Topic: Delusional Disorder
Author: Ghina Mohamad Kaskas
Editor: Ihdaa Mahmoud Bani Khalaf, Sadeen Eid.
Reviewer: Ethar Hazaimeh
Keywords: Delusional disorder, delusions, antipsychotics, paranoid psychosis
Overview
Delusional disorder (DD) is a condition in which a person has monothematic delusions for more than a month. [4] This disorder has multiple names, including paranoia, paranoid condition, paranoid reaction, paraphrenia, paranoid state, paranoid psychosis, and paranoid disorder. [6] The first comprehensive psychopathological description of paranoia was described by Esquirol in 1838 as partial delirium, which, in the end, was named partial psychosis. [10] After that, Kraeplin separated paranoia (precursor of DD) from his dementia praecox category (later named Schizophrenia). [10] He believed that paranoia had an endogenous cause. [5] Paranoia/paranoid psychosis was then renamed by Winokur in 1977 as Delusional disorder. [6]
Sérieux and Capgras postulated a hypertrophy of attention in which the individual focuses on particular issues to the exclusion of other issues. [2] Kauffman investigated this in 1981 with people with delusions, finding true experiences at the root of delusion-like experiences. [2]
Epidemiology
This condition is underreported so the frequency in the population is not known. It usually presents the psychiatric facilities only when the person becomes litigious or criminal. [10] The estimated lifetime prevalence for DD is 0.2% in the general population and around 2-3% in patients with other psychotic disorders. [7] It affects both genders equally. [7]Persecutory DD is the most common type of DD. [4]
Clinical presentation and complications
Since delusions are the main symptom of delusional disorder, we need to clearly define them. According to DSM-V TR delusion is defined as:
Fixed beliefs that are not amenable to change even with the presence of conflicting evidence. Their content may include a variety of themes (e.g., somatic, referential, persecutory, religious, grandiose). [14]
Individuals present with delusions of a specific theme for more than one month, and they’re usually uncooperative with treatment and annoyingly talkative during therapy sessions [2]. They will try to offer evidence to support their belief and get the doctor convinced [2]. They will argue anything presented against them through appeals to coincidence, misunderstanding, or alternative interpretations of facts [2]. An important feature of DD patients is that their personality is intact, and the delusions are encapsulated [2]. DD patients cannot have symptoms of thought alteration, passivity, and negativity [1].
A patient with DD is mostly characterized by:[10]
- An egocentric, narcissistic, self-overrated arrogance.
- A suspicious and negative attitude toward the outside world, which is perceived as hostility, causes the patient to isolate him/herself.
- A propensity for misinterpretations and misjudgments.
- A diminished capacity for social adjustment and flexibility because of the points mentioned above.
Diagnosis
According to DSM-V, the diagnostic criteria are as follows:[14]
A. Presence of one (or more) delusions with a duration of 1 month or longer.
B. Criterion A for schizophrenia is never met.
Note that hallucinations, if present, are not prominent and are related to the delusional theme (e.g., the sensation of being infested with insects associated with delusions of infestation).
C. Apart from the impact of the delusion(s) or its ramifications, behavior is not bizarre or odd and functioning is not impaired.
D. If manic or major depressive episodes have occurred, these have been brief in comparison to the duration of the delusional periods.
E. The disturbance is not due to the physiological effects of a substance or another medical condition and is not better explained by another mental disorder, such as obsessive-compulsive disorder or body dysmorphic disorder.
Specify whether:
- Erotomaniac type: This subtype applies when the central theme of the delusion is that another person is in love with the individual.
- Grandiose type: This subtype applies when the central theme of the delusion is the conviction of having some great (but unrecognized) insight or talent or having made some important discovery.
- Jealous type: This subtype applies when the central theme of the individual’s delusion is that her or his spouse or lover is unfaithful.
- Persecutory type: This subtype applies when the central theme of the delusion involves the individual’s belief that he or she is being conspired against, spied on, cheated, followed, drugged or poisoned, harassed, maliciously maligned, or obstructed in the pursuit of long-term goals.
- Somatic type: This subtype applies when the central theme of the delusion involves sensations or bodily functions.
- Mixed type: This subtype applies when there is no one delusional theme that predominates.
- Unspecified type: This subtype applies when the dominant delusional belief cannot be determined or is not described in the specific types (e.g., referential delusions without a prominent grandiose or persecutory component).
Specify if:
With bizarre content: Delusions are deemed bizarre if they are implausible, not understandable, and not derived from ordinary life experiences (e.g., an individual’s belief that a stranger has removed his or her internal organs and replaced them with someone else’s organs without leaving any wounds or scars).
Specify if:
The following course specifiers are only to be used after a 1-year duration of the disorder:
The first episode, currently in acute episode: The first manifestation of the disorder meets the defining diagnostic symptom and time criteria. An acute episode is a period in which the symptom criteria are fulfilled.
The first episode, currently in partial remission: Partial remission is a period during which an improvement after a previous episode is conserved and the defining criteria of the disorder are partially fulfilled only.
The first episode, currently in full remission: Full remission is a period after a previous episode in which there are no disorder-specific symptoms are present.
Multiple episodes, currently in an acute episode.
Multiple episodes, currently in partial remission. Multiple episodes, currently in full remission.
Continuous:
Symptoms fulfilling the disorder’s diagnostic symptom criteria remain for most of the illness course, with sub-threshold symptom periods being very brief relative to the overall course.
Unspecified
Specify current severity:
Severity is rated by a quantitative assessment of the primary symptoms of psychosis, including hallucinations, delusions, disorganized speech, abnormal psychomotor behavior, and negative symptoms. Each of these symptoms may be rated for its current severity (most severe in the last 7 days) on a 5-point scale ranging from 0 (not present) to 4 (present and severe).
Note: Diagnosis of the delusional disorder can be made without using this severity specifier.
Differential diagnosis:
- Obsessive-compulsive and other related disorders [14]: when a person with obsessive-compulsive disorder is totally persuaded that her or his obsessive-compulsive disorder beliefs are true then the diagnosis of obsessive-compulsive disorder, with absent insight / delusional beliefs specifier, should be given rather than a diagnosis of delusional disorder. Similarly, if an individual with body dysmorphic disorder is completely convinced that her or his body dysmorphic disorder beliefs are true, then the diagnosis of body dysmorphic disorder, with absent insight / delusional beliefs specifier, should be given rather than a diagnosis of delusional disorder.
- Major neurocognitive disorder, delirium, psychotic disorder due to another medical condition, and substance/medication-induced psychotic disorder [14]: Individuals with these disorders may present with symptoms that suggest delusional disorder. For example, simple persecutory delusions in the context of a major neurocognitive disorder would be diagnosed as a major neurocognitive disorder, with behavioral disturbance. A substance / medication-induced psychotic disorder cross-sectionally may be identical in symptomatology to delusional disorder but can be distinguished by the chronological relationship of substance use to the onset and remission of delusional beliefs.
- Schizophreniform disorder and Schizophrenia [14]: Delusional disorder can be distinguished from schizophreniform disorder and schizophrenia by the absence of the other characteristic symptoms of the active phase of schizophrenia.
- Bipolar and depressive disorders and schizoaffective disorder [14]: These disorders may be differentiated from delusional disorders by the temporal relationship between delusions and mood disturbance and by the severity of the mood symptoms. If delusions occur exclusively during mood episodes, the diagnosis is a depressive or bipolar disorder with psychotic features. Mood symptoms that meet the full criteria for a mood episode can be superimposed on the delusional disorder. The delusional disorder can be diagnosed only if the total duration of all mood episodes remains brief relative to the total duration of the delusional disturbance. If not, then a diagnosis of other specified or unspecified schizophrenia spectrum and other psychotic disorders accompanied by other specified depressive disorder, unspecified depressive disorder, other specified bipolar and related disorder, or an unspecified bipolar and related disorder is appropriate.
Treatment and management
-
Pharmacological treatment:
When it comes to treatment, there are no clear guidelines for the pharmacological treatment of Delusional disorder [8]. The most commonly used treatment is antipsychotics, mostly first-generation antipsychotics and second-generation antipsychotics [8]. Antipsychotics achieved a 33.6% good response in the treatment of DD [8]. second-generation antipsychotics appeared to be less effective than first-generation antipsychotics [8]. There is a high degree of heterogeneity in variables such as response rate, treatment, follow-up period length, and response criteria [8].
The response is greater in hospitalized patients [8]. second-generation antipsychotics are safer and more appropriate for DD as they have a wider coverage of affective and negative psychopathology [8]. The good response rate for SGAs was higher for inpatients rather than outpatients [8].
First-generation antipsychotics:[8]
- Pimozide was the most used drug, and it showed a similar response in all types of DD.
- Somatic DD responded better to pimozide than to other APS [8]
- Pimozide increases the risk of arrhythmia because it largely increases the QT interval on ECG. This is why it is no longer the first-choice treatment.
- Pimozide good response rate of 48.6%.
- Haloperidol good response rate of 32.3%.
Second-generation antipsychotics:
- Only a few case reports have documented the effectiveness of SGAs in DD [7].
- Risperidone good response of 34.3% [8].
- Olanzapine good response of 33.7% [8].
Aripiprazole:[7]
- This is a third-generation antipsychotic with partial D2 agonist properties, which differentiates it from SGAs.
- It showed a good response in only 33.6% of patients.
- It was used on patients who previously received treatment with FGAs and SGAs but either showed no response or were unable to tolerate the side effects.
- Improvement was reported in around 5-6 weeks with the dose used is 11.1 mg/day.
- It is mostly used as monotherapy but sometimes combined with antidepressants.
- A combination of aripiprazole with antidepressants was highly effective in the somatic DD.
- It’s effective in DD cases because it modulates dopamine and serotonin signaling.
Conclusion: Treatment of Decisional disorder with antipsychotics is effective in 94% of patients regardless of the used medication [2].
-
Cognitive behavioral therapy (CBT) [2]
- CBT is the only psychological therapy with evidence of effectiveness. It resulted in a greater reduction in effect relating to belief, the intensity of conviction, and positive action on belief subscales of the Maudsley Assessment of Delusions schedule.
- CBT did not abolish delusions.
- It is intensive and may not be cost-effective.
Risk factors [5]
- Low socioeconomic status.
- Older age.
- In women with premenopausal onset, erotomaniac themes predominated [4].
- Somatic and jealousy delusions were more common in postmenopausal-onset women [4].
- Family history of psychiatric disease especially:
- Schizophrenia > Almost 9% of patients had a positive family history of schizophrenia [11]
- Paranoid personality disorder [11]
- Premorbid tendency to jealousy [11]
- Sensory defect (deafness).
- Exposure to stressful life events.
- The delusional disorder usually develops under variable levels of psychological stress. Vulnerable patients will develop delusion-like responses to the stress so they can be the ones controlling it[9].
- Men:[12]
- A younger onset of disease.
- More schizoid premorbid personality features.
- More likely to have the diagnosis changed to schizophrenia or schizoaffective disorder.
- Women:[12]
- Poorer initial social functioning.
- Better engagement with therapeutic interventions helped to regain functioning.
- More likely to receive medication but less likely for the disorder to remit.
Prognosis
Third of the patients were found to reach remission [10]. It is usually better when the duration of the delusion is short before seeking help and when precipitating factors have been present during the development of DD [10]. Acute and subacute turn out to have favorable outcomes [10]. The diagnostic stability of DD is moderate (around 60%) in long-term follow-up studies. The diagnosis would later be changed to schizophrenia in 20% of cases [10]. Delusions usually tend to weaken with time, but a small group of patients will still have the intensity of delusions for years [10]. The course of the disease is highly variable, going from rapid and full recovery to a chronic condition [7]. Psychiatric comorbidity rates ranged from 46.5% to 64.8%, considered fairly high, with mood disorders being the most frequent [5].
Recent updates
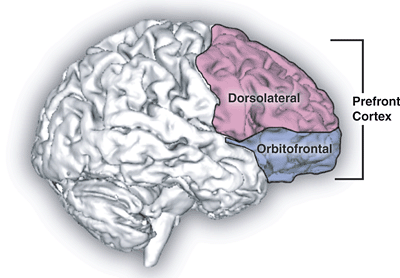
Researchers conducted a combined functional and structural imaging study in a sample of delusional disorder (DD) patients to determine if DD is associated with structural and functional imaging changes and to what extent. They performed structured imaging with both modulated and unmodulated analysis. They also performed cognitive task fMRI and resting-state functional connectivity analysis. Results were compared between DD patients, schizophrenics, and controls. Structured imaging revealed a significant reduction of cortical thickness. The unmodulated analysis revealed a decline in the bilateral insula/middle temporal gyrus and the cortical grey matter in the medial frontal/anterior cingulate cortex. In addition, it showed a decrease in scattered distributed small clusters. The modulated analysis did not show any significant difference between patients and controls. Cognitive task fMRI revealed a significant cluster of failure of deactivation in the anterior/medial frontal cingulate cortex. Resting-state functional connectivity (fcMRI) demonstrated that DD patients exhibited a significant decline in resting-state connectivity in the bilateral insula. Structured imaging and cognitive task fMRI results in DD patients are a bit similar to Schizophrenia, or at least they’re both present but to a different extent. The reduction in resting-state connectivity has fewer clear parallels with schizophrenia while the failure of deactivation is now considered a well-replicated finding in schizophrenia
Recommendations
This paper highlighted the most important information about delusional disorder. However, future researchers could further investigate the genetic basis of DD and the brain’s structural and functional changes as this would help understand the disease more. We should raise awareness campaigns to educate the community about DD and encourage seeking professional help.