
Article Topic : Meningitis
Name of the Author : Hashem Mohammad Jameel Bani Ata
Keywords : meninges , meningismus , neuroinfectious disease
Overview
Meningitis is defined as inflammation of the meninges, diagnosed by an abnormal number of white blood cells in the cerebrospinal fluid and certain clinical signs and symptoms1 . The cause could be chemical or infectious , however the most common causing micro-organisms are enteroviruses . Aseptic meningitis has self-limiting course , but bacterial one has high morbidity and mortality rates , so immediate treatement and diagnosis should be done2. Patients with bacterial meningitis present with the abrupt onset of fever, headache and meningismus3 . Streptococcus pneumoniae and Neisseria meningitidis are the main bacterial caustive pathogens outside the neonatal age4 . classical clinical signs that are used to diagnose meningitis are nuchal rigidity, Kernig’s sign and Brudzinski’s sign5.
Epidemiology6 7
Globally, bacterial meningitis has a prevalance rate of more than one million cases and 135,000 deaths annually. Continuous neurological complications occur in 9-25% of cases. However, administration of conjugate vaccines for Haemophilus influenzae type b, N. meningitidis, and S. pneumoniae contributes in decreasing the incidence of bacterial meningitis .
Etiology8 9 10
The etiologies of meningitis ranges in severity of caused disease from benign and self-limited to life-threatening. Bacterial meningitis requires fast recognition and treatment. Aseptic meningitis is the most common form of meningitis especially viral and require supporutive treatment . enterovirus accounts for the most common cases of meningitis .
Viral meningitis :
- Enterovirus (most common cause)
- Herpes simplex virus
- Varicella zoster virus
- Arboviruses(e.g., West Nile virus)
Bacterial meningitis : depend on age, vaccination status, and recent trauma or instrumentation as illustrated in Table 1.
Table 1. Bacterial meningitis
| Age /condition | Propaply pathogen |
| Infants within the first month | Streptococcus agalactiae, Listeria monocytogenes, Escherichia coli |
| Children 1 to 23 months of age | Streptococcus pneumoniae, Neisseria meningitidis, S. agalactiae, Haemophilus influenzae, E. coli |
| Age (2 -50 ) year | N. meningitidis, S. pneumoniae |
| Age > 50 / immunocompromiesd / alcoholics | S. pneumoniae, N. meningitidis, L. monocytogenes, |
| basilar skull fracture / cochlear implant | S. pneumoniae, H. influenzae |
| penetrating trauma / post neurosurgery | Staphylococcus aureus, aerobic gram-negative bacilli ( Pseudomonas aeruginosa), Coagulase-negative staphylococci |
| cerebrospinal fluid shunt | Staphylococcus aureus, aerobic gram-negative bacilli(Pseudomonas.aeruginosa), Propionibacterium acnes, Coagulase-negative staphylococci |
Fungal menigitis
Fungal systemic infection can reach the subarachnoid space and cause meningitis, either haematogeneously or due to trauma or surgery . Major fungal pathogens are :
- Neoformans,C. gattii, C. immitis : cause infection in immunocompetent and immunocompromised individuals . Cryptococcal meningitis is the most common fungal meningitis , and HIV is the largest risk factor for it . Other risk factors are steroid therapy, chronic disease in kidney, liver, or lung disease, malignancy and solid-organ transplants.
Immunocompetent individuals with no chronic diseases commonly get infected by C. gattii causing Cryptococcal meningitis. - Histoplasma meningitis : causes infection in immunocompetent and immunocompromised individuals, particularly these patients are AIDS patients, solid-organ transplant recipients, receiving corticosteroids or TNF-α antagonists.
- Coccidioides meningitis : Although immunosuppression state increases risk of Coccidioides meningitis , gentics play a major role in it , because Filipinos and African Americans have the highest incidence .
- Candida meningitis : opportunistic fungi that can disseminate through the CNS in immunocompromised state or a disrupted protective structures . It is most common in infants with an immature BBB, patients with ventriculoperitoneal shunts or ventriculostomies.
Parasitic(Eosinophilic) meningitis : presence of >10 eosinophils/μL in cerebrospinal fluid (CSF) . the most common causes are Angiostrongylus cantonensis and Gnathostoma spinigerum.
Noninfectious meningitis :
- Drug-induced (e.g., non-steroidal anti-inflammatory drugs, trimethoprim/sulfamethoxazole)
- Neurosarcoidosis
- Neoplastic meningitis
- Leptomeningeal carcinomatosis
- Benign recurrent lymphocytic meningitis (Mollaret meningitis)
The least common causes are :
- Behçet syndrome
- Central nervous system abscess
- Ehrlichiosis
- Human immunodeficiency virus
- Lyme disease (neuroborreliosis)
- Neurosyphilis
- Systemic lupus erythematous
- Tuberculous meningitis
- Vasculitis
Pathogenesis1
There is no exact hypothesis that explains the pathogenesis of meningitis. One hypothesis depends on Virchow-Robin space(VRS) as the following :
1. Nasopharyngeal colonization.
2. Penetration into the blood stream after crossing the mucosal membranes.
3. Proliferation of micro-organisms in the bloodstream
4. Extravasations across the endothelium of the post-capillary venules to the perivascular VRS.
5. Passage from VRS to subpial space
6. Moving through pia mater, infiltrating the CSF in the subarachnoid space
7. Invasion of the meninges .
Clinical features12 13 8
Presentation of meningitis has unique characterstics depending on the age group :
· Neonate/ infant is non-specific in its clinical presentation as in older patients , so infant will look ill with one or more of the following: loss of appetite, irritability, vomiting, hypotonia, apnea , grunting, bulging fontanelle and seizure. Neck stiffness is uncommon.
· Children: headache, fever, confusion, photophobia, nausea, vomiting, neck stiffness, irritability and seizure.
· Adults present with at least two of these four symptoms ; headache, fever, neck stiffness and altered mental status. Patient may have petechial rash from either pneumococcal or meningococcal meningitis.
· Patients older than 65 years of age may present with atypical presentation like non-specific confusion. Fever, headache and nuchal rigidity may not be present, moreover the Listeria monocytogenes is common in elderly patient.
Additionally, a good history is important to make a differential diagnosis17; that includes :
· Social history containing risk factors for sexually transmitted diseases.
· Immune status and vaccination history of all patients.
· Up to date medications are required because some medication groups (eg, IV immunoglobulin [IVIg], nonsteroidal anti-inflammatory medications) can lead to chronic meningitis.
· Travel history, vocational history.
· The presence of systemic symptoms or signs. including skin rash, joint pains, or mouth/genital ulcers, might sometimes provide diagnostic clues.
Complications14 may include seizures, Hydrocephalus, subdural collection, cerebral infarction, empyema, intracranial abscess, cranial nerve palsy , motor disability, intelligence quotient, sensorineural hearing loss, visual deficits and venous sinus thrombosis.
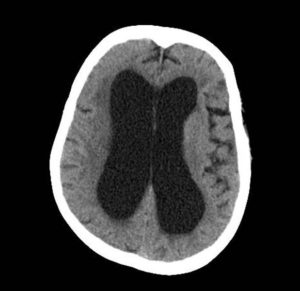
Figure 1 : hydrocephalus : Case courtesy of Radswiki, Radiopaedia.org.14
Physical Examination:
Classic physical examination maneuvers for the evaluation of meningitis that irritates the meningeal membrane are nuchal rigidity, Kernig’s sign and Brudzinski sign.
Kernig’s sign is performed with the patient supine in position with hips and knees in flexion, the patient’s knee is extended. Pain involving the hamstring muscles as a result of stretching the inflamed sciatic nerve roots at angles less than 135°, indicates a positive Kernig’s sign .20
Brudzinski’s sign is performed while the patient is in a supine position. The examiner, one hand behind the patient’s head and the other on their chest, elevates the patient’s head while the other hand prevents the patient from rising. If the patient does have meningitis, passive flexion of the neck is going to pull the nerve roots through the meninges, both of which are inflamed, causing pain and involuntary movement of lower extremities. Therefore, flexion of the patient’s hips and knees after passive flexion of the neck indicates a positive Brudzinski sign .20

Figure 2 : (a,b) : Kernig’s sign / (C) : Brudzinski’s sign 21
laboratory investigations 18 19
- Blood culture
Blood samples should be drawn for culture , and are useful before starting the antibiotics , because antibiotics have an influence on the diagnosis . Blood cultures are positive in 50–80% of bacterial meningitis cases . To determine the exact pathogen, require microscopic investigation with gram stain and acid fast stain .
2. Blood PCR : Higher sensitivity rate compared to blood culture. It also has an important advantage being that it detects bacteria after antibacterial agent is administrated .
Lumbar puncture (LP)19
Lumbar puncture is the confirmatory test for meningitis. Cell count in CSF indicates if there’s inflammation or not , the type of leukocytes help in determining the cause of meningitis; Lymphocyte predominance suggests viral, whereas neutrophil predominance suggests bacterial infection also observed in tuberculous meningitis.
In addition , biochemistry of CSF is also helpful in diagnosis ; Cerebrospinal fluid glucose is normally approximately two-thirds the plasma concentration , but It is lower in bacterial and tuberculous meningitis , so we should consider the plasma glucose when we approach lumbar puncture . Also , increased protein levels in CSF suggests inflammation . To determine the exact pathogen , require microscopic investigation with gram stain and acid fast stain. But one method with a higher sensitivity rate is CSF PCR , and its benefit is in patients who received antibiotics before LP .
TABLE 2. This table show parameters change with different pathogens.8 , 15
| Parameter | Normal | Bacterial | Viral | Tuberculous | Fungal |
| Opening presssure (cm CSF) | 12–20 | High | Normal or slightly raised | High | High |
| Appearance | Clear | Purulent | Clear | Clear /cloudy | Clear /cloudy |
| CSF WBC (cells/μL) | <5 | >100 | (5–1000) | (5–100) | (5–100) |
| Predominant cell | Neutrophils | Lymphocytes | Lymphocytes | Lymphocytes | |
| CSF protein | High | Slightly raised | High | High | |
| CSF Glucose level (mg/dL) | 50 to 80 | Usually <40 | Mostly normal | low glucose level (< 40 mg/dL) | normal or low |
| CSF to blood glucose ratio | >0.66 | Very low | Normal or slightly low | Very low | low |
Lumbar puncture contraindications:22
Contraindications were identified from many clinical research . The most important contraindications are:
1. If the patient has low platelet levels >20,000/mm3 to 50,000/mm3 or elevated international normalized ratio (INR) can be at risk of subarachnoid hemorrhage.
2. Presence of skin infection at the puncture site.
3. Congenital spine abnormalities (e.g., tethered cord), LP procedure can be guided by fluoroscopy, ultrasound, or CT.
4. Possible high intracranial pressure with brain herniation, in this case we should perform fundoscopy and CT/MRI Brain before LP. Significant clinical symptoms and signs for possible high intracranial pressure with brain herniation when a patient has focal neurological deficits, recent generalized seizures, abnormal level of consciousness, respiratory abnormalities, decorticate or decerebrate posturing, dilated or fixed pupil or papilledema at fundoscopy.
It’s also important to check medications before the procedure, like anticoagulant medications and if they can be temporarily discontinued or not.
 Figure 3 : Papilledema secondary to meningitis.23
Figure 3 : Papilledema secondary to meningitis.23
Treatment8 18 22 24
Patients with suspected acute bacterial meningitis need rapid diagnosis, empirical antimicrobial and early adjunctive therapy (high dose dexamethasone); strong inflammatory response has its negative sequelae hearing loss, deafness ,so adminstration of dexamethsone reduces the rate of occurance of these sequelae .
1. Consider precaution droplet.
2. Stabilization of the patient if they have breathing or circulatory difficulties.
3. Intravenously dexamethasone with dose of 2 x 0.4 mg/kg/24h or 4 x 8-12mg/24h (0.15 mg/kg every 6 h for infants and children): High dose of dexamethasone is given to reduces the mortality and morbidity rate of acute bacterial meningitis. For maximum benefit, dexamethasone must be given early (first dose should be adminstrated either shortly before or simultaneously with antibiotics).
4. Initiating empirical therapy; should begin therapy as soon as possible; delay may increase morbidity and mortality, such therapy should be initiated before CT brain if indicated. Recommended antibiotics are included in Table 3.
5. Once the causative pathogen is determined, the empirical therapy is stopped and patient is started on the specific antimicrobial agent. (Table 4)
Table 3. Recommended empirical antibiotics.
| Age and condition | Recommended therapy |
| Infant within 1st month | Ampicillin + cefotaxime |
| Age ( 2nd month – 50 year ) | Vancomycin + ceftriaxone |
| Age > 50 year or immunocompromised or alcoholics patient | Vancomycin + ceftriaxone + ampicillin |
| basilar skull fracture / cochlear implant | Vancomycin / ceftriaxone |
| penetrating trauma / post neurosurgery / Patients with cerebrospinal fluid shunt | Vancomycin + cefepime |
Table 4. Pathogen specific therapy
| Pathogen | Antibiotic | Duration of therapy (days) |
| Streptococcus pneumonia | Vancomycin + 3rd generation cephalosporin | 10 – 14 |
| Neisseria meningitidis | 3rd generation cephalosporin | 7 |
| Listeria monocytogenes | ampicillin or penicillin | >= 21 |
| Streptococcus agalactiae | ampicillin or penicillin | 14 – 21 |
| Haemophilus influenzae | 3rd generation cephalosporin | 7 |
| Escherichia coli | 3rd generation cephalosporin | 21 |
Viral meningitis requires supportive treatment only, acyclovir is not necessary unless the patient has impairment of consciousness, focal neurological signs and inflammation of temporal lobe in imaging Figure (4) ; because herpes encephalitis is suspected in this case, it should be treated with a high-dose of acyclovir for no fewer than 14 days and still will have about a 50% chance of permanent neurologic sequelae.
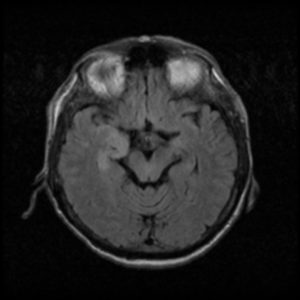
Figure 4 : Herpes simplex encephalitis, Case courtesy of RMH Core Conditions, Radiopaedia.25
Prevention26
Meningococcal vaccination is recommended for these groups:
· Infants aged 2 through 18 months.
· Persons aged 9 months until 55 years of age.
· Persons aged ≥56 years.
High risk situations that are recommended to get meningococcal vaccine:
· Who suffer from Persistent Complement Component Deficiencies (C3, C5-9, Properdin, Factor D, and Factor H).
· Anatomic or Functional Asplenia.
· Human Immunodeficiency Virus.
· Travelling to an epidemic country.
Table 5. Risk factors and the most common causative organism27
| Risk factor | Most common causative organism |
| Elderly > 65 years | S. pneumoniae, L. monocytogenes |
| Splenectomy / hyposplenic state | S. pneumoniae |
| Alcoholism | S. pneumoniae , L. monocytogenes |
| HIV/AIDS | S. pneumoniae, Salmonella spp |
| Diabetes mellitus | S. pneumoniae, L. monocytogenes |
| Cancer | S. pneumoniae, L. monocytogenes |
| Anatomical defect | S. pneumoniae |
| Organ transplant recipients | S. pneumonia, L. monocytogenes, Nocardia |
Prognosis:
Bacterial meningitis has a mortality rate of 14.8%.28
The mortality for each pathogen:
· S. pneumoniae is (16-37%).
· N. meningitidis is (5%).
· Haemophilus influenzae (3%).
And it is associated with bad outcomes as the following18 24 ;
· Focal neurological deficits occurs in 50% of cases
· Hearing impairment (14%); most common outcome.
· Moderate to severe disability (14%) .
· Cognitive impairments.
Viral meningitis is self- limiting, however in rare cases it is associated with long-term neuropsychiatric sequelae, particularly anxiety, depression and neurocognitive dysfunction.29
References:
1. Putz K, Hayani K, Zar FA. Meningitis. Prim Care. 2013;40(3):707-726. doi:10.1016/j.pop.2013.06.001
2. Cordeiro AP, Silva Pereira RA, Chapeaurouge A, et al. Comparative proteomics of cerebrospinal fluid reveals a predictive model for differential diagnosis of pneumococcal, meningococcal, and enteroviral meningitis, and novel putative therapeutic targets. BMC Genomics. 2015;16 Suppl 5(Suppl 5):S11. doi:10.1186/1471-2164-16-S5-S11
3. Davis LE. Acute Bacterial Meningitis. Continuum (Minneap Minn). 2018;24(5, Neuroinfectious Disease):1264-1283. doi:10.1212/CON.0000000000000660
4. Figueiredo AHA, Brouwer MC, van de Beek D. Acute Community-Acquired Bacterial Meningitis. Neurol Clin. 2018;36(4):809-820. doi:10.1016/j.ncl.2018.06.007
5. Tracy A, Waterfield T. How to use clinical signs of meningitis. Arch Dis Child – Educ &amp; Pract Ed. 2020;105(1):46 LP – 49. doi:10.1136/archdischild-2018-315428
6. McNeil HC, Jefferies JMC, Clarke SC. Vaccine preventable meningitis in Malaysia: epidemiology and management. Expert Rev Anti Infect Ther. 2015;13(6):705-714. doi:10.1586/14787210.2015.1033401
7. Hasbun R. Update and advances in community acquired bacterial meningitis. Curr Opin Infect Dis. 2019;32(3):233-238. doi:10.1097/QCO.0000000000000543
8. Mount HR, Boyle SD. Aseptic and Bacterial Meningitis: Evaluation, Treatment, and Prevention. Am Fam Physician. 2017;96(5):314-322.
9. Charalambous LT, Premji A, Tybout C, et al. Prevalence, healthcare resource utilization and overall burden of fungal meningitis in the United States. J Med Microbiol. 2018;67(2):215-227. doi:10.1099/jmm.0.000656
10. Shah I, Barot S, Madvariya M. Eosinophilic meningitis: a case series and review of literature of Angiostrongylus cantonensis and Gnathostoma spinigerum. Indian J Med Microbiol. 2015;33(1):154-158. doi:10.4103/0255-0857.148430
11. Chan P, Meerdink DJ, Uchizono JA. Potential role of the Virchow Robin space in the pathogenesis of bacterial meningitis. Med Hypotheses. 2017;109:114-118. doi:10.1016/j.mehy.2017.09.014
12. van de Beek D, de Gans J, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med. 2004;351(18):1849-1859. doi:10.1056/NEJMoa040845
13. Goldacre MJ. Neonatal meningitis. Postgrad Med J. 1977;53(624):607-609. doi:10.1136/pgmj.53.624.607
14. Wu H-M, Huang W-Y, Lee M-L, Yang AD, Chaou K-P, Hsieh L-Y. Clinical features, acute complications, and outcome of Salmonella meningitis in children under one year of age in Taiwan. BMC Infect Dis. 2011;11:30. doi:10.1186/1471-2334-11-30
15. radiopedia. hydrocephalus. https://radiopaedia.org/cases/meningitis-6?lang=us
16. radiopedia. hyrocephalus. https://radiopaedia.org/cases/hydrocephalus-1?lang=us
17. Thakur KT, Wilson MR. Chronic Meningitis. Continuum (Minneap Minn). 2018;24(5, Neuroinfectious Disease):1298-1326. doi:10.1212/CON.0000000000000664
18. Griffiths MJ, McGill F, Solomon T. Management of acute meningitis. Clin Med. 2018;18(2):164-169. doi:10.7861/clinmedicine.18-2-164
19. Alamarat Z, Hasbun R. Management of Acute Bacterial Meningitis in Children. Infect Drug Resist. 2020;13:4077-4089. doi:10.2147/IDR.S240162
20. Ward MA, Greenwood TM, Kumar DR, Mazza JJ, Yale SH. Josef Brudzinski and Vladimir Mikhailovich Kernig: signs for diagnosing meningitis. Clin Med Res. 2010;8(1):13-17. doi:10.3121/cmr.2010.862
21. kernigs and brudzisnki. https://annalsofian.org/article.asp?issn=0972-2327;year=2012;volume=15;issue=4;spage=287;epage=288;aulast=Mehndiratta;type=3
22. Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267-1284. doi:10.1086/425368
23. Papilledema secondary to meningitis. https://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/papilledema-secondary-to-meningitis/index.htm
24. Barichello T, Generoso JS, Collodel A, Moreira AP, Almeida SM de. Pathophysiology of acute meningitis caused by Streptococcus pneumoniae and adjunctive therapy approaches. Arq Neuropsiquiatr. 2012;70(5):366-372. doi:10.1590/s0004-282×2012000500011
25. radiopedia. Herpes simplex encephalitis. https://radiopaedia.org/cases/herpes-simplex-encephalitis-2?lang=gb
26. Cohn AC, MacNeil JR, Clark TA, et al. Prevention and control of meningococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm reports Morb Mortal Wkly report Recomm reports. 2013;62(RR-2):1-28.
27. Adriani KS, Brouwer MC, van de Beek D. Risk factors for community-acquired bacterial meningitis in adults. Neth J Med. 2015;73(2):53-60.
28. Thigpen MC, Whitney CG, Messonnier NE, et al. Bacterial meningitis in the United States, 1998-2007. N Engl J Med. 2011;364(21):2016-2025. doi:10.1056/NEJMoa1005384
29. McGill F, Griffiths MJ, Bonnett LJ, et al. Incidence, aetiology, and sequelae of viral meningitis in UK adults: a multicentre prospective observational cohort study. Lancet Infect Dis. 2018;18(9):992-1003. doi:10.1016/S1473-3099(18)30245-7




Very usefull, thank you Dr.Hashem.