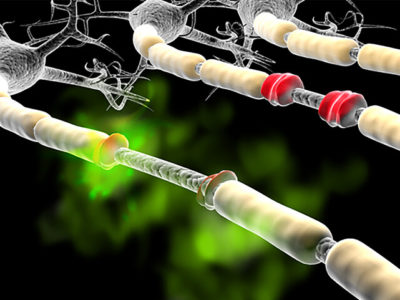
JCV, a double-stranded DNA genome, is a polyomavirus with a circular structure (Figure 22. Research on blood samples has shown that JCV infects children without causing symptoms before the age of 5. Moreover, approximately 85% of individuals are found to have antibodies against JCV by the time they reach adulthood5. After the initial infection, JCV remains dormant in various locations such as the kidney, bone marrow, and tonsils. However, it is uncertain whether JCV also becomes latent in the central nervous system. In immunocompetent individuals, JCV reactivation typically occurs without any noticeable symptoms6.
Etiology
PML primarily affects individuals with significant immune suppression, most commonly among patients with acquired immune deficiency syndrome (AIDS). However, people on chronic immunosuppressive or chemotherapeutic medications, such as patients with transplants, Hodgkin’s lymphoma, multiple sclerosis, psoriasis, rheumatoid arthritis, and other autoimmune diseases, are also at increased risk of PML7.
Classic PML: PML usually presents with subacute neurologic deficits, including altered mental status, motor deficits (hemiplegia), limb ataxia, gait ataxia, and visual symptoms such as hemianopia and diplopia. PML may be asymptomatic in its earliest stages8.
Inflammatory PML (PML-IRIS): Some patients with reversible immunosuppressive causes may experience an inflammatory response in PML lesions, termed immune reconstitution inflammatory syndrome (IRIS), and associated with new onset or clinical worsening of PML and with brain PML Lesions on Magnetic Resonance Imaging (MRI)8 PML-IRIS mainly occurs in HIV patients receiving antiretroviral therapy, and these patients have a significant increase in CD4+ T cell counts and a decrease in HIV plasma viral load, indicating a recovery of the immune system8. Multiple sclerosis patients treated with natalizumab may develop PML and then PML-IRIS after discontinuation of natalizumab and restoration of the immune response9.
Clinical Manifestations
Progressive multifocal leukoencephalopathy, or PML, is a rare but serious brain infection that mostly affects people with weakened immune systems. The symptoms can vary depending on which part of the brain is involved, but they often start subtly—maybe some clumsiness, trouble speaking, or weakness.10 As the disease progresses, people might experience vision problems, memory loss, or personality changes. In those with AIDS, it can also affect walking, speech, and even eye movement.
In recent years, patients on immunomodulatory therapies (e.g., natalizumab) represent the second-largest group at risk for PML, after individuals with AIDS. Diagnosing PML used to require a brain biopsy, but that’s rarely done today. Instead, doctors usually look for signs of the JC virus—the virus that causes PML—in spinal fluid, along with brain scans and symptoms. The good news is that if the immune system can recover, the outlook for people with PML has improved significantly.11
– Focal neurological deficits: hemiplegia, aphasia, ataxia3.
– Seizures3.
– Impaired concentration3.
– Isolated encephalopathy, dementia, altered mental status, and altered behavior are rare, but focal neurologic deficits may be present12.
Diagnosis
PML can be diagnosed in a patient when the disease shows a progressive course. Diagnosis involves finding JC virus DNA in cerebrospinal fluid (CSF) along with consistent white-matter lesions observed on brain magnetic resonance imaging (MRI)9. Alternatively, a brain biopsy can be diagnostic if it reveals typical histopathology of demyelination, bizarre astrocytes, and enlarged oligodendroglia nuclei, coupled with techniques that indicate the presence of the JC virus9.
Characteristically, on brain CT scan images, PML presents as multifocal, non-contrast-enhancing hypo-dense lesions without mass effect8. However, MRI is considerably more sensitive than CT in detecting these lesions12. The cortical white matter of the frontal and occipital lobes is the most commonly affected area in PML, although lesions may appear anywhere in the brain, including the basal ganglia, external capsule, brain stem, and cerebellum13. It’s worth noting that natalizumab-associated PML often manifests as monofocal lesions, predominantly found in the frontal lobe13.
Lab results
- CD4 count: typically, < 2002,8
- CSF analysis:-
- CSF PCR; JC virusDNA2
Brain biopsy findings
- The classic triad consists of
- Enlarged oligodendrocyte nuclei with intranuclear inclusions Figure 3
- Demyelination Figure 42
- Bizarre astrocytes12.
Treatment
Currently, it mostly affects people with weakened immune systems.14 The virus damages the protective covering of nerve cells in the brain, leading to a range of neurological problems. The best way to manage PML is by helping the immune system recover and fight back. Unfortunately, if the immune system can’t bounce back, the outlook can be quite poor. There are no drugs available that can effectively inhibit or cure the virus infection without causing toxicity8. As a result, the primary goal of treatment is to reverse the immune deficiency and thereby slow or halt the progression of the disease13. For patients who are on immunosuppressive medications, this involves discontinuing those drugs or using plasma exchange to expedite the removal of the biologic agent that may have put the individual at risk for PML12.
Given the limitations in direct antiviral treatments, the approach to managing PML is primarily supportive. This includes treating seizures when they occur and, in the case of patients with HIV, initiating antiretroviral therapy (ART) or highly active antiretroviral therapy (HAART) immediately to boost the immune response and combat the virus effectively12.
Overall, the current therapeutic strategies mainly focus on providing support and managing associated complications, while efforts to find more effective and targeted treatments continue to be an important area of research13 Experimental treatments such as pembrolizumab or mefloquine are under investigation but lack definitive evidence.

Figure 5: Axial CT of the brain demonstrates a large area of low attenuation in the right hemisphere, without evidence of contrast enhancement. It affects the white matter, sparing the cortex.15
Prognosis
Following a diagnosis of PML, approximately one-third to one-half of individuals succumb to the disease within the first few months, the fatality rate varying based on the severity of their underlying condition2. For those who survive, the aftermath can involve varying degrees of neurological disability13.
Conclusion
PML is a viral infection that causes swelling in the brain’s white matter. Induced by JCV and appear when the immune system is weak. There are no drugs available that can effectively inhibit or cure the virus infection without causing toxicity. As a result, the primary goal of treatment is to reverse the immune deficiency and thereby slow or halt the progression of the disease. Prognosis remains poor, particularly in patients with severe immunosuppression, but may improve with timely immune restoration.
References...