Article Topic: Trigeminal Neuralgia
Author: Hashem Mohammad Jameel Bani Ata
Editor: Ethar hazaimeh, Yaman B. Ahmed
Keywords: Headache, Migraine, Cranial nerves, Pain.
Introduction1,2
The International Classification of Headache Disorders ICHD-3 defines neuralgia as “pain in the distribution(s) of a nerve or nerves, presumed to be due to dysfunction or injury of those neural structures. Common usage has implied a paroxysmal or lancinating quality, but the term neuralgia should not be reserved for paroxysmal pains.”
The most common neuralgias are trigeminal neuralgia, occipital neuralgia, glossopharyngeal neuralgia, and Nervus intermedius neuralgia.
The International Classification of Headache Disorders defines trigeminal neuralgia (TN) as “A disorder characterized by recurrent unilateral brief electric shock-like pain, abrupt in onset and termination, limited to the distribution of one or more divisions of the trigeminal nerve and triggered by innocuous stimuli.” trigeminal neuralgia is the most common form of craniofacial pain.
Epidemiology5
TN is a rare condition, however, it is the most common neuralgia with an incidence of 5/100,000 annually, and is usually seen in the middle or elderly ages with female to male ratio equal (3:1). (2 – 5)% of patients with multiple sclerosis suffer from trigeminal neuralgia. The incidence increases with age: it is rare below the age of 40 so in 90% of the cases, symptoms appear after age 40. Familial cases of TN are reported in (1-2%) of all cases. Racial or geographic differences in trigeminal neuralgia are not reported.
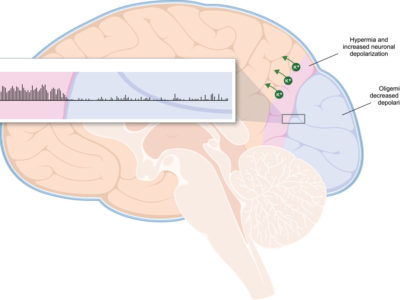
Pathogenesis5,12
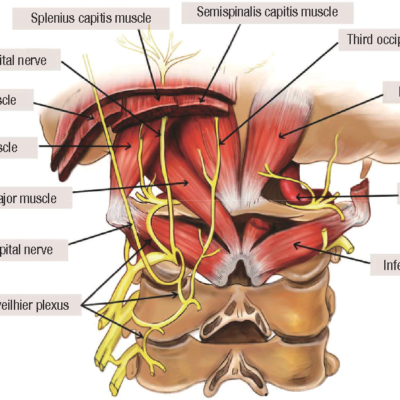
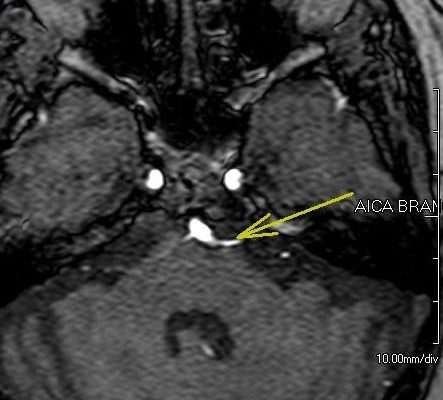
It is proposed that the trigeminal nerve roots into the pons are compressed by an aberrant loop of the vessel (usually by a superior cerebellar artery), so demyelination of nerve fibers occurs, which makes nerve fibers hyperexcitable. This hypothesis is supported by that microvascular decompression relieves pain in most cases.
compression causes could be by :
- Brain tumors: meningiomas and vestibular schwannomas
- Aneurysms
- Arteriovenous malformations
- Cysts
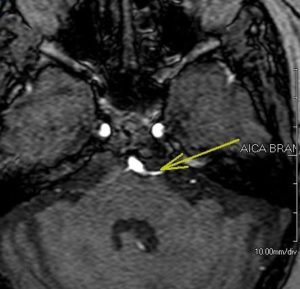
Figure 1: Enlarged vascular loop of anterior inferior cerebellar artery pressing upon trigeminal nerve 13
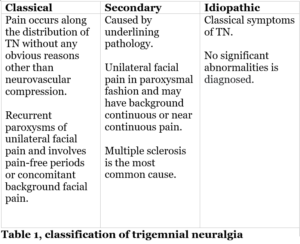
Etiology1,3,4
The pathology of these cranial neuralgias can be due to almost any type of lesion: compressive, metabolic, or infectious. According to ICHD-3, It is classified to classical, secondary, and idiopathic. Table 1.
Clinical features5,6
TN is characterized by short paroxysms of high-intensity sharp, stabbing facial pain in the distribution of the fifth cranial nerve, lasting from second to two minutes, each attack is followed by a refractory period during it no other attack is provoked.
The most trigeminal branch affected is maxillary and the least one is ophthalmic. Low probability of three branches being affected.
Triggers are described as minimal, seemingly harmless touches to the critical areas. Among the commonly described triggers are chewing, talking, touching, cold or hot sensations, shaving, or wind, usually over the division of cranial nerve V affected. These triggers reflect negatively on the quality of life because patients avoid feeding and communication due to fear to stimulate the pain.
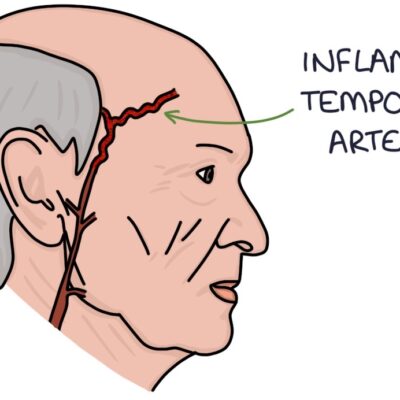
Autonomic symptoms; such as conjunctival injection or tearing, miosis, ptosis, sweating, and clogged nose may also occur with pain unilaterally in the affected side. Episodes of pain interval may last for weeks or months followed by intervals with no pain.
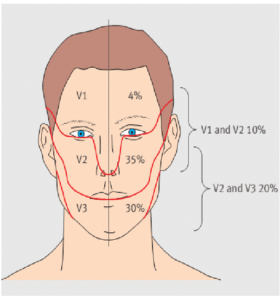
Figure 2:distribution of trigeminal neurolagia 7
Painful trigeminal neuropathies1,8,9
The painful trigeminal neuropathies listed by the ICHD-3 include:
- Acute herpes zoster:
Diagnosis is got by the history of chickenpox and dermatologic lesion of a division of trigeminal nerve, and it is most common in V1, unlike classical trigeminal neuralgia. It is more common in females. Immunosuppression is a risk factor for acute herpetic infection.
- Postherpetic trigeminal neuropathy:
is caused by the reactivation of varicella-zoster virus in the dorsal root ganglia neural cells. It causes unilateral stabbing radiating pain, confined to a dermatome. Risk factors associated with a higher risk to develop PHN are old age and Immunosuppression. It resolves spontaneously over weeks or months after the rash resolutes in most cases.
- Painful posttraumatic trigeminal neuropathy:
is a complication of oral and maxillofacial procedures such as implant surgery and the removal of impacted lower third molars. It is characterized by sensation disturbance and neuropathic pain.
- Trigeminal neuralgia secondary to Multiple sclerosis10
Multiple sclerosis: is a chronic, demyelinating disease of axons in the central nervous system, it increases the risk of developing trigeminal neuralgia by 20-fold, which is characterized by a sudden, more frequently bilateral, brief, stabbing recurrent pain with a distribution of one or more branches of the fifth cranial nerve. Attacks last from parts of a second to two minutes with frequency possibility through(1-50) days. trigeminal neuralgia secondary to multiple sclerosis is more common in females than in males and characterized earlier age of onset with a range (40-50) years.
Diagnosis of trigeminal neuralgia secondary to multiple sclerosis: is done by:
- Trigeminal reflex(blink reflex and the masseter inhibitory reflex): structural lesion caused by multiple sclerosis results in abnormal reflex,89% of patients with trigeminal neuralgia due to multiple sclerosis have the abnormal reflex. This technique provides specificity and sensitivity reach to 90%.
- MRI: it is useful in identifying any linear plaques in the ventrolateral pons located between the trigeminal root entry zone and the trigeminal nuclei, and to identify compression of the trigeminal nerve root by vessels.

Figure 3: trigeminal neuralgia secondary to MS11
Risk factors14
The risk of trigeminal neuralgia increases with age, so most cases are above the age of 40 with women predominance. Multiple sclerosis and hypertension are the most common risk factors for trigeminal neuralgia. Diabetes and chronic sinusitis are reported in rare cases.
Diagnosis4,15,16
Trigeminal neuralgia is diagnosed clinically depending on the Diagnostic criteria for classic TN from The International Classification of Headache Disorders :
- Pain has all of the following characteristics:
- lasting from a fraction of a second to 2 minutes
- severe intensity
- electric shock-like, shooting, stabbing, or sharp in quality
- Precipitated by innocuous stimuli within the affected trigeminal distribution
- Not better accounted for by another ICHD-3 diagnosis.
Neuroimaging with MRI and CT is considered when suspecting with trigeminal neuralgia, but without symptoms of trigeminal neuralgia, also to identify vascular compression.
Electrophysiologic trigeminal reflex assessment is normal in classic TN, so it is useful to differentiate classic TN from painful trigeminal neuropathy.
Differential diagnosis6
- Glossopharyngeal neuralgia
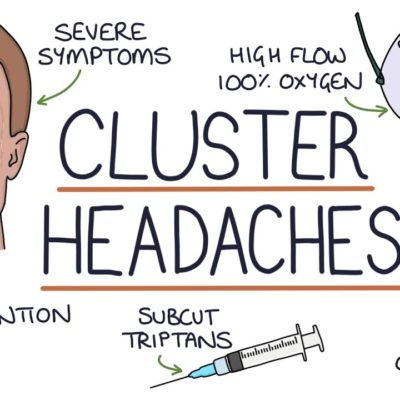
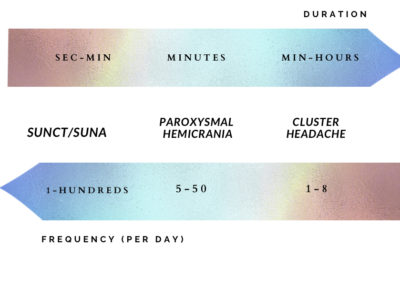
- Cluster headache
- Chronic paroxysmal hemicrania
- Tolosa-Hunt syndrome
- HZ involving the trigeminal ganglion
- Short-lasting unilateral neuralgiform headache with autonomic symptoms (SUNA).
Treatment2,12,17–19
Pharmacological therapy
- Carbamazepine: is the drug of choice in the treatment of trigeminal neuralgia. at the beginning of treatment, the dose is 100 – 200 mg twice /day with an increase of 100 mg every other day until the pain is relieved. The maximum dose is 1200 mg/d. However long term treatment with Carbamazepine is associated with bad side effects as the following:
- Hyponatremia: in many cases is mild hyponatremia that results in drowsiness, diplopia, vertigo, and Some cases have severe hyponatremia which results in coma.
- Development of resistance and intolerance.
- Hemopoietic depression.
- Aplastic anemia.
- Abnormalities in liver functions.
- Oxcarbazepine: is often used as an initial drug for trigeminal neuralgia, its side effects are the same as Carbamazepine with the exception of hyponatremia, with lower frequency than with carbamazepine. The dose is 150 mg twice/day, The dose can be increased as tolerated in 300 mg increments every third day until pain relief occurs. The maximum dose is 1800 mg/d.
- Anticonvulsant drugs: gabapentin, lamotrigine, and baclofen may improve the case:
- Gabapentin: 300 mg/d with increase 300mg/ 2-3 days. maximum dose is 1800 mg/d.
- Lamotrigine: dose 25 mg twice/day, with a gradual increase to 200-400 mg/d. Lamotrigine is associated with some side effects like sleepiness, dizziness, headache, vertigo, ataxia, and skin rash in the first 1-2 months of treatment, most often resolves during the therapy and it occurs in 7–10% of patients, Stevens-Johnson syndrome: once it occurs the medication should be stopped. It develops in 1 from 10,000 patients.
- baclofen: dose is 10 mg/d for 3 days with the possibility to increase the dose to 10-20 /d every 3 days if there is a need.
- Phenytoin: less effective, but is used in cases of refractory pain and carbamazepine intolerance.
- Peripheral alcohol injections: it may relieve the pain however, it has 3 negative points which are :
- tissue inflammation and fibrosis.
- temporary weakness the muscles of mastication
- burning alcohol neuritis
Surgery
Surgical intervention is considered to patients of trigeminal neuralgia refractory to pharmacological treatments, these surgeries are :
- Microvascular decompression: release the pressure on the trigeminal nerve by vessels. this procedure requires craniotomy to get the posterior fossa. However, this surgery has some complications at different rates as the following :
- Aseptic meningitis(11%): is the most common complication.
- hearing loss(10%): ipsilateral, major long term complication
- Diplopia: damage of the 4th or 6th nerve, often transient.
- Sensory loss(7%)
- 7th nerve palsy: rare
- Cerebrospinal fluid leak
- Infarction
- hematomas
- Percutaneous procedures on the Gasserian ganglion(percutaneous rhizotomies) :
This procedure is done by inserting cannula through foramen ovale to reach the lesion of the trigeminal ganglion or root, and treat this lesion by :
- Thermal: radiofrequency thermocoagulation.
- Chemical : injection of glycerol.
- Mechanical : compression by an inflation balloon in Meckel’s cave.
This technique is recommended for patients with multiple sclerosis complications are :
- Sensory loss happens in half of the patients.
- Postoperatively sensation of burning, heavy or aching(12%)
- Dysesthesias(6%)
- Anesthesia dolorosa (4%)
- Corneal numbness(4%) : there is risk to develop keratitis
- Meningitis: a major complication
- temporary chronic masticatory problems: half of the patients with balloon compression suffer from it.
- Gamma knife surgery: a non‐invasive procedure which is done by focus beam of radiation to the trigeminal root in the posterior fossa. Complications are facial numbness, sensory loss, or paresthesia in some patients.
- Peripheral neurectomy: is done by block or damage of trigeminal nerve outside the cranium.
- Recurrence of pain after surgery reaches up to 50% of patients after 5 years. Microvascular decompression has the longest duration of pain freedom in comparison with other interventions.