Title: Brown Sequard Syndrome
Author: Zuhdi Badwan
Editor: Aseel Rabadi
Keywords: Brown Sequard Syndrome, incomplete spinal cord injury, spinal cord syndrome, Spine, neurosurgery.
-
History
Brown-Sequard syndrome (BSS) is classified as an incomplete spinal cord injury, where sensory and motor functions are not completely lost below the level of damage.
Brown-Sequard syndrome, named after the physiologist Charles-Edouard Brown-Séquard (1817–1894), was famous for his contributions to the fields of neurology and endocrinology[1]. He first published this condition in (1849) and discussed it later on other occasions: one was a case about a sea captain who developed the syndrome after getting stabbed in the neck. Also, in The Lancet (1869), he defined the syndrome as we know it today[1].
-
Epidemiology
There is no reliable estimate of the global prevalence or incidence of Brown-Sequard syndrome. However, spinal cord injuries, in general have a global incidence from 8 to 246 cases per million per year and a global prevalence from 236 to 1,298 cases per million per year[2]. Given that, the National Organization for Rare Diseases (NORD) estimated that around 2% of spinal cord injury cases are Brown-Sequard syndrome cases[3].
-
Etiology and pathogenesis
In The Lancet (1869): the physiologist Brown Sequard described his syndrome based on three findings: “A lesion in one of the lateral halves of the spinal cord that produces: firstly, paralysis of voluntary movements in the same side; secondly, anesthesia to touch, tickling, painful impressions, and changes of temperature in the opposite side; thirdly, paralysis of muscular senses in the same side”[1].

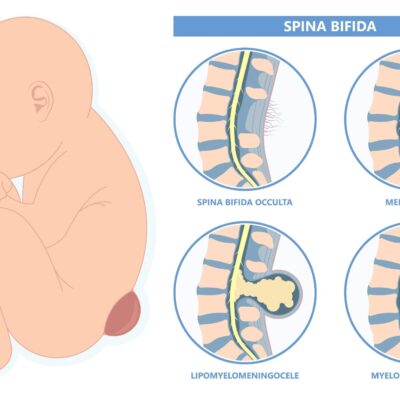
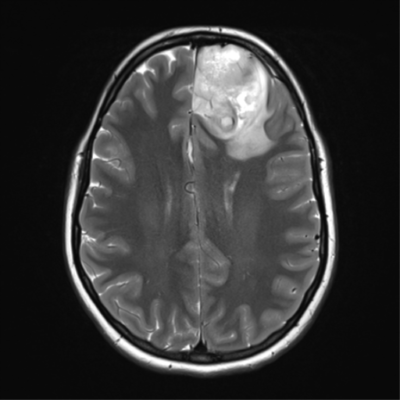
Figure 1: Features of Brown Sequard syndrome
In order to understand these findings, we have to take a look at the spinal cord: it has a lot of tracts, but BSS is only concerned with three of them: the spinothalamic tract, the lateral corticospinal tract, and the medial lemniscus tract.
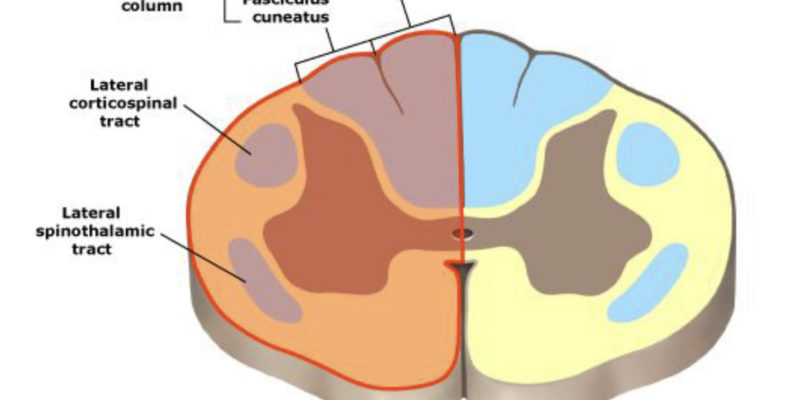
1. Spinothalamic tract:
The spinothalamic tract basically mediates the sensation of pain and temperature. Sensory modalities enter the cord via the dorsal root entry zone and synapse in the dorsal horn. At the level of synapses, the postsynaptic fibers directly cross to the opposite side. After that, they ascend within the anterolateral funiculus. These fibers continue to the thalamus to synapse with ventral posterolateral and intralaminar thalamic nuclei, continuing from the thalamic nuclei to the primary somatosensory cortex[4].
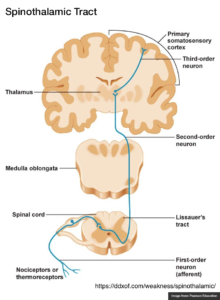
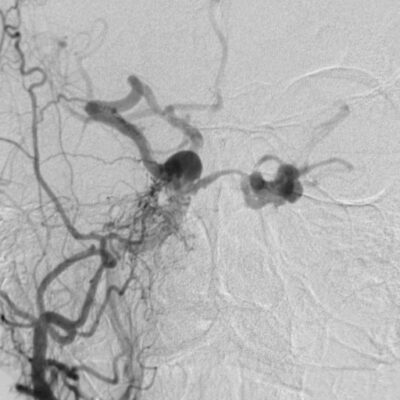
Figure 2: the spinothalamic tract.
2.Lateral corticospinal tract:
The lateral corticospinal tract on the other hand, mediates axial body and limb movements. It descends from the precentral motor cortex to decussate at the level of the lower medulla to the contralateral side. Then it continues down to synapse with neurons in the anterior gray horn at each ventral root. Lastly, the postsynaptic neurons exit via the ventral root to innervate the muscles[4].
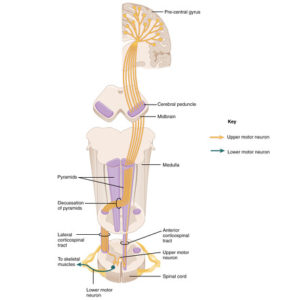
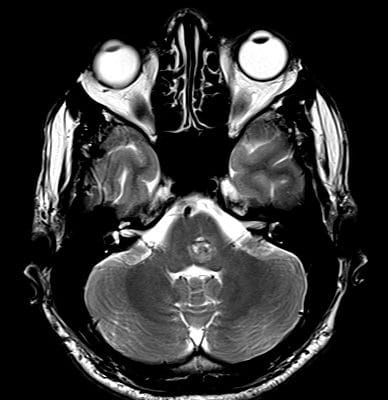
Figure 3: The lateral corticospinal tract.
3. Dorsal/Medial lemniscus tract:
The medial lemniscus tract mediates the sensations of vibration, proprioception (position sense), and 2-point discrimination from the skin and joints. Sensory modalities enter the spinal cord via the dorsal root. Nerve fibers ascend on the same side of their entry until they reach the gracile and cuneate nuclei in the lower medulla where they synapse. Postsynaptic fibers leave the nuclei and decussate to the contralateral side. Then travel upward to the ventral posterolateral thalamic nucleus to a new synapses point which eventually leads to the primary somatosensory cortex[4].
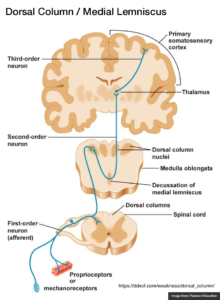
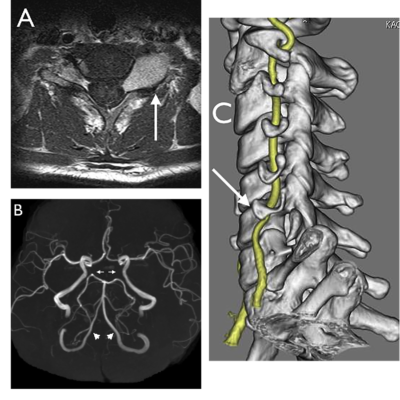
Figure 4: The medial lemniscus tract
To sum up, if the spinal cord is injured in a way that affects the three tracts on the same lateral half, the signal transmission is disrupted and as a result Brown Sequard syndrome will manifest accordingly.
Overall, three main mechanisms cause a spinal cord injury and can develop a case of Brown Sequard syndrome: First, direct physical damage causing physical spinal cord damage. Second, when the cord vascular supply is compromised causing ischemia. Third, due to spinal cord contusion and innate problems in the nervous tissue[5].
Most BSS cases are of a traumatic etiology: car accidents, violent acts (stabbing, gunshot, etc.), and falls. Non-traumatic causes are less prevalent but have many variations in the literature, like tumors, degenerative diseases, disk herniation, ischemia, inflammation or infections of the spinal cord, epidural hematoma, decompression sickness, cervical synovial cyst, and ruptured pheochromocytoma[5-8].
-
Diagnosis and Management
Diagnosis is reached based on extensive neurological clinical exams that show the features of BSS. In addition to MRI and CT imaging, other investigations such as spinal angiography and nuclear medicine can help identify vascular malformations and infectious or inflammatory causes.
BSS treatment can be conservative (medical treatment, physiotherapy, and rehabilitation) or surgical management, from which to choose depending on the patient’s neurological status and radiological findings.
Surgical interventions are necessary to reduce pressure on the spinal cord and increase its stability. For instance, in cases of traumatic injury, disc herniation, spinal hematoma to evacuate, or a foreign object or bony elements to remove. Used Surgical interventions include laminoplasty, laminectomy, and discectomy. Whilst medical management is chosen over surgical interventions in cases of infective, inflammatory, or demyelinating causes of BSS. Corticosteroids, antibiotics, antispasmodics, and analgesics are often used[9-12].
-
Complications
Published literature didn’t point out specific complications following BSS. However, spinal cord injuries collectively have certain complications which can involve many systems and they largely depend on the location of the injury. For example:
- Cardiovascular complications are the most common cause of death in SCI. Manifest mainly as a neurogenic shock. A neurogenic shock: involves bradycardia and hypotension, it happens due to loss of sympathetic drive because of injuries at T6 vertebrae level and above.
- Pulmonary complications are the most common complications in SCI. Including Diaphragmatic and intercostal muscles dysfunctions, caused by injuries at T1 vertebrae level and above. Whereas injuries at C3 vertebrae level and above are more severe and could lead to diaphragmatic paralysis. Additional pulmonary complications include pneumonia, pulmonary embolism, pleural effusion, pneumothorax, and mucus plug.
- Gastrointestinal Complications include ileus, constipation, pancreatitis, abdominal rigidity, and stress ulceration.
- Genitourinary Complications include neurogenic bladder and urinary tract infections.
- Autonomic dysreflexia happens due to an injury in high thoracic and cervical levels. Opposite to what happens in a neurogenic shock: the lesion blocks sympathetic inhibitory outflow which leads to a sympathetic overdrive, that causes cardiac, bladder, bowel, temperature, and sexual dysfunctions[13].
-
Prognosis
BSS demonstrates a bright prognosis after rehabilitation. Shortly after it, patients can independently perform functional skills at discharge and could even regain employment.
It is important to mention that patients with predominant upper limb weakness show better outcomes than those with predominant lower limb weakness. Also, BSS has a better prognosis than all of the other spinal cord injuries[14,15].