Article Topic: The use of stem cell therapy in the treatment of neurological disorders.
Author: Loay B. Zamil
Editors: Peter Bael, Hamid Ghanem
Reviewer: Ethar Hazaimeh
Keywords: stem cell therapy, neurological disorders, neurodegenerative diseases, nervous system, regenerative medicine.
Introduction
Nervous tissues have a special feature that other tissues do not have; the inability to regenerate their cells. You develop a nervous system and it remains with you throughout your life, except for some specific areas within the brain that are characterized by neurogenesis during adulthood which are the subgranular zone of the hippocampus (SGZ), and subventricular zone of the lateral ventricle (SVZ)[1].
There is a limited ultimate cure window for neurodegenerative diseases such as Alzheimer’s disease (AD), Cerebral palsy (CP), Multiple sclerosis (MS), and Parkinson’s disease (PD), which occurs due to progressive loss of structure, function, or number of neurons[2]. Besides that, the limitation for the vast majority of drugs regarding crossing the blood-brain barrier (BBB) makes the process of treatment more difficult[3].
Stem cell therapy looks like a golden solution for such disorders. It is a branch of regenerative medicine that focuses on the use of stem cells [4], which can achieve self-renewal and differentiate, to regenerate damaged cells of other types of tissue cells to replace damaged tissues that couldn’t regenerate again for any reason[2]. This gives us novel and effective treatments for neurodegenerative diseases with wider therapeutic windows than the currently limited treatment, and clinicians are solving the problem, not just supportive care and rehabilitation.
The problem that we struggle with
– Alzheimer’s disease (AD) is the most common type of dementia accounting for 60–70% of cases. Currently, more than 55 million people have dementia worldwide which is expected to rise to 139 million in 2050, and approximately 10 million new cases every year [5]. It is a multi-factorial disorder; the main reasons are age, environmental factors, such as chronic stress, traumatic brain injury, and several genetic factors.
Clinically, these patients are characterized by an impairment of short-term memory, later they are followed by impairment in other cognitive functions, such as logical understanding, language, and executive function. These characteristics are associated with a significant reduction in brain volume [6]. This reduction results from the degeneration of neurons and synapses, particularly in the hippocampus [1], which is a region of the brain responsible for memory and spatial orientation. The hippocampus is one of the first regions of the brain to suffer from damage.
Current pharmacological interventions in dementia are symptomatic relief drugs, which aim to treat some of the symptoms of dementia itself or other reflected symptoms. Currently, there are two drugs available for these patients, cholinesterase inhibitors, which function to prevent the acetylcholinesterase from breaking down acetylcholine, which helps in contact between nerve cells. The other drug is the N-methyl-D-aspartate (NMDA) receptor, which tries to block the effects of glutamate, which is excessively released in the brains of Alzheimer’s patients, and causes damage to their brain cells[7][8].
– Multiple sclerosis (MS) is a central nervous system disorder characterized by damage to the myelin sheaths surrounding the axons of neurons, caused by an autoimmune or persistent infection. Damaged myelin sheaths disrupt the conduction of action potentials along these axons, which is thought to cause many of the symptoms, and can also lead to the deterioration of axons, which can be detected as plaques or lesions visible with neuroimaging [9][24].
– Cerebral palsy (CP) is considered a neurodevelopmental disease, caused by multifactor that cause failure of the development of some brain areas during fetal life or post-neonatal onset, such factors are infection, hypoxia, and genetic mutation[10].
– Parkinson’s disease (PD) is a neurodegenerative brain disorder characterized by unintended or uncontrollable movements, that are caused by low levels of dopamine in the basal ganglia, a group of structures involved with the movement. These low dopamine levels in the basal ganglia are caused by the death of dopamine neurons in a region of the basal ganglia called the substantia nigra [11].
Such disorders and others have in common a characteristic of neurodegenerative disorder, which here in the nervous system causes a struggling issue that is distinct from other systems because the nervous tissues cannot regenerate their cells.
The Golden Solution for this problem
“This problem” is the lack of the ability to regenerate cells in the nervous tissue, and to solve it we have to replace or regenerate neuron cells. Stem cell therapy, which has been developed relatively recently, gives hope for doing that, an important branch of regenerative medicine, that focuses on the use of stem cells which can self-renewal and differentiate, to regenerate damaged cells of other types of tissue cells to replace damaged tissues that couldn’t regenerate again for any reason[2,3]. Stem cells as a treatment option have been increasingly popular due to their capacity to target specific pathways and improve patient outcomes [23].
Stem cell therapy enhances the level of functional recovery in the nervous system after the degeneration of its tissue and cells, by implementing exogenous stem cells, the degenerated neuronal circuitry could be regenerated [11]. Stem cell therapy offers amazing possibilities. The treatment aims to repair, replace, or at least prevent future deterioration, whereas, at present, we mainly provide supportive care to prevent such situations from becoming worse.
The Therapeutic Strategies:
Stem cell transplantation is mainly done by two methods. One is the transplantation of proper stem cells directly into the desired location, beside of internal environment and specific signal molecules they will be guided towards differentiation into a particular mature cell, thus exerting the necessary functions. The other method is done in vitro, by isolating, purifying, and amplifying a certain type of stem cell, and inducing it to differentiate into the cells with desired functions. Then, these mature, differentiated cells can be implanted into the damaged area. An appropriate combination of both methods may produce better effects for patients [12][21].
From where can I get it?
Stem cells can be classified into three types according to their abilities to differentiate and the range of the types of cells that can be generated. The first type is totipotent stem cells, which can give rise to all the cell types in a body, plus the placental cells. The second type is pluripotent stem cells, which can give rise to the three embryonic layers (endoderm, mesoderm, and ectoderm). Such as embryonic stem cells (ESC) and induced pluripotent stem cells (iPSC). The third type is multipotent stem cells, which are adult stem cells and can only generate specific lineages of cells. Such as; neural stem cells (NSCs) which are derived from neural tissues and can give rise to all cell types (neurons, astrocytes, and oligodendrocytes) of the nervous system [13][22].
Endogenous Regeneration
Mainly for AD, because this process depends on the principle of powering the neurogenesis ability of hippocampus tissue that has been weakened with age or other reasons [5][21].
The treatment aimed to return the ability of neurogenesis of such these areas and power it furthermore to recompensate that weakens. Which can be stimulated through extrinsic administration of chemical agents and growth factors, such as Erythropoietin, fluoxetine, granulocyte colony-stimulating factor, nerve growth factor (NGF), insulin growth factor-1 (IGF-1), and brain-derived neurotrophic factor (BDNF) [14].
Engrafted Regeneration
In contrast, this is concerned with implanting stem cells from outside the concerned tissue. Several major groups of stem cells are used for therapeutic purposes. Mostly, embryonic stem cells (ESCs), neural stem cells (NSCs), induced pluripotent stem cells (iPSCs), and mesenchymal stem cells (MSCs) are applied in this context. Other types, such as olfactory ensheathing cells and hematopoietic stem cells, may as well be applied [14][20].
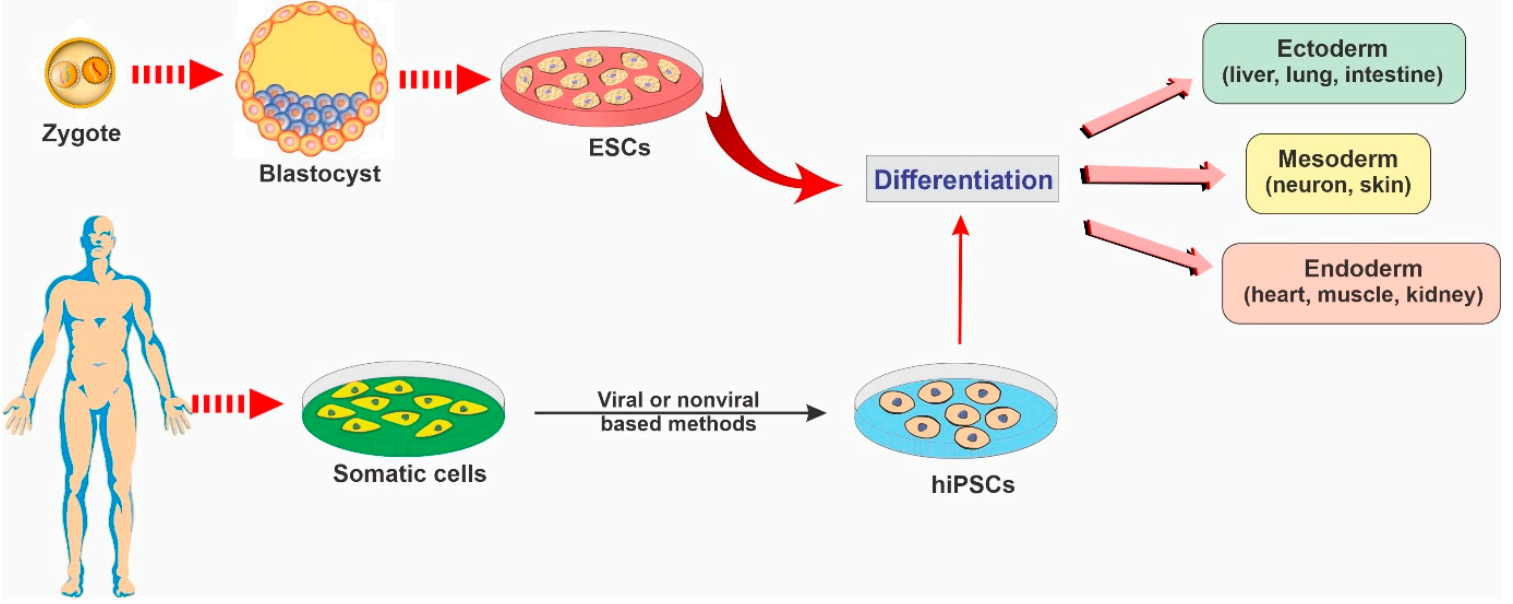
Figure (1): Representative diagram depicting the main types of stem cells and their potential to differentiate into various lineages.
Embryonic stem cells (ESCs)
They are pluripotency stem cells, very attractive candidates for therapeutic use. They are derived from the inner cell mass of a developing blastocyst at embryonic days 5-6. Pluripotency, is one of the biggest advantages, however, it represents one of their main drawbacks, as their differentiation can occur in any direction, and lead to neoplasia or teratoms[15].
Neural stem cells (NSCs)
Like “Engrafted Regeneration” in some way, it is a type of stem cell that is derived from the areas of the brain that have the feature of neurogenesis, such as the sub-granular zone (SGZ) of hippocampal and the subventricular zone (SVZ) of the lateral walls of the ventricles[1]. They are multipotent stem cells that can give rise to neurons, oligodendrocytes, or astrocytes[14].
Induced pluripotent stem cells (iPSCs)
Pluripotent stem cells are produced by reprograming derived patients’ cells by defined reprogramming factors back into an embryonic-like pluripotent state. Currently, there is a limited number of studies about iPSCs, due to their novelty and ethical issues.
Mesenchymal stem cells (MSCs)
They are multipotent stromal stem cells, found normally in the body’s tissue that can be isolated, such as bone marrow, umbilical cord, adipose tissue, peripheral blood, amniotic fluid, muscle, and lung. Bone marrow mesenchymal stem cells can differentiate into mesodermal tissues, which differentia from ectodermal and endodermal fates to end with the ability for use with neurological disorders.
The Routes of Stem Cell Administration
To deliver stem cells to the desired location of nervous tissue there is a variety of routes that are applied in research, comprising:
- Intraventricular, intra-subarachnoid space, and intrathecal transplantation provide effective access to pass through the BBB, allowing the stem cell to migrate and implant in the injured brain tissue area via the cerebrospinal fluid (CSF).
- Intracerebrally transplantation, delivery of clusters of stem cells, impeding their further migration towards sites of the damaged tissue, which compromises the effects and limits the application.
- Intravenous transplantation of cells overcomes the above disadvantages and can afford the transfer of a large number of SCs.
- The intraarterial route is the vascular delivery of stem cells, which can be directed to the injury site, and is more effective than the intravenous route. However, occlusion and thrombosis are the biggest problems.
- Another route is intranasal administration, which will not cause secondary injury.
It is self-evident that insufficient transplanted cells do not exert therapeutic effects, whereas an excess of cells may cause multiple complications including occlusion, thrombosis, and even the increased risk of tumor formation [18][25].
The Safety of Stem Cell Therapy
Administration of stem cells may cause severe adverse reactions and complications, such as:
- Thrombosis or embolism causes occlusion of the blood vessels which can result from excessive administration of stem cells [16].
- Immune rejection is caused by transplanted stem cells [17].
- Tumorigenicity and instability [12].
- In addition, can cause also other side effects such as seizure, infection, hyperpyrexia, and even death [12].
According to the Food and Drug Administration (FDA), other safety concerns
-
- Administration site reactions.
- The ability of cells to move from placement sites and change into inappropriate cell types or multiply.
- Failure of cells to work as expected.
- The growth of tumors [19].
References
References...