Article topic: Charles Bonnet syndrome
Author: Sarkis Gerges
Editor: Lubna AL-Rawabdeh
Reviewer: Ethar Hazaimeh
Keywords: Charles Bonnet syndrome, visual hallucinations, visual impairment
Introduction
Charles Bonnet Syndrome (CBS), also called “ phantom vision,” is an illness where cognitively normal people experience simple or complex and consistent visual hallucinations, due to damage along the visual pathway.[1]This condition was named after the 18th-century botanist and philosopher, Charles Bonnet recounted the complex visual hallucinations experienced by his grandfather, Charles Lullin, in his work “Analytical Essay on the Faculties of the Soul.”[2]
Depending on the study, the prevalence of CBS might range from 0.4% to 30%[1]. Differential CBS prevalence rates exist for a variety of reasons. First, no single definition of CBS has been endorsed by all medical professionals. Second, ophthalmology, geriatric medicine, and neurology are among the fields in which CBS is diagnosed. Third, many people are hesitant to admit that they have visual hallucinations out of concern that they will be branded as mentally ill [3,4,5].
Etiology and pathogenesis:
Many studies show no positive correlation between the risk of CBS and increased age [6,7]. Even though CBS affects geriatric populations because of the increased incidence of eye disease in the elderly, it can affect all ages suffering from visual impairment [8].
CBS can be caused by any factor affecting the visual pathway, extending from the visual cortex down to the eyes [9]. The most common etiologies include Figure (1):
- Age-related macular degeneration
- Diabetic retinopathy
- Cataract
- High Myopia
- Retinal vein occlusion
In addition to these etiologies, subjective feelings of loneliness, low extroversion, and shyness may contribute to an increased risk of being affected by CBS. [10]
The precise pathogenesis of CBS is still unknown. However, 2 main theories are suggested to explain the visual hallucinations experienced during CBS:
- The deprivation theory suggests that diminution in sensory input leads to the production of spontaneous images from the visual association cortex, resulting in visual hallucinations [12].
- The ‘release theory’ suggests that a lesion of the visual pathway causes abnormal signals to be sent to the visual cortex. The hallucinations result from a combination of normal and abnormal signals at the level of the visual association cortex [12].
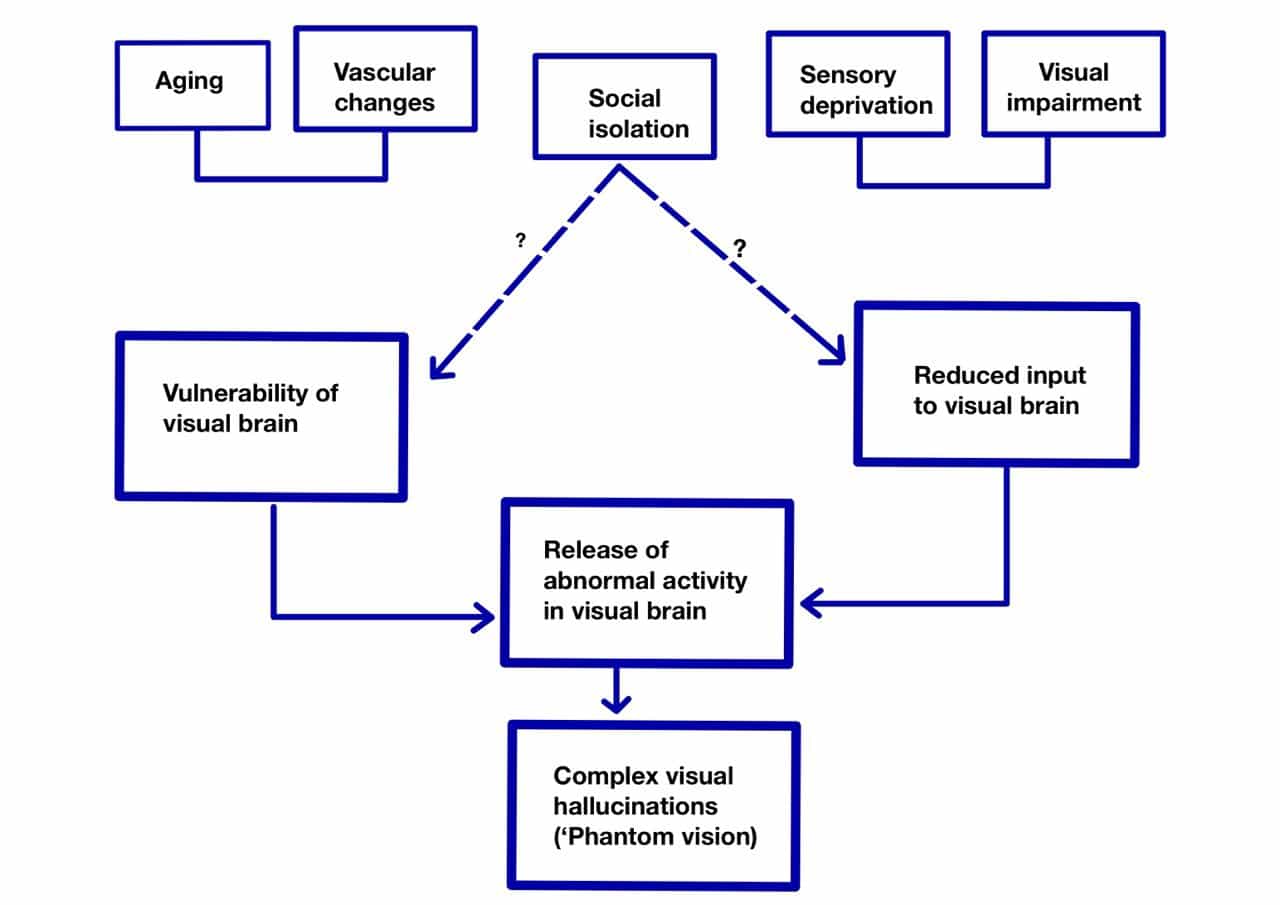
Figure (1): Factors contributing to CBS pathogenesis Charles Bonnet syndrome
Clinical presentation:
Clinical case:
A 91-year-old patient suffers from age-related macular degeneration and chronic diseases such as hypertension and has geographic atrophy in both eyes. This patient was diagnosed with CBS after seeing many complex images several times over 2 weeks. In addition, The hallucinations lasted for only a minute, and were not scary to the patient, as he was able to know they were not there.[11] The following 2 figures ( Figures 2 and 3 ) show the patient’s posterior pole of both eyes where we can notice a large geographic atrophy.[11]

Figure 2: Posterior Pole O.D.

Figure 3: Posterior Pole O.S.
Clinical Characteristics
The frequency and timing of the hallucinations can vary widely among patients with Charles Bonnet Syndrome. Hallucinations can be episodic, periodic, or chronic. The hallucinations are usually daily (like in the presented case), but they may be weekly and tend to occur upon awakening [6,14].
Furthermore, patients who have recently begun hallucinations hallucinate more frequently than those who suffer from chronic hallucinations. In addition, the hallucinations tend to last for several minutes ( 70%), but in some cases, the duration of hallucinations can be seconds or hours [14].
Unfamiliar or familiar images may be seen during hallucinations. Hallucinations may occur in color or in black and white, they could be motionless or not. In addition, hallucinations could be less clear in comparison to reality. Usually, patients hallucinate only with their eyes open [9]. Finally, patients suffering from CBS are mentally and cognitively normal.
Complications:
CBS is described as a temporary condition not associated with significant adverse complications outside of aggravating illusions. However, approximately 32% of CBS patients suffer from psychological problems such as anxiety and emotional distress due to hallucinations, thus, a continuous psychological follow-up is required.[15,16]
Workup and Diagnosis:
In addition to CBS, visual hallucinations can be caused by different neurological, psychiatric, and metabolic disorders (Table 1). Hence, these etiologies must be ruled out to diagnose CBS by performing psychological and neurological tests such as MMSE and CT scans. CBS is considered a diagnosis of exclusion, but the diagnosis can be more difficult because of the comorbidities, especially in the elderly.[17,18]
| Neurologic disorders | Hemispheric lesions
Parkinson’s disease Lewy-body dementia Brain-stem lesions Epilepsy Migraine Narcolepsy-cataplexy syndrome |
| Psychiatric disorders | Acute psychosis
Delirium Schizophrenia Affective disorder Conversion reactions |
| Toxic and metabolic disorders | Metabolic encephalopathies are caused by cardiopulmonary insufficiency, uremia, hepatic disease, endocrine disturbances, and vitamin deficiency states.
inflammatory and infectious diseases Hallucinogenic agents Drug and alcohol withdrawal syndromes Medications or toxin side effects |
| Miscellaneous conditions | Sensory and sleep deprivation
Hypnopompic or hypnagogic states Intense emotional experiences (stress, grief) Charles Bonnet syndrome |
Table (1): Causes of visual hallucinations [17]
Treatment and management:
Management of CBS can vary depending on the severity of symptoms. In mild symptoms, reassurance is sufficient in 94% of the cases. However, in more severe symptoms, CBS can be managed by medications and behavioral techniques, such as blinking during a hallucination, rapid eye movement from one object to another, or improved lightning. [12,19]. In addition to these techniques, many other types of treatments could be given:
Pharmacotherapy:
Used to treat patients who suffer from continuous and disturbing hallucinations. In such cases, physicians may prescribe low doses of atypical antipsychotics such as olanzapine and quetiapine or cholinesterase inhibitors such as donepezil, since these drugs show good efficacy and minimal side effects. [19,20,21].
Psychological therapy:
Psychological therapy techniques such as hypnosis, relaxation, and cognitive remodeling have been advocated to minimize visual hallucinations’ disturbing effects.[22]
Optimizing Visual Function:
Hallucinations may disappear through optical correction, although visual deficit correction may not always be possible[1]. Removal of a cataract, treatment of diabetic retinopathy, and laser photocoagulation of a subretinal hemorrhage (all with resultant improvement in vision) have been associated with the alleviation of illusions.[17]
Prevention:
There is no concrete way to prevent CBS, but preserving the vision can reduce the risks. Therefore, people, especially the elderly, must have regular eye exams. [24]
Prognosis:
Recent studies suggest that CBS takes more than 8 years to be resolved, in other words, hallucinations’ frequency tends to decrease after a long period. However, an old study indicates that Charles Bonnet syndrome tends to resolve spontaneously within a year, as was the case for Charles Lullin.[25,26,27]





