Article topic: Neurological Manifestations of COVID-19
Author: Miramar Haddad
Editors: Nicola Al-Madani, Ethar Hazaimeh
Keywords: Pandemic, covid-19, headache, CNS, nervous system, SARS-2.
Overview and epidemiology
Coronavirus is a single-stranded RNA genome with a positive sense and an envelope to protect its RNA. Corona in Latin means a crown that describes spikes like protein projection 1. The severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) is the cause of the coronavirus disease 2019 (COVID‐ 19), which is now a pandemic that has taken over the world since it started in December 2019 5 that affected individuals in every country and of any age 11. The median incubation period is usually 4 to 7 days, and symptoms will initially resemble influenza. Fever is present in 90% of cases 1.
As the number of patients grows as we go throw the pandemic the urgency to find a treatment for the patients, especially those who need assistance ventilation and people with the neurological manifestation of COVID- 19 7. The clinical manifestation of COVID- 19 could happen as an asymptomatic infection or severe acute respiratory distress with multiorgan involvement and death. COVID- 19 can also cause extrapulmonary complications such as neurologic disorders, which are increasingly reported day by day. Understanding the nervous system involvement pathways and neurologic manifestations can be useful in improving the assessment and management of SARS-CoV-2 patients. These disorders can interfere with the prognosis or require treatment modification.
Pathogenesis and etiology
COVID- 19 binds to ACE2 (the angiotensin-converting enzyme 2) by the spikes that allow COVID-19 to enter and affect the cell. for the virus to have a complete entry the spikes have to be primed by an enzyme called protease (TMPRSS2) 12. the virus enters the host cell and un coat. Then the genome is transcribed and then translated. The genome replication and transcription takes a place at the cytoplasmic membrane 12. COVID-19 is related to a severe innate immune response and continued raise of systemic cytokine levels. the innate immune response that started due to covid-19 infection is suggested to be an indication to predict mortality and severity7.
Cardiovascular, cerebrovascular disease and several abnormalities also have been observed including cellular immune deficiency, coagulation activation myocardia injury, hepatic and kidney injury, and secondary bacterial infection rise the possibility of severe disease. It has been recorded that in these cases (severe disease and death ) lymphopenia and sustained inflammation 12.
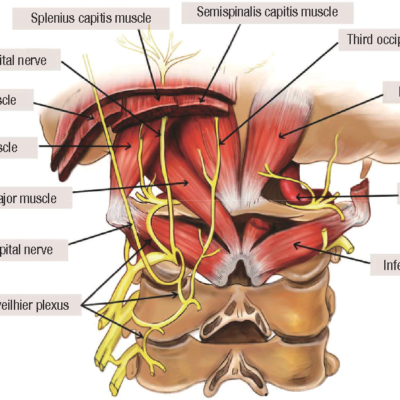
The majority of viral infection begins in the peripheral tissues. despite our body protective barrier and the immune system. viruses might invade the nervous system including covid-19 which either affect the CNS hematological ( by the bloodstream ) or by infecting the nerves connecting to peripheral tissue 11. A lot has been investigated on the pathogenetic mechanisms involved in the acute phase of neuro-COVID in the past months and these studies hinted that SARS-CoV-2 is a neurotropic virus 6.
Clinical presentation and complications
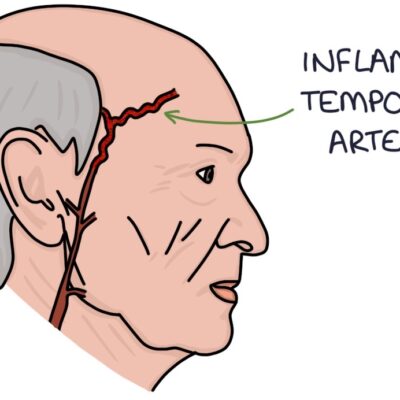
COVID-19 can cause complications in the entire neuraxis 1, some of these complications might be a para-infection syndrome or postinfection syndrome, or both 1. Fig (1) shows the mechanism of nervous system infections and neurological repercussions caused by SARS-CoV-29.
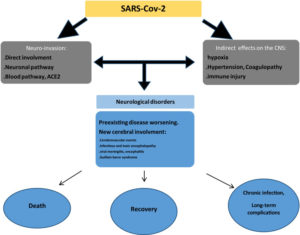
figure 1 : The mechanism of nervous system infections.
Neurological symptoms and manifestations can affect three possible systems: the central nervous system CNS, the peripheral nervous system PNS, and the musculoskeletal system 10. Around 26% of the acute phase of COVID- 19 infection develop neurological symptoms and about 25% of them can be attributed to the direct involvement of the central nervous system 7.
Headache, confusion, and dizziness are the most common general but not specific neurological symptoms observed in COVID- 19 patients. Ansomnia and ageusia are common manifestations also 1. Some long-term complication that stays after the resolving of the infection includes dysautonomia, exercise intolerance, malaise, sleep disturbances, cognitive impairment, and mood disorders 1. Encephalopathy is the most common neurological manifestation in covid-19 hospitalized patients 1.
40% to 60% develop loss of smell and 90% alteration of smell 1. the alteration of the sense of smell and/or taste in uncomplicated early-stage COVID-19 patients is suggestive of a movement of the virus to the brain via the olfactory bulb which allows the virus to reach and affect the brain 9. The acute ischemic stroke incidence among COVID-19 patients is estimated at 2.3% with a pooled prevalence for an acute cerebrovascular disease of 2.6%. the prevalence of acute cerebrovascular diseases in COVID-19 hospitalized patients with more severe infection almost reaches 6% 3,10.
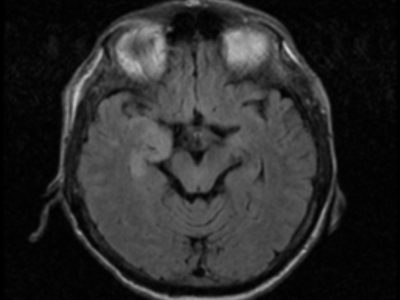
These patients often have a prothrombotic problem and can develop occlusion of multiple arteries and the venous system simultaneously 1. It has been recently reported several categories of cerebrovascular events (intracerebral hemorrhage, ischemic stroke, and cerebral venous thrombosis ) in COVID- 19 patients 9. All of this can generate severe and sometimes fatal outcomes for those who are affected 3.
Work up and diagnosis
Early detection of the possible neurological symptoms, manifestations, and complications is necessary to limit the long-term consequences of COVID- 19. The health care professional should be aware of the heterogeneous neurological manifestations of COVID- 19 when dealing with the patients during the current viral pandemic 10. The patient who severely suffers from covid-19 and other clinical signs of seizures or encephalopathy could benefit from electroencephalography monitoring (EEG) to early diagnose and treat seizures 10.
We primarily diagnose the patient who dealing with cerebral venous sinus thrombosis based on clinical and radiological criteria with (MRI) and venography and computed tomographic venography being the non-invasive imaging modalities of choice 10.
Following a multidisciplinary approach for the treatment of neuro-PASC (post-acute sequelae of SARS-CoV-2) will be the best way to diagnose and address these symptoms. Tailored rehabilitation and novel cognitive therapy protocols are equally important as pharmacological treatments to treat neuro-PASC effectively 4.
Treatment and Management
Taking care of the patients who develop and suffer from COVID- 19 neurological manifestation will be the responsibility of the neurologist from early diagnosis and treatment to reach effective management to these patients 1. The Management of COVID-19 patients has to include early clinical, radiologic, and laboratory neurologic assessment, with a close follow-up, especially in severe forms 9.
The statistics that were collected during the pandemic highlight the careful and continuous follow-up of COVID- 19 patients, even if they are asymptomatic by regular screening for probable long-term persistent neurological sequelae. When several cases develop a neurological manifestation they require rapid lines of communication to be established between primary care physicians and neurologists in many ways either via direct emails or telephone communications through neurology registrars for at least once to properly document and study these cases that develop this kind of symptoms 3.
Patients who suffer from encephalopathy that can affect neurological function can benefit from exercises to stimulate neuroplasticity, these exercises might be music therapy, physical therapy, cognitive-behavioral therapy, gait training, telerehabilitation, among others. This is better achieved with the help of a multidisciplinary team that includes neurophysiology, biomechanics, biomedical engineering, physiotherapy, and clinical medicine 3.
For the patient who lost the sense of smell, most physicians have been administering empirical treatments for COVID-19-associated olfactory dysfunction, including topical or systemic steroid supplementation and olfactory training 2. Sometimes knowing the pathogenesis helps in determining treatment modalities like attempting to rapidly neutralize the host cell binding S-protein of SARS-CoV-2 by infusion of monoclonal antibodies 6.
A couple of studies showed that there are a few recombinant compounds as IFN with ribavirin had only limited effects against COVID-19 infection 12. Another study suggested the administration of immunomodulatory hormones, like melatonin, and curcumin to help the neurorehabilitation interventions, based on the demonstrated share pathobiology of the neurological impact in acute ischemic stroke and COVID-19, manifestations like fatigue, infection, dyspnea, muscle weakness, and neuropsychiatric manifestations as impaired thinking, depression and anxiety. However, better quality studies are needed to support this intervention 3.
the prognosis of recovery from post-COVID neurological syndrome must be evaluated in a personalized way, taking into consideration the target organ damage, especially lungs and heart, which intervene in the process of physical activity and maintenance of the patient daily living activities. It is necessary to design a specific protocol and to establish directed spaces for the neurorehabilitation process, that include personnel, infrastructure, and technological equipment that guarantee therapeutic success, especially in low and middle-income countries that do not have units of specialized rehabilitation 3.
Risk factors
The SARS-CoV-2 infection might affect the brain and influence it by different factors including genetic and environmental factors. Several patients who have COVID-19 infection also have chronic diseases, which might increase the probability of getting an infection and lower their immune-mediated response. Immune and neural cells serve as reservoirs of latent SARS‐CoV‐2, which may contribute to the delayed neurodegenerative events 11. The blood-brain barrier in a healthy individual prevents the breach by pathogens. however, if there is immunosuppression and inflammation, invasion of viruses could happen. (Mahalakshmi et al., 2021) 11
Prognosis
Only a minority of patients with the usual risk factors develop severe neurological symptoms such as acute cerebrovascular disease which is associated with poor outcomes 9. To provide a better prognosis early initiation of neurorehabilitation is crucial, it is not prudent to start until the patient’s health status stabilizes, to avoid possible relapses during rehabilitation. It is essential to carry out a complete evaluation in stroke patients that eventually will go to the rehabilitation area since it must be determined the short, medium, and long term prognosis 3.
Studies showed that patients who develop encephalopathy suggest that in general, these patients have a worse prognosis and a lower survival rate. This association could be mediated by ACE2 / SARS-Cov-2 interaction, which happens on capillary endothelium and neurons. Thus, neurotropism is directly affecting the entire brain territory 3.
References...